Cindy Johnson holds a painting of her husband, Steven, a retired pharmacist who had survived colon cancer and took meticulous measures to avoid contracting covid-19. Steven died of covid in December 2020, and Cindy believes he contracted the virus at Blake Medical Center in Bradenton, Florida, where he was admitted for an infection in his hip. (EVE EDELHEIT FOR KHN)
This is a republication of the article below, under the title above, with focus on the mortality rate for hospital acquired covid patients.
Patients Went Into the Hospital for Care. After Testing Positive There for Covid, Some Never Came Out.
Kaiser Health News
By Christina Jewett, with Lauren Weber
NOVEMBER 4, 2021
Key message (by the editor of the blog):
More than 10,000 patients were diagnosed with covid in a U.S. hospital last year after they were admitted for something else;
Yet in the scheme of things that can go wrong in a hospital, it is catastrophic:
- About 21% of the patients who contracted covid in the hospital from April to September last year died, the data shows.
- In contrast, nearly 8% of other Medicare patients died in the hospital at the time.
A KHN review of work-safety records, medical literature and interviews with staff at high-spread hospitals points to why the virus took hold:
- Hospital leaders were slow to appreciate its airborne nature, which made coughing patients hazardous to roommates and staff members, who often wore less-protective surgical masks instead of N95s.
- Hospitals failed to test every admitted patient, enabled by CDC guidance that leaves such testing to the “discretion of the facility.”
- Management often failed to inform workers when they’d been exposed to covid and so were at risk of spreading it themselves.
Overall, the rate of in-hospital spread among Medicare and other patients was lower than in other countries, including the United Kingdom, which makes such data public and openly discusses it.
LONG READ
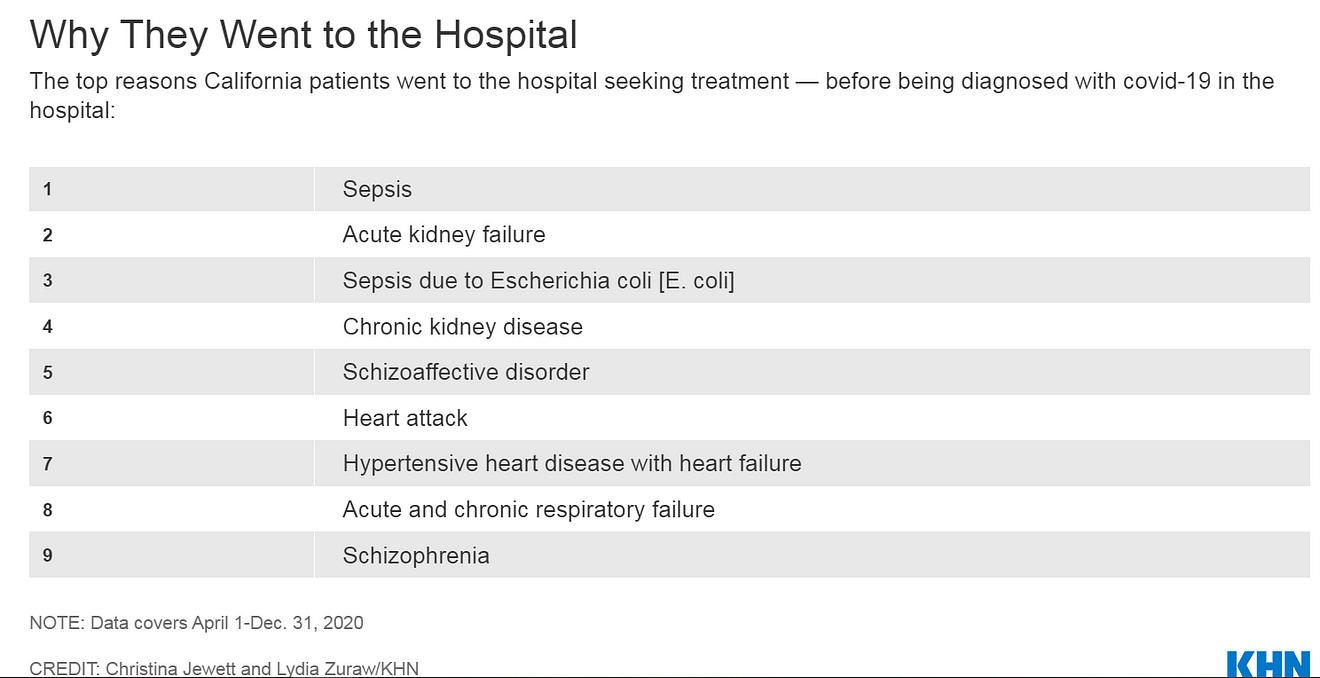
They went into hospitals with heart attacks, kidney failure or in a psychiatric crisis.
They left with covid-19 — if they left at all.
More than 10,000 patients were diagnosed with covid in a U.S. hospital last year after they were admitted for something else, according to federal and state records analyzed exclusively for KHN.
The number is certainly an undercount, since it includes mostly patients 65 and older, plus California and Florida patients of all ages.
Yet in the scheme of things that can go wrong in a hospital, it is catastrophic:
- About 21% of the patients who contracted covid in the hospital from April to September last year died, the data shows.
- In contrast, nearly 8% of other Medicare patients died in the hospital at the time.

Steven Johnson, 66, was expecting to get an infection cut out of his hip flesh and bone at Blake Medical Center in Bradenton, Florida, last November. The retired pharmacist had survived colon cancer and was meticulous to avoid contracting covid.
He could not have known that, from April through September, 8% of that hospital’s Medicare covid patients were diagnosed with the virus after they were admitted for another concern.
Johnson had tested negative for covid two days before he was admitted. After 13 days in the hospital, he tested positive, said his wife, Cindy Johnson, also a retired pharmacist.
Soon he was struggling to clear a glue-like phlegm from his lungs. A medical team could hardly control his pain. They prompted Cindy to share his final wishes. She asked: “Honey, do you want to be intubated?” He responded with an emphatic “no.” He died three days later.
After her husband tested positive, Cindy Johnson, trained in contact tracing, quickly got a covid test. She tested negative.
Then she thought about the large number of hospital staffers flowing into and out of his room — where he was often unmasked — and suspected a staff member had infected him.
That the hospital, part of the HCA Healthcare chain, still has not mandated staff vaccinations is “appalling,” she said.
“I’m furious,” she said.
“How can they say on their website,” she asked, “that the safety precautions ‘we’ve put into place make our facilities among the safest possible places to receive healthcare at this time’?”
Blake Medical Center spokesperson Lisa Kirkland said the hospital is “strongly encouraging vaccination” and noted that it follows Centers for Disease Control and Prevention and federal and state guidelines to protect patients.
President Joe Biden has called for all hospital employees to be vaccinated, but the requirement could face resistance in a dozen states, including Florida, that have banned vaccine mandates.

Johnson holds a pillow made from a shirt her husband, Steven, used to wear.(EVE EDELHEIT FOR KHN)
Overall, the rate of in-hospital spread among Medicare and other patients was lower than in other countries, including the United Kingdom, which makes such data public and openly discusses it.
The … United Kingdom, makes such data public and openly discusses it (the rate of in-hospital spread)
On average, about 1.7% of U.S. hospitalized covid patients were diagnosed with the virus in U.S. hospitals, according to an analysis of Medicare records from April 1 to Sept. 30, 2020, provided by Dr. James Kennedy, founder of CDIMD, a Nashville-based consulting and data analytics company.
Yet the rate of infection was far higher in 38 hospitals where 5% or more of the Medicare covid cases were documented as hospital-acquired.
The data is from a challenging stretch last year when protective gear was in short supply and tests were scarce or slow to produce results.
The Medicare data for the fourth quarter of 2020 and this year isn’t available yet, and the state data reflects April 1 through Dec. 31, 2020.
A KHN review of work-safety records, medical literature and interviews with staff at high-spread hospitals points to why the virus took hold:
- Hospital leaders were slow to appreciate its airborne nature, which made coughing patients hazardous to roommates and staff members, who often wore less-protective surgical masks instead of N95s.
- Hospitals failed to test every admitted patient, enabled by CDC guidance that leaves such testing to the “discretion of the facility.”
- Management often failed to inform workers when they’d been exposed to covid and so were at risk of spreading it themselves.
Spread among patients and staffers seemed to go hand in hand.
At Beaumont Hospital, Taylor, in Michigan, 139 employee covid infections were logged between April 6 to Oct. 20 last year, a hospital inspection report shows.
Nearly 7% of the Medicare patients with covid tested positive after they were admitted to that hospital for something else, the federal data shows.
A hospital spokesperson said tests were not available to screen all patients last year, resulting in some late diagnoses. He said all incoming patients are tested now.
Tracking covid inside health facilities is no new task to federal officials, who publicly report new staff and resident cases weekly for each U.S. nursing home.
Yet the Department of Health and Human Services reports data on covid’s spread in hospitals only on a statewide basis, so patients are in the dark about which facilities have cases.
KHN commissioned analyses of hospital billing records, which are also used more broadly to spot various hospital-acquired infections.
For covid, the data has limitations. It can pick up some community-acquired cases that were slow to show up, as it can take two to 14 days from exposure to the virus for symptoms to appear, with the average being four to five days.
The records do not account for cases picked up in an emergency room or diagnosed after a hospital patient was discharged.

Linda Moore, 71, tested positive at least 15 days into a hospital stay for spinal surgery, according to her daughter Trisha Tavolazzi.
Her mother was at Havasu Regional Medical Center in Lake Havasu City, Arizona, which did not have a higher-than-average rate of internal spread last summer.
The hospital implemented “rigorous health and safety protocols to protect all of our patients” during the pandemic, said hospital spokesperson Corey Santoriello, who would not comment on Moore’s case, citing privacy laws.
Moore was airlifted to another hospital, where her condition only declined further, her daughter said. After the ventilator was removed, she clung to life fitfully for 5½ hours, as her daughter prayed for her mother to find her way to heaven.
“I asked her mom and her dad and her family and prayed to God, ‘Please just come show her the way,’” Tavolazzi said. “I relive it every day.”
When Tavolazzi sought answers from the hospital about where her mom got the virus, she said, she got none: “No one ever called me back.”
Two Negative Covid Tests, Then ‘Patient Zero’
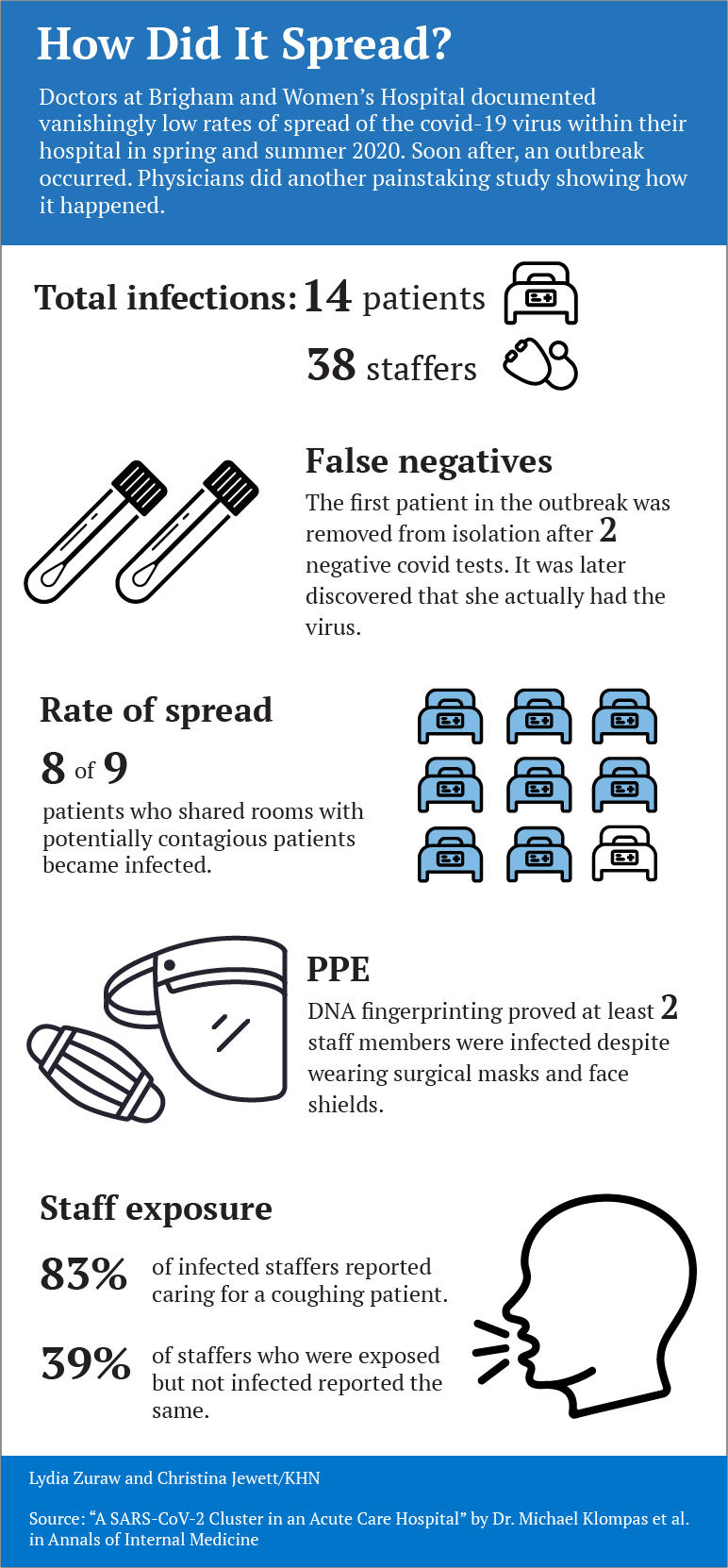
As the second surge of covid subsided last September, doctors from the prestigious Brigham and Women’s Hospital published a reassuring study:
With careful infection control, only two of 697 covid patients acquired the virus within the Boston hospital.
That is about 0.3% of patients ― about six times lower than the overall Medicare rate.
Brigham tested every patient it admitted, exceeding CDC recommendations. It was transparent and open about safety concerns.
But the study, published in the high-profile JAMA Network Open journal, conveyed the wrong message, according to Dr. Manoj Jain, an infectious-disease physician and adjunct professor at the Rollins School of Public Health at Emory University.
Covid was spreading in hospitals, he said, and the study buried “the problem under the rug.”
Before the virtual ink on the study was dry, the virus began a stealthy streak through the elite hospital.
It slipped in with a patient who tested negative twice ― but turned out to be positive. She was “patient zero” in an outbreak affecting 38 staffers and 14 patients, according to a study in Annals of Internal Medicine initially published Feb. 9.
That study ‘s authors sequenced the genome of the virus to confirm which cases were related ― and precisely how it traveled through the hospital.
As patients were moved from room to room in the early days of the outbreak, covid spread among roommates 8 out of 9 times, likely through aerosol transmission, the study says.
A survey of staff members revealed that those caring for coughing patients were more likely to get sick.
The virus also appeared to have breached the CDC-OK’d protective gear. Two staff members who had close patient contact while wearing a surgical mask and face shield still wound up infected.
The findings suggested that more-protective N95 respirators could help safeguard staff.
Brigham and Women’s now tests every patient upon admission and again soon after.
Nurses are encouraged to test again if they see a subtle sign of covid, said Dr. Erica Shenoy, associate chief of the Infection Control Unit at Massachusetts General Hospital, who helped craft policy at Brigham.
She said nurses and environmental services workers are at the table for policymaking: “I personally make it a point to say, ‘Tell me what you’re thinking,’” Shenoy said. “‘There’s no retribution because we need to know.’”
CDC guidelines, though, left wide latitude on protective gear and testing. To this day, Shenoy said, hospitals employ a wide range of policies.
The CDC said in a statement that its guidelines “provide a comprehensive and layered approach to preventing transmission of SARS-CoV-2 in healthcare settings,” and include testing patients with “even mild symptoms” or recent exposure to someone with covid.
Infection control policies are rarely apparent to patients or visitors, beyond whether they’re asked to wear a mask.
But reviews of public records and interviews with more than a dozen people show that at hospitals with high rates of covid spread, staff members were often alarmed by the lack of safety practices.
Nurses Sound the Alarm on Covid Spread
As covid crept into Florida in spring 2020, nurse Victoria Holland clashed with managers at Blake Medical Center in Bradenton, where Steven Johnson died.
She said managers suspended her early in the pandemic after taking part in a protest and “having a hissy fit” when she was denied a new N95 respirator before an “aerosol-generating” procedure.
The CDC warns that such procedures can spread the virus through the air. Before the pandemic, nurses were trained to dispose of an N95 after each patient encounter.
When the suspension was over, Holland said, she felt unsafe. “They told us nothing,” she said. “It was all a little whisper between the doctors.
You had potential covids and you’d get a little surgical mask because [they didn’t] want to waste” an N95 unless they knew the patient was positive.
Holland said she quit in mid-April. Her nursing colleagues lodged a complaint with the Occupational Safety and Health Administration in late June alleging that staff “working around possible Covid-19 positive cases” had been denied PPE.
Staff members protested outside the hospital in July and filed another OSHA complaint that said the hospital was allowing covid-exposed employees to keep working.
Kirkland, the Blake spokesperson, said the hospital responded to OSHA and “no deficiencies were identified.”
The Medicare analysis shows that 22 of 273 patients with covid, or 8%, were diagnosed with the virus after they were admitted to Blake.
That’s about five times as high as the national average.
Kirkland said “there is no standard way for measuring COVID-19 hospital-associated transmissions” and “there is no evidence to suggest the risk of transmission at Blake Medical Center is different than what you would find at other hospitals.”
In Washington, D.C., 34 Medicare covid patients contracted the virus at MedStar Washington Hospital Center, or nearly 6% of its total, the analysis shows.
Unhappy with the safety practices ― which included gas sterilization and reuse of N95s — National Nurses United members protested on the hospital lawn in July 2020.
At the protest, nurse Zoe Bendixen said one nurse had died of the virus and 50 had gotten sick: “[Nurses] can become a source for spreading the disease to other patients, co-workers and family members.”
Nurse Yuhana Gidey said she caught covid after treating a patient who turned out to be infected. Another nurse ― not managers doing contact tracing ― told her she’d been exposed, she said.
Nurse Kimberly Walsh said in an interview there was an outbreak in a geriatric unit where she worked in September 2020. She said management blamed nurses for bringing the virus into the unit. But Walsh pointed to another problem: The hospital wasn’t covid-testing patients coming in from nursing homes, where spread was rampant last year.
MedStar declined a request for an interview about its infection control practices and did not respond to specific questions.
While hospitals must track and publicly report rates of persistent infections like C. diff, antibiotic-resistant staph and surgical site infections, similar hospital-acquired covid rates are not reported.
KHN examined a different source of data that Congress required hospitals to document about “hospital-acquired conditions.”
The Medicare data, which notes whether each covid case was “present on admission” or not, becomes available months after a hospitalization in obscure files that require a data-use agreement typically granted to researchers.
KHN counted cases, as federal officials do, in some instances in which the documentation is deemed insufficient to categorize a case (see data methodology, below).
For this data, whether to deem a covid case hospital-acquired lies with medical coders who review doctors’ notes and discharge summaries and ask doctors questions if the status is unclear, said Sue Bowman, senior director of coding policy and compliance at American Health Information Management Association.
She said medical coders are aware that the data is used for hospital quality measures and would be careful to review the contact tracing or other information in the medical record.
If a case was in the data KHN used, “that would mean it was acquired during the hospital stay either from a health care worker or another patient or maybe if a hospital allowed visitors, from a visitor,” Bowman said. “That would be a fair interpretation of the data.”
The high death rate for those diagnosed with covid during a hospital stay — about 21% — mirrors the death rate for other Medicare covid patients last year, when doctors had few proven methods to help patients.
It also highlights the hazard unvaccinated staffers pose to patients, said Jain, the infectious-disease doctor.
The American Hospital Association estimates that about 42% of U.S. hospitals have mandated that all staff members be vaccinated.
“We don’t need [unvaccinated staff] to be a threat to patients,” Jain said. “[Hospital] administration is too afraid to push the nursing staff, and the general public is clueless at what a threat a non-vaccinated person poses to a vulnerable population.”

Cindy Johnson said the hospital where she believes her husband contracted covid faced minimal scrutiny in a state inspection, even after she said she reported that he caught covid there. She explored suing, but an attorney told her it would be nearly impossible to win such a case. A 2021 state law requires proof of “at least gross negligence” to prevail in court.
Johnson did ask a doctor who sees patients at the hospital for this: Please take down the big “OPEN & SAFE” sign outside.
Within days, the sign was gone.
KHN Midwest correspondent Lauren Weber contributed to this report.
Originally published at https://khn.org on November 4, 2021.