Health & Care Transformation Institute (HCTI)
research institute, knowledge portal and
advisory consulting
Joaquim Cardoso MSc*
Founder, and Chief Researcher & Editor
December 1, 2022
MSc* from London Business School
MIT Sloan Masters Program
Senior Advisor for Health & Care Transformation , and Digital Health
Executive Summary
Things are once again going in the wrong direction in the United States.
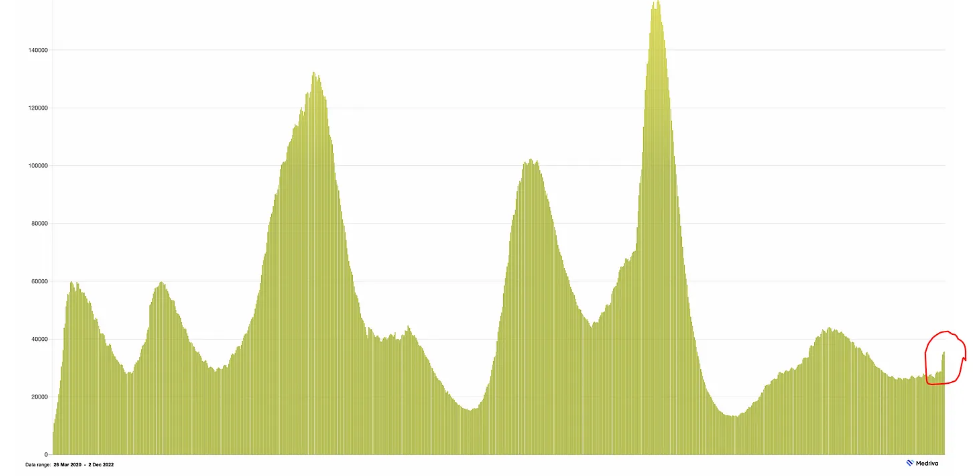
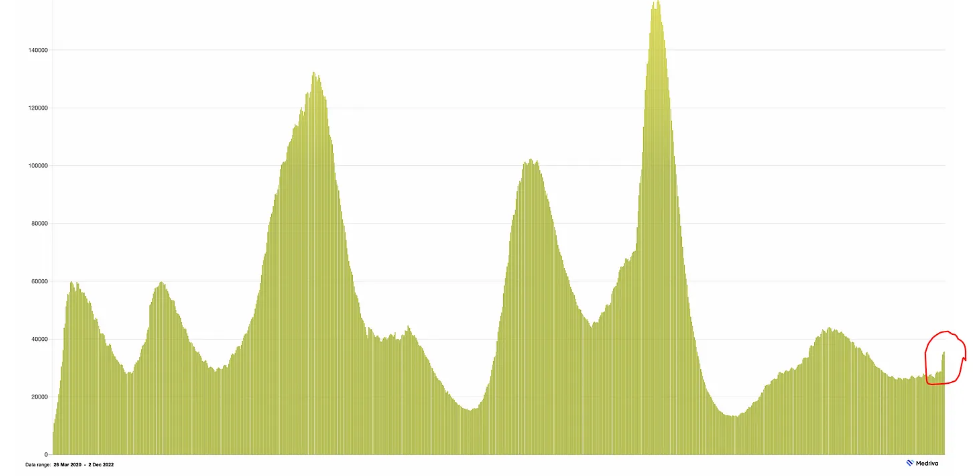
- Hospitalizations have jumped by 25% in recent days, along with ICUs, test positivity, wastewater surveillance virus levels, and even cases, which have been grossly under-diagnosed because of rapid antigen testing or no testing.
- Seniors, particularly those without a booster or one in the past 6 months, are bearing most of the brunt with the sharp ascent seen below, already surpassing the summer BA.5 wave nationally.
- The increase in hospital admits is also seen for age 50+ and all ages, yet not as sharp.
- The unvaccinated are part of this, too, but recent CDC data and the Kaiser Family Foundation analysis demonstrated that, with most seniors having at 2 shots, more of the deaths in recent months are among those without a booster shot.
There are a few reasons why this is happening again.
- 1.Immunity waning
- 2.Abandonment of mitigation measures, colder weather, indoor and holiday gatherings
- 3.The rise of the BQ.1.1 variant
- 4.Low Use of Paxlovid
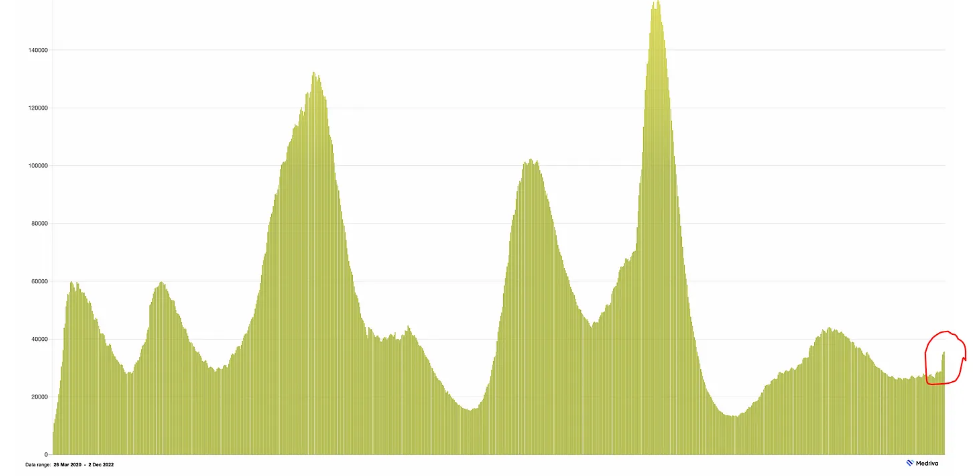
The wave is not just in the United States
- Europe is seeing a similar pattern as seen in many countries using weekly hospital admissions that are up diffusely (countries with data provided by Our World in Data) and most recent BQ.1.1 percentages by cov-spectrum.org
- Like the US, except for France (which has the highest hospital admissions per capita) BQ.1.1 has not yet reached dominance (50%+).
The pandemic is far from over: Asia
- Besides what is happening in Europe, and the well-publicized situation in China where the Zero-Covid policy worked well until containment of Omicron became impossible, there is a new wave in Asia developing that includes Japan, Australia, Hong Kong and South Korea
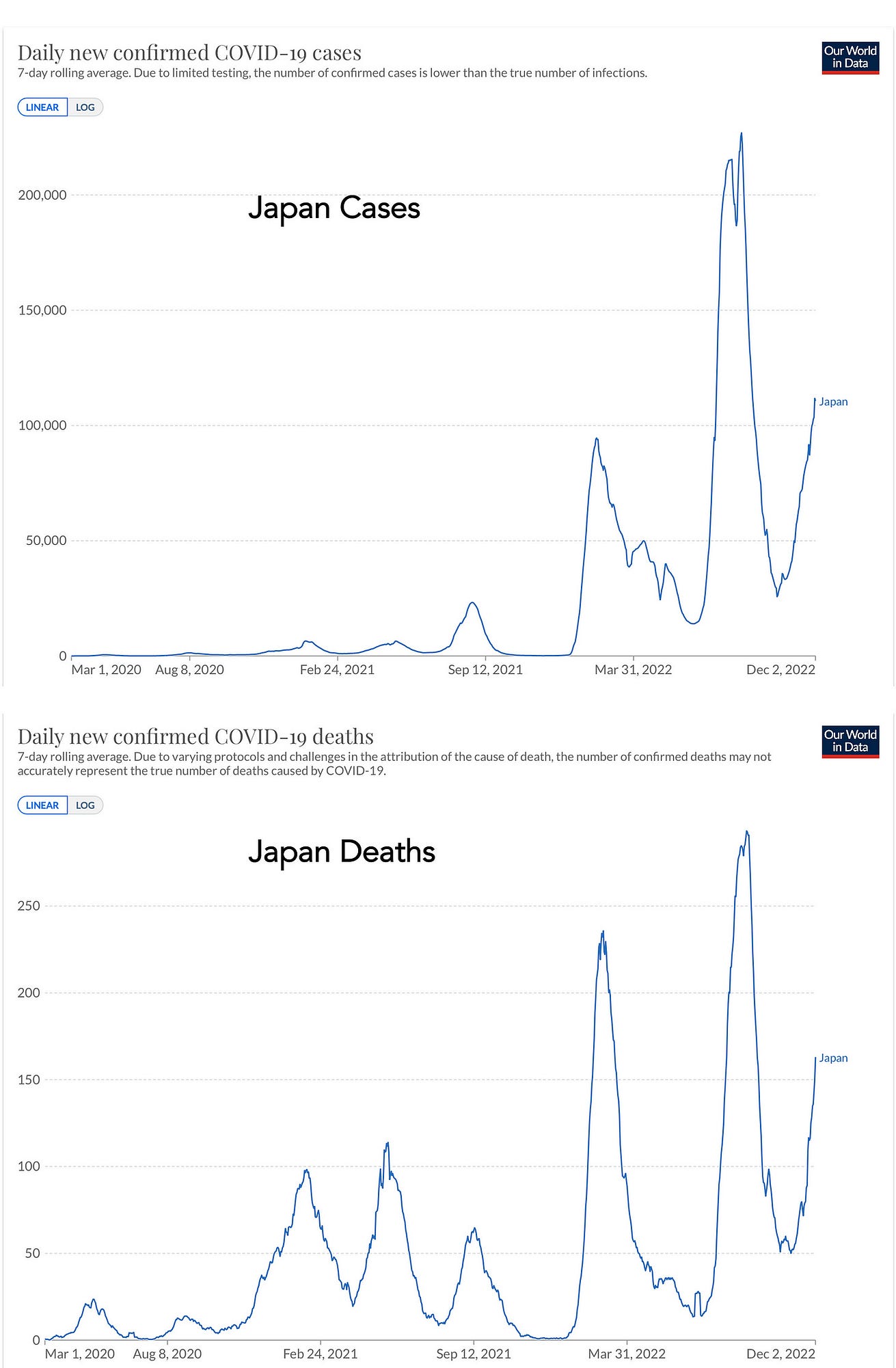
- Japan is especially noteworthy because it is experiencing a large and second BA.5 wave (perhaps due to newer subvariants of BA.5 not yet delineated). Japan’s management of the pandemic has been exemplary with an enviable balance of avoiding full lockdowns, use of masks and mitigation, “cluster-busting”and high uptake of vaccinations/boosters.
- But, there are an average of 120,000 new cases per day and deaths are, in parallel, on the rise, steeply.
- The fact that Australia and New Zealand are involved in the new Asian-Pacific wave takes us out of the northern hemisphere and winter/ cold weather as a principal driver.
- Yes, South America, too.
What’s Next?
- The hope is that we’ll not see a major wave in the weeks ahead, but there’s lots of uncertainty, especially in the United States.
- We’ve had a heck of a lot of Covid infections, and reinfections, that together with vaccinations and boosters have built a fairly formidable immunity wall (albeit perhaps less formidable than many countries in Europe, and for a different reason Japan, South Korea, Australia, New Zealand, Singapore, Taiwan and others with their much higher vaccination/booster rates).
- Accordingly, just as Singapore largely withstood the XBB variant challenge well, we/globally should be able to handle BQ.1.1.
- And we may well be facing XBB or other Omicron BA.2/BA.5 mutation-laden descendants after the BQ.1.1 wave is finished.
The main point is that we’re not doing what we can do reduce the toll of the virus.
- That means for everyone (especially age 50+) getting a booster and using mitigation measures appropriately.
- It also means we’re poorly equipped to ever keep up with the virus, no less get ahead of it, having lost the power of monoclonal antibodies as a backstop and for the immunocompromised.
- This represents a do nothing posture and extends to not aggressively going after nasal vaccines and pan-β-coronavirus vaccines.
- The idea that current boosters could be used and effective on an annual basis is balderdash, given their durability is less than 6 months.
The recent extraordinary success of a pan-influenza vaccine, across all Influenza A and B lineages, and effective in experimental models, for the first time, should markedly bolster our confidence for developing one against SARS-CoV-2, a much easier target than influenza.
- But we’re not doing that.
- All part of a complacency syndrome, …
- And there is still looming the potential that we will get “Omicron-ized” with a whole new, antigenically distinct family of variants (say Pi or Sigma) in the months or years ahead that we’re not prepared for, but certainly could be.
Whatever happens in the current Covid wave, and it certainly will not be as as bad the initial Omicron BA.1 or Delta waves, I know we in the US could do far better.
- At some point an aggressive push for better vaccines, new antibodies and pills to replace or combine with Paxlovid will all get done.
- The question is why do we have to wait for the urgent, reactive need when all of that can be anticipated.
The question is why do we have to wait for the urgent, reactive need when all of that can be anticipated.
Infographic

ORIGINAL PUBLICATION (full version)
The new Covid wave
It’s across most of the planet now. Delving into why, what to expect, and what we can do about it.
Eric Topol
December 3, 2022
Things are once again going in the wrong direction in the United States.
Hospitalizations have jumped by 25% in recent days, along with ICUs, test positivity, wastewater surveillance virus levels, and even cases, which have been grossly under-diagnosed because of rapid antigen testing or no testing.
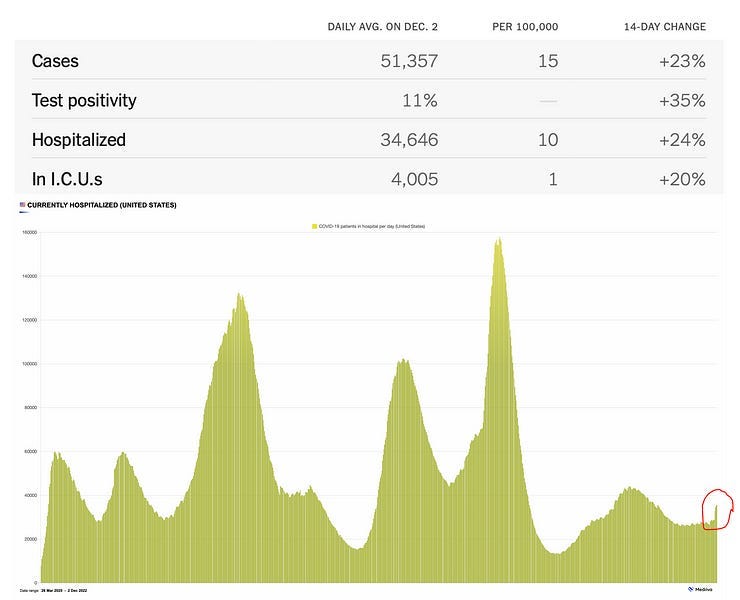
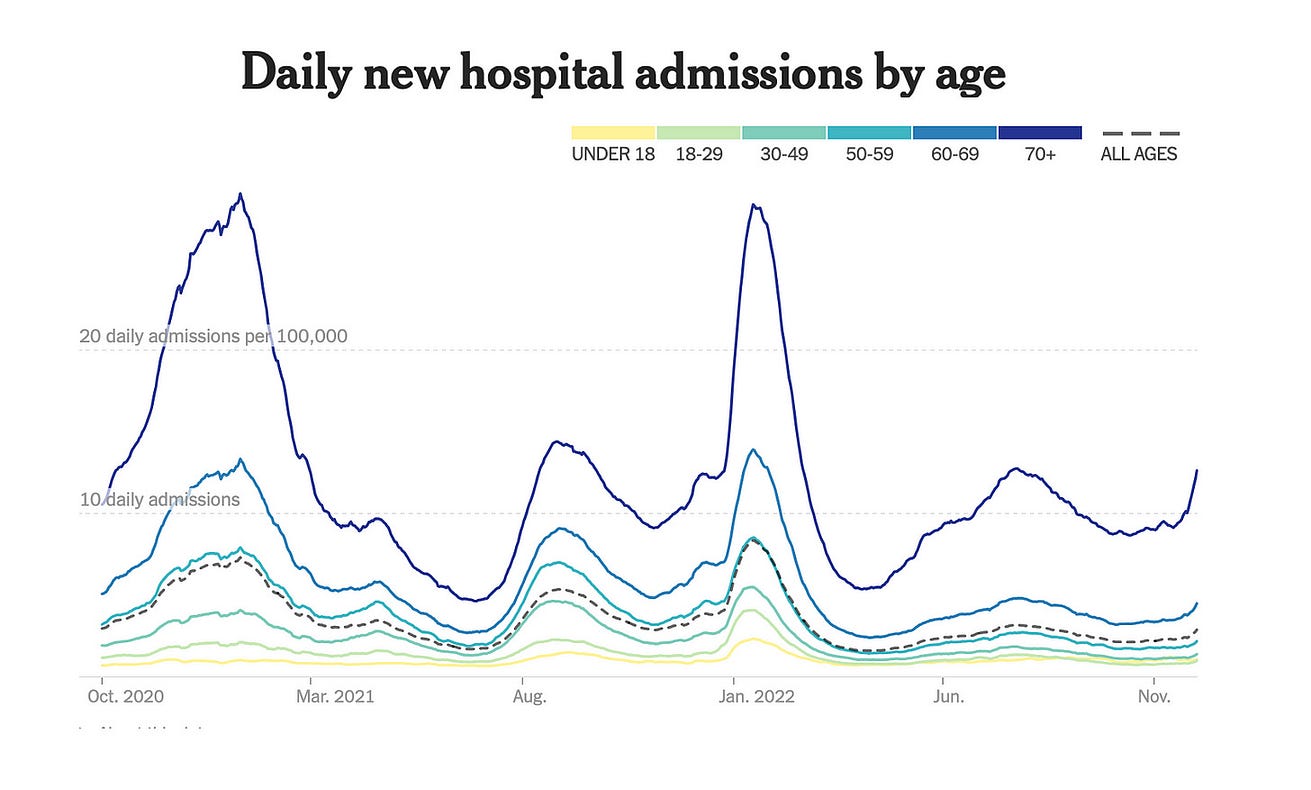
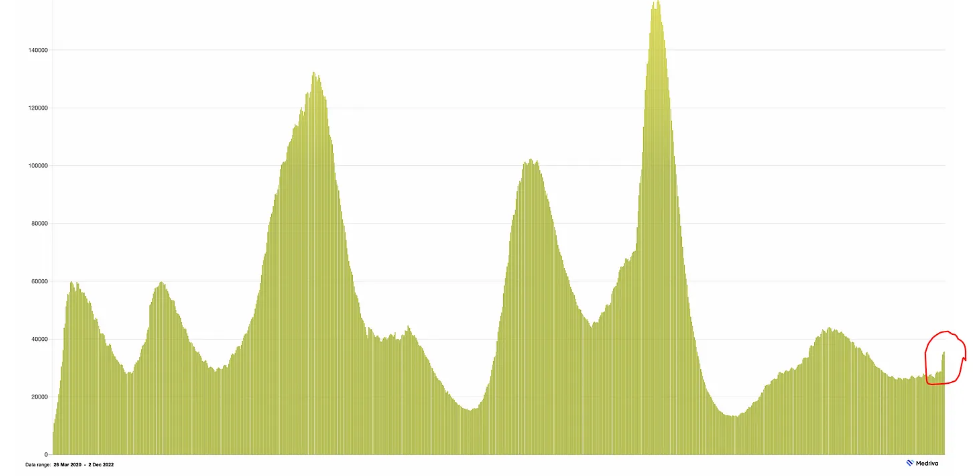
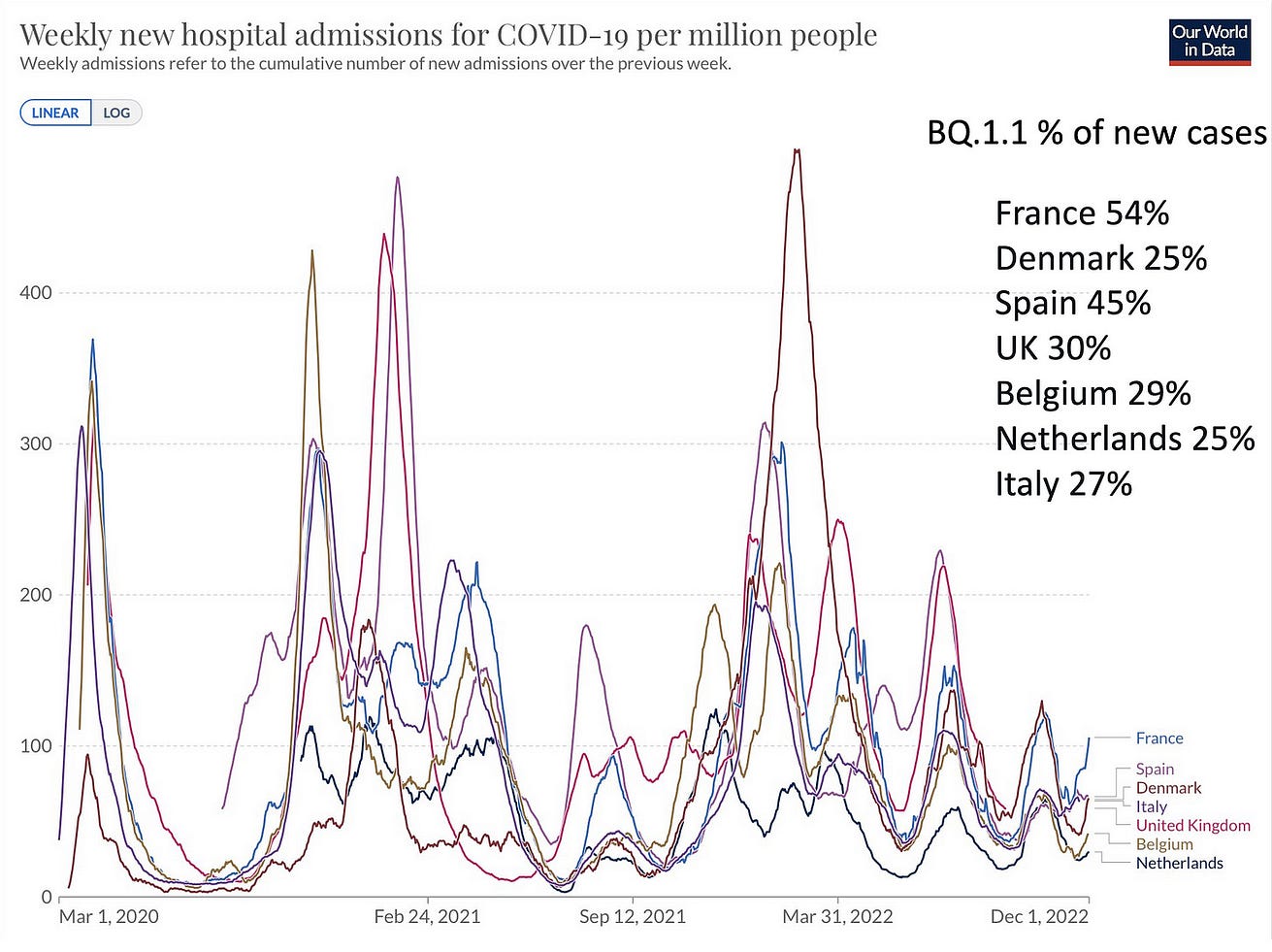
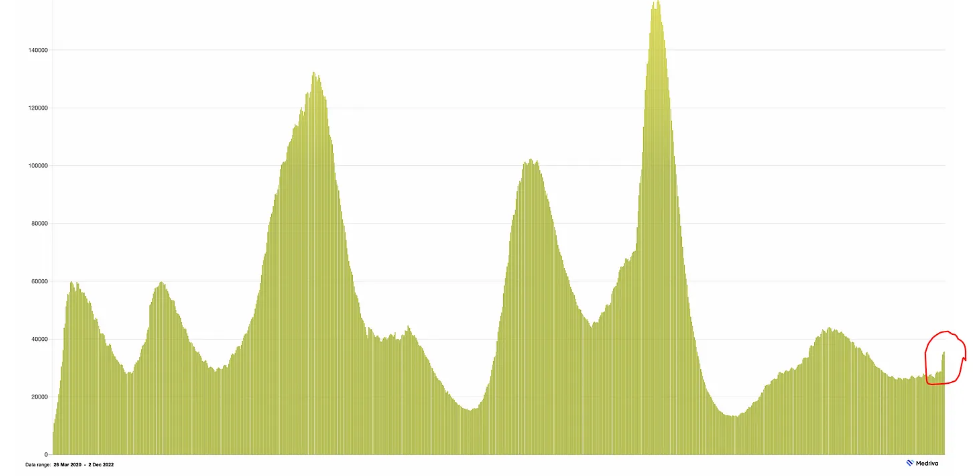
Seniors, particularly those without a booster or one in the past 6 months, are bearing most of the brunt with the sharp ascent seen below, already surpassing the summer BA.5 wave nationally.
The increase in hospital admits is also seen for age 50+ and all ages, yet not as sharp.
The unvaccinated are part of this, too, but recent CDC data and the Kaiser Family Foundation analysis demonstrated that, with most seniors having at 2 shots, more of the deaths in recent months are among those without a booster shot.
The unvaccinated are part of this, too, but recent CDC data and the Kaiser Family Foundation analysis demonstrated that, with most seniors having at 2 shots, more of the deaths in recent months are among those without a booster shot.
There are a few reasons why this is happening again.
- 1.Immunity waning
- 2.Abandonment of mitigation measures, colder weather, indoor and holiday gatherings
- 3.The rise of the BQ.1.1 variant
- 4.Low Use of Paxlovid
1.Immunity waning
On December 2nd, the CDC posted updated data for 2 booster shots vs unvaccinated against hospitalizations through September (BA.5 wave). The graphs below are for age 18+ at left and age 65+ at right. In the month of September, there was ~80% reduction of Covid hospitalizations for people with 2 boosters compared with unvaccinated- across all age groups-with a much higher absolute reduction for seniors, as noted by the change in Y-axis on the right panel.
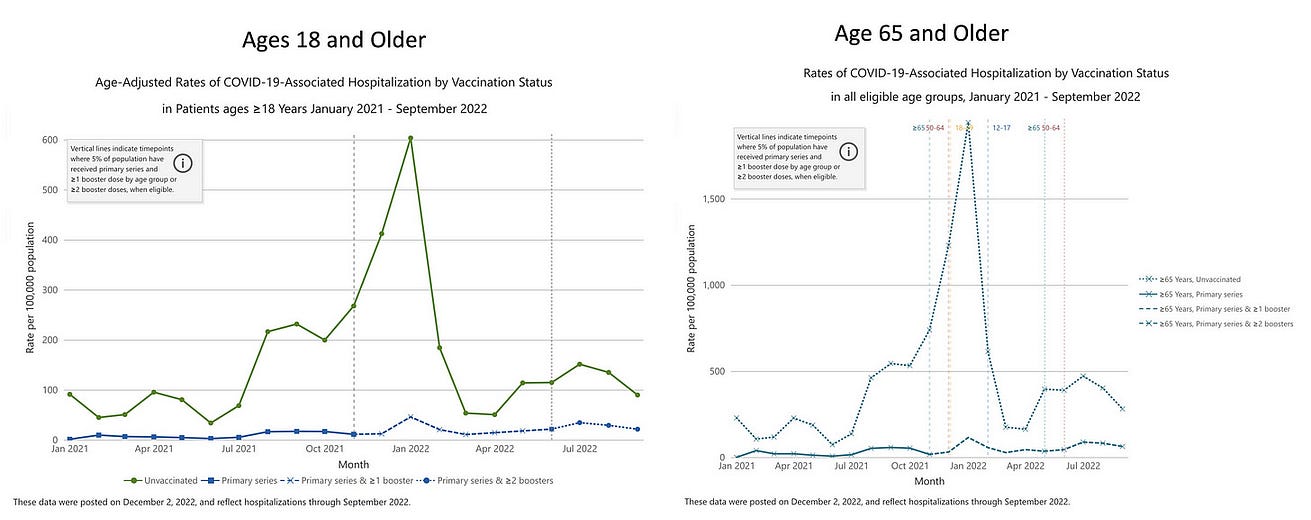
It’s quite simple. You want to avoid severe Covid and hospitalization, you need a booster within the past 4–6 months. The boosters won’t do too much to block infections but are holding up well for preventing hospitalizations. Unfortunately, our weak CDC continues to define “fully vaccinated” as 2 shots. I’ve had 5 shots, like many of you. That’s fully vaccinated. It’s frankly hard to believe that, with all the billions of dollars devoted to our public health agencies, they can’t even get such a straightforward message and fact out as what it means to be “fully vaccinated.”
2.Abandonment of mitigation measures, colder weather, indoor and holiday gatherings
Masking has largely been abandoned. When I go to the grocery store these days wearing a KN95 mask, people look at me like I’m a weirdo. We’ve just gotten through the Thanksgiving holiday and are about to go through far more holiday indoor gatherings. Rapid testing is not being done for the vast majority of these gatherings. Air filtration and ventilation are largely ignored. “The pandemic is over” attitude is pervasive and blatantly off-base. Ignoring the circulating virus doesn’t and won’t make it go away. We’re surely putting our elders and immunocompromised people at risk (more on the latter below).
3.The rise of the BQ.1.1 variant
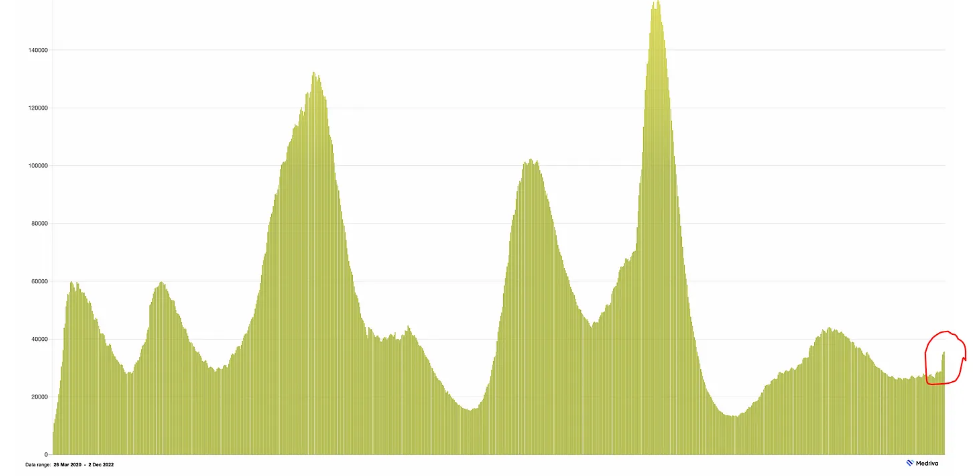
The new CDC genomic data that was released this week showed that BQ.1/BQ.1.1 have shot up to 63% of new cases. The BA.5 wave has faded away (14%) while the worrisome XBB variant is gaining at low levels (now 5.5%) and so is BN.1 (4.6%). The rest of the variant soup is in descent or not gaining traction.
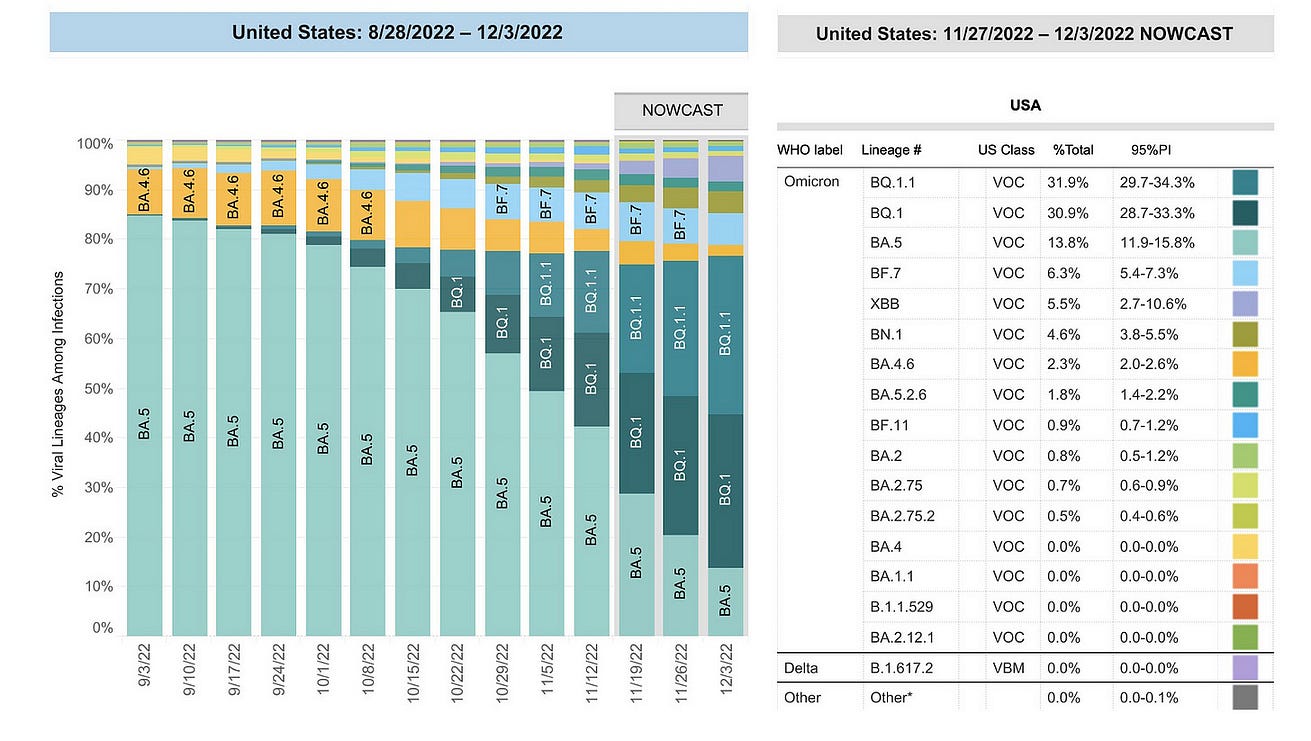
There is a major difference between BQ.1 and BQ.1.1: the R346T mutation in the spike protein (as seen below), which gives the latter variant a big edge in immune evasion and makes it resistant to Evusheld. Both are resistant to Bebtelovimab, which is the reason that the FDA withdrew its authorization (EUA) for this monoclonal antibody this week. If we could do sequencing of the virus sample for an individual, that would be premature, because BA.5 cases would still be responsive. Notably, we’ve lost the important preventive measure for immunocompromised — Evusheld — and there’s no sign of any replacement of combination, effective monoclonal antibodies in the imminent pipeline.
The point here is that it is hard to know how much the BQ.1’s are impacting the current wave, with points (1) and (2) above. But as the BQ.1.1 becomes fully dominant (now ~32% in the US), whatever influence the variant has will increase over the weeks ahead.
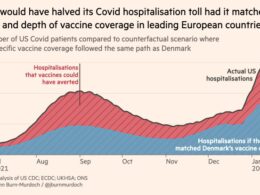
You may recall in my earlier review of this variant, there was a sense of optimism based on what was happening in France with a drop in BQ.1. But that turned out to be related to a lab strike and under-diagnosis of cases and the variants which accounted for them. More recently, France’s hospitalizations are on the ascent as BQ.1.1 has become dominant (vida infra). Importantly, as I previously emphasized, France’s booster rate is 50% higher than the United States.
4.Low Use of Paxlovid
Unlike all the monoclonals that have lost efficacy, Paxlovid still works and the real world data are even better than the EPIC randomized trial that ushered in its use. People who are vaccinated/boosted have as much benefit as those who are unvaccinated; the same for immunocompromised; the same for people with prior covid and across age groups. And the unexpected bonus of a 26% reduction of Long Covid. I recently summarized all these points and more, including the point that rebound is much less of a concern that it was made out to be, and the markedly low rate of use of Paxlovid in people of advanced age.
The wave is not just in the United States
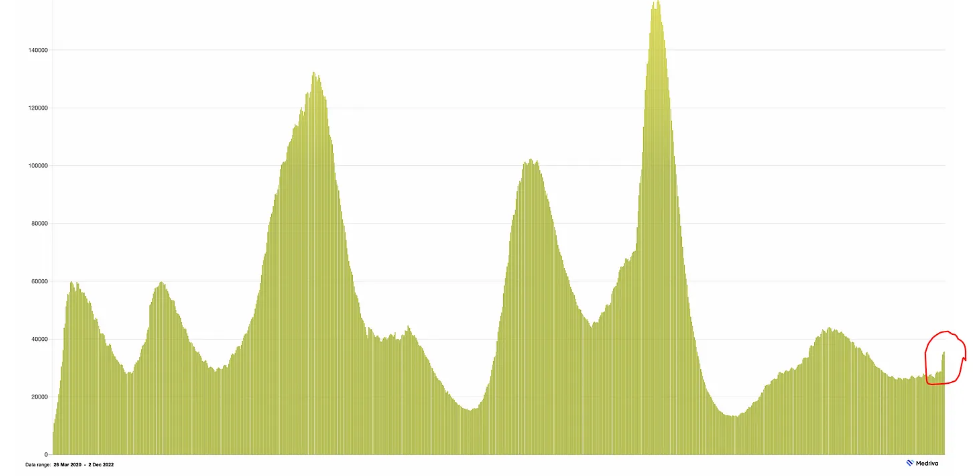
Europe is seeing a similar pattern as seen in many countries using weekly hospital admissions that are up diffusely (countries with data provided by Our World in Data) and most recent BQ.1.1 percentages by cov-spectrum.org
Like the US, except for France (which has the highest hospital admissions per capita) BQ.1.1 has not yet reached dominance (50%+). There is a lag of sequencing and reporting to actual, such that it is likely that BQ.1.1 (and BQ.1) are contributing to the wave in all of these countries to some degree. But again it is hard to dissect out the relative contribution given the other factors reviewed above.
The pandemic is far from over: Asia
Besides what is happening in Europe, and the well-publicized situation in China where the Zero-Covid policy worked well until containment of Omicron became impossible, there is a new wave in Asia developing that includes Japan, Australia, Hong Kong and South Korea
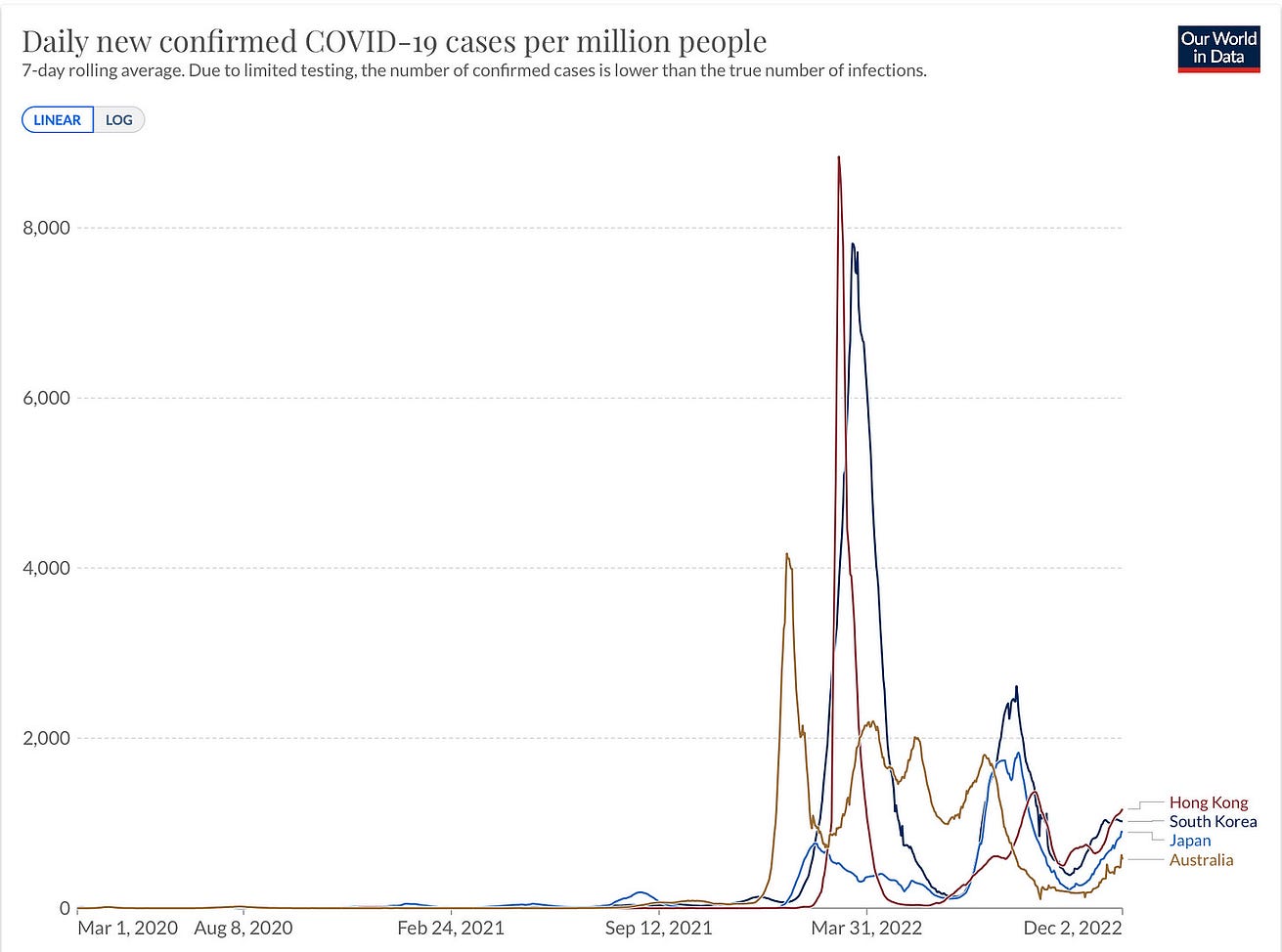
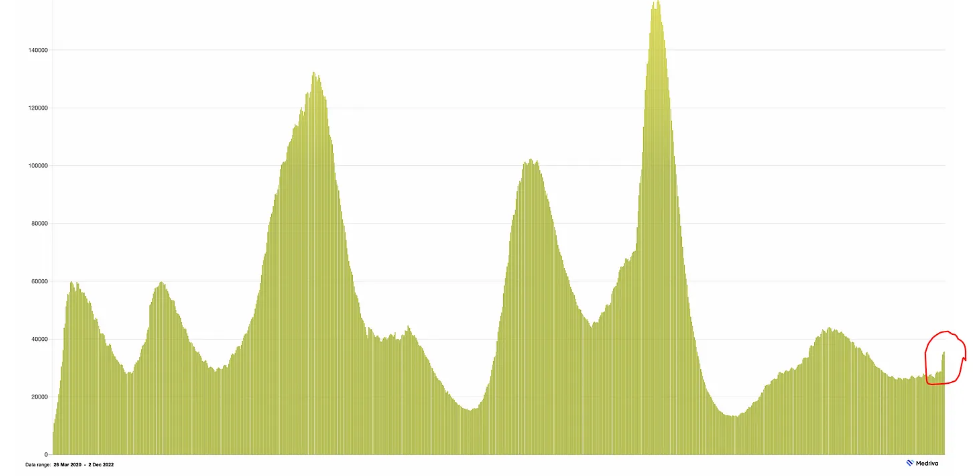
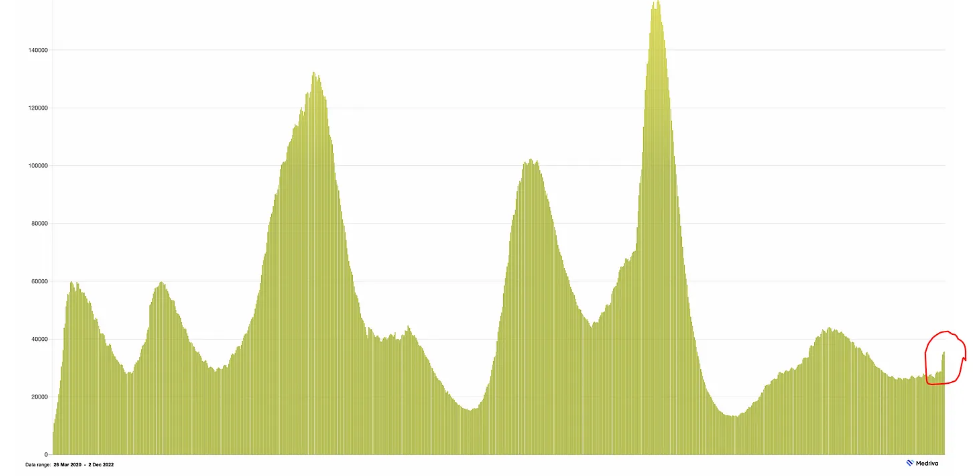
Japan is especially noteworthy because it is experiencing a large and second BA.5 wave (perhaps due to newer subvariants of BA.5 not yet delineated). Japan’s management of the pandemic has been exemplary with an enviable balance of avoiding full lockdowns, use of masks and mitigation, “cluster-busting”and high uptake of vaccinations/boosters. But, as you can see below, there are an average of 120,000 new cases per day and deaths are, in parallel, on the rise, steeply.
The fact that Australia and New Zealand are involved in the new Asian-Pacific wave takes us out of the northern hemisphere and winter/ cold weather as a principal driver. Yes, South America, too.

What’s Next?
The hope is that we’ll not see a major wave in the weeks ahead, but there’s lots of uncertainty, especially in the United States.
A recent preprint from Harvard Chan School of Public Health suggested that 94% of Americans have had Covid at least once (95% confidence intervals 79, 99%) . I found that point estimate hard to believe, not having had Covid and knowing so many people who have not (with nucleocapsid antibody negativity). Putting aside that absolute number, we’ve had a heck of a lot of Covid infections, and reinfections, that together with vaccinations and boosters have built a fairly formidable immunity wall (albeit perhaps less formidable than many countries in Europe, and for a different reason Japan, South Korea, Australia, New Zealand, Singapore, Taiwan and others with their much higher vaccination/booster rates).
Accordingly, just as Singapore largely withstood the XBB variant challenge well, we/globally should be able to handle BQ.1.1.
And we may well be facing XBB or other Omicron BA.2/BA.5 mutation-laden descendants after the BQ.1.1 wave is finished.
The main point is that we’re not doing what we can do reduce the toll of the virus.
That means for everyone (especially age 50+) getting a booster and using mitigation measures appropriately. It also means we’re poorly equipped to ever keep up with the virus, no less get ahead of it, having lost the power of monoclonal antibodies as a backstop and for the immunocompromised. This represents a do nothing posture and extends to not aggressively going after nasal vaccines and pan-β-coronavirus vaccines. The idea that current boosters could be used and effective on an annual basis is balderdash, given their durability is less than 6 months.
The recent extraordinary success of a pan-influenza vaccine, across all Influenza A and B lineages, and effective in experimental models, for the first time, should markedly bolster our confidence for developing one against SARS-CoV-2, a much easier target than influenza.
But we’re not doing that. All part of a complacency syndrome, as I recently posted about below. And there is still looming the potential that we will get “Omicron-ized” with a whole new, antigenically distinct family of variants (say Pi or Sigma) in the months or years ahead that we’re not prepared for, but certainly could be.

Whatever happens in the current Covid wave, and it certainly will not be as as bad the initial Omicron BA.1 or Delta waves, I know we in the US could do far better.
At some point an aggressive push for better vaccines, new antibodies and pills to replace or combine with Paxlovid will all get done. The question is why do we have to wait for the urgent, reactive need when all of that can be anticipated.
Thanks for reading sharing and subscribing to Ground Truths!
Originally published at https://erictopol.substack.com on December 3, 2022.