This is an Executive Summary with the title above, of the article “Re-Imaging Radiology”, by Artur Olesch @ About Digital Health, which version is fully published on the 2nd part of this post.
Re-Imaging Radiology
About Digital Health
Artur Olesch
February 19, 2022
Interview with: Prof. Dr. med. Mathias Goyen — Chief Medical Officer EMEA at GE Healthcare
Executive Summary
by Joaquim Cardoso MSc
Chief Editor of The Digital Health Strategy Blog
February 23, 2022
What was the impact of the pandemic in Health Care and Technology?
- The COVID-19 pandemic has revealed how vulnerable the health care industry is to change and its need for structural and technological transformation.
- Digitalization will help solve some of the challenges that exist today, but the problems will not be solved overnight.
- And while disease will never be completely eliminated, through science, data, and technology, we will be able to identify it earlier, intervene proactively, and better understand its progression to help consumers and patients more effectively and actively sustain their well-being.
What is your opinion about the future of radiology, and your advice for medical students?
- Radiology is a necessary and highly relevant specialty, but it will change fundamentally — perhaps more than other specialties — due to the possibilities of digitization.
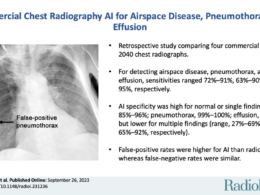
- AI can truly augment the daily work of radiologists. For example, AI will support radiologists in the interpretation of less challenging cases, which will give the radiologists more time to focus on the challenging tasks as well as interactions with patients and other clinicians.
- There are some voices warning of the effects of AI, especially for radiology. Some future scenarios predict that AI might replace the human radiologist.
- This possibility of AI replacing many radiologists is generally dismissed by the radiology community. The arguments usually include that AI will never be able to match the keen eye of a radiologist or that radiologists do more than interpret images. This might be true.
- However, I think that AI has the potential to create a significant disruption in the radiology workforce. Such disruption is a real possibility.
- Although the radiology specialty has shown an astonishing ability to adapt to the changing technology, the future is uncertain — an honest, in-depth discussion is needed to guide the development of the field.
What is your more realistic vision of digital healthcare?
- For me, a realistic future of digital healthcare consists of a connected and highly accessible network of virtual and in-person care, with real-time and predictive insights supporting care collaboration across the patient journey.
- In tandem, AI-enabled workflow optimization can help improve operational efficiency so that healthcare professionals get to focus on what they do best: providing patient care.
- And by enabling people to take better care of their health and well-being with personalized digital health solutions, we can promote a shift from sick care to true health care.
- Taken together, that’s how digital transformation can support better health outcomes, improved patient and staff experience, and lower cost of care.
What are the trends for the radiologist, along the patient journey?
- Multispecialty physicians and caregivers must work together in teams, esp. in cancer care.
- The AI-empowered radiologist can play the key role of jumping in to investigate disease — diagnosing, staging, monitoring, and following it over time and offering expertise and consultation on disease states.
- Radiology often serves as the patient entry point into the cancer care system. Therefore, it is uniquely positioned to play a value-adding role in facilitating patient and team engagement, especially during cancer care initiation.
- I don’t get tired of proposing radiology to assume the “Quarterback” function during this process and engaging the patients and their care team in timely, coordinated activities. After initial consultations and treatment plan development, the Quarterback function is transitioned to surgery or medical oncology.
- It is a tremendous opportunity to get radiologists from behind the monitor and bring them back into daylight by empowering them to become more “doctor” than ever before.
What are the trends in two decades from now?
- In 10–15 years from now, there might be a new discipline which would encompass radiology, pathology, and molecular testing and called “diagnostic medicine” or “integrated diagnostics.”
- We have already seen the beginning of integrating pathology and radiology disciplines that both form the core of cancer diagnosis. Both share a mission of diagnosing disease through images and biomarkers.
- The integrated reports of pathologists and radiologists working collaboratively would achieve higher levels of quality.A single pathology-radiology report has already become a reality at several University Medical Centers.
- The science and research agendas of molecular imaging and molecular diagnostics already show extensive overlaps.
- However, it will be a long time — if at all — before the two specialist areas are merged into an integrated knowledge base, a uniform professional identity, and a newly designed, joint residency training.
- Is the radiologist and pathologist as we know them today an extinct species? Will there be “diagnosticians” in the future? That gives us a lot to ponder — these are some exciting times.
ORIGINAL PUBLICATION (long read)

Re-Imaging Radiology
About Digital Health
Artur Olesch
February 19, 2022
Interview with: Prof. Dr. med. Mathias Goyen — Chief Medical Officer EMEA at GE Healthcare
As a radiologist scientist and clinician, Prof. Dr. med. Mathias Goyen — Chief Medical Officer EMEA at GE Healthcare — knows the evolution of medical imaging from the inside out.
So I asked him about the future of radiology, how to improve accurate diagnosis and the gap between the capabilities of technology and clinical practice.
When you started to study medicine in the 90s, how did you imagine the future of healthcare in 30 years, in 2020?
To be honest, in the 1990s, when I started studying medicine, I wasn’t as concerned about the future of medicine as much as I was focused on getting through my medical studies relatively “accident-free.” Towards the end of my studies in my mid-20s, however, I did think about what the future of medicine might look like and that was quite exciting. I imagined that advances in medical technology, computer science and life sciences would enable us to detect diseases earlier and treat them better in the future. I was eager to take part in this future of medicine.
Having a world without diseases, especially without cancer? I couldn’t imagine that.
But it was also clear to me that, despite all the advances in medicine and related sciences, that the doctor would still be in charge in 30 years. And luckily, that’s how it happened.
For example, artificial intelligence (AI) can support and augment physicians by taking away the data-driven analytical portion of a physician’s work.
Still, luckily, it cannot replace the unique and critical relationship between doctor and patient that will hopefully never disappear.
For example, artificial intelligence (AI) can support and augment physicians by taking away the data-driven analytical portion of a physician’s work.
Still, luckily, it cannot replace the unique and critical relationship between doctor and patient that will hopefully never disappear.
What do patients want? Think of yourself. Patients are always looking for the human touch in medicine. Patients don’t want to get their diagnosis from a computer; they want to talk to a physician.
What do patients want? Think of yourself. Patients are always looking for the human touch in medicine. Patients don’t want to get their diagnosis from a computer; they want to talk to a physician.
As a Star Trek fan, I naturally wondered whether there would really be something like the ‘tricorder’ in the future with the three functions of sensing, recording, and computing. But I quickly dismissed it as a pipe dream. Thirty years on, I realize we’re not that far off.
Think of all the handheld mobile computing devices on the market. There is even the first mobile app to allow anybody to study DNA virtually anywhere using an iPhone or iPad, which many media outlets dubbed to be a “DNA tricorder.”
I asked you that because 30 years ago we hoped that computers would solve all the problems in healthcare and diseases like cancer would be fully treatable. It didn’t happen.
Today we are basically at the same point — we dream about personalized, preventive, and proactive healthcare.
Still, instead, we have healthcare workforce shortages, COVID-19 pandemic, and digitalized but completely not interoperable data.
I don’t entirely share the pessimism that resonates here. Undeterred, medicine has made enormous progress in the last 30 years.
For example, therapies for HIV, hepatitis C, and other infectious diseases have helped millions of patients globally.
Added to this are verifiable advances in the field of precision cancer therapy, cardiology, and transplantation medicine, just to name a few.
On the other hand, I agree that major challenges still lie ahead of us.
The COVID-19 pandemic has revealed how vulnerable the health care industry is to change and its need for structural and technological transformation.
Digitalization will help solve some of the challenges that exist today, but the problems will not be solved overnight.
And while disease will never be completely eliminated, through science, data, and technology, we will be able to identify it earlier, intervene proactively, and better understand its progression to help consumers and patients more effectively and actively sustain their well-being.
And while disease will never be completely eliminated, through science, data, and technology, we will be able to identify it earlier, intervene proactively, and better understand its progression to help consumers and patients more effectively and actively sustain their well-being.

Let’s turn the perspective. What can radiology today that you didn’t think of 30 years ago?
Of course, towards the end of my studies, when it became clear that I would become a radiologist, I thought about how the field of radiology would develop. And of course, I knew that as technological advances emerged, radiology would become faster and more accurate.
But I had no idea at the time that artificial intelligence (AI) — a term that we didn’t even use in medicine back then — would one day make radiologists’ work easier and enable them to handle the unbelievable amounts of data.
What did convince you to become a radiologist?
At the time, I had an idea that radiological data would grow over the years because of technical progress. Still, I could not have imagined that they would explode so incredibly in radiology.
As a medical student, I came early into touch with radiology during internships. I was highly fascinated by the technical possibilities to investigate the human body with impressive precision (already back then). This prompted me to do a radiological doctoral thesis on MRI during my studies.
However, my decision to become a radiologist came from my stay at the University Medical Center Basel in Switzerland during my final year of study. I enjoyed working there, especially during my radiology elective.
However, the final decisive factor in choosing radiology was not the technology but ONE person who fascinated me: the deputy chief physician, Prof. Dr. Georg Bongartz.
I quickly learned from him that in addition to profound radiological knowledge, which a radiologist should naturally have, a radiologist who wants to be taken seriously by his clinical partners is also characterized by deep clinical knowledge.
Prof. Bongartz embodied this in a wonderful way. In addition, he was — and of course, still is — a very nice guy characterized by a cooperative leadership style allowing employees to grow quickly.
In 2020, the British Institute of Radiology published a study, “Artificial intelligence in radiology: does it impact medical students preference for radiology as their future career?”.
31% of students agreed that AI would replace radiologists in their lifetime, 44,8% of them think that AI will reduce the number of radiologists needed on the market.
And what’s your opinion and advice for medical students?
Radiology is a necessary and highly relevant specialty, but it will change fundamentally — perhaps more than other specialties — due to the possibilities of digitization.
AI can truly augment the daily work of radiologists.
For example, AI will support radiologists in the interpretation of less challenging cases, which will give the radiologists more time to focus on the challenging tasks as well as interactions with patients and other clinicians.
There are some voices warning of the effects of AI, especially for radiology.
Some future scenarios predict that AI might replace the human radiologist. This possibility of AI replacing many radiologists is generally dismissed by the radiology community.
The arguments usually include that AI will never be able to match the keen eye of a radiologist or that radiologists do more than interpret images. This might be true.
However, I think that AI has the potential to create a significant disruption in the radiology workforce. Such disruption is a real possibility.
Although the radiology specialty has shown an astonishing ability to adapt to the changing technology, the future is uncertain — an honest, in-depth discussion is needed to guide the development of the field.
However, I think that AI has the potential to create a significant disruption in the radiology workforce. Such disruption is a real possibility.
I would like to touch on a related topic quickly:
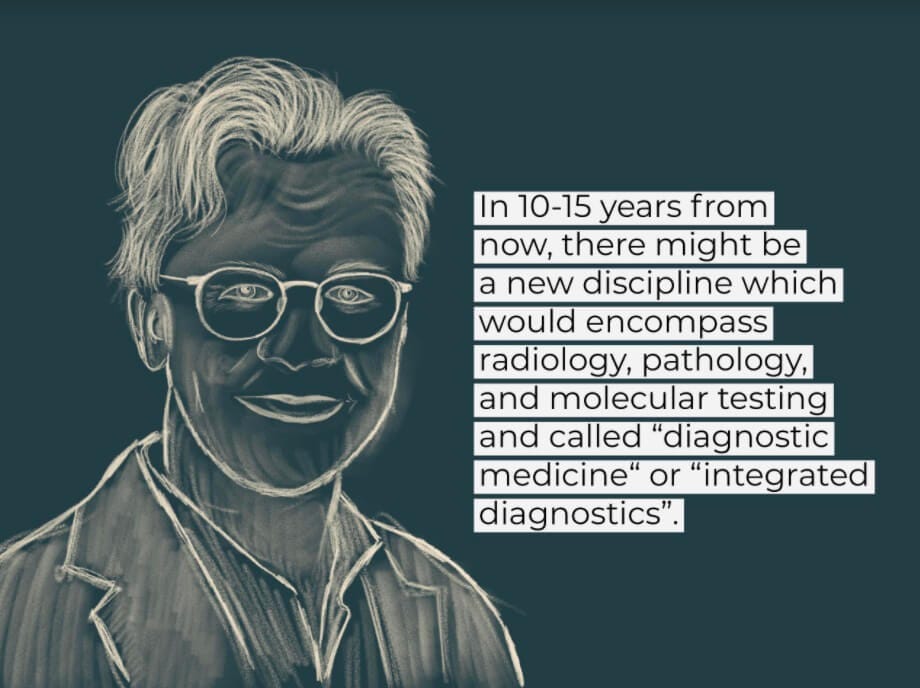
In 10–15 years from now, there might be a new discipline which would encompass radiology, pathology, and molecular testing and called “diagnostic medicine” or “integrated diagnostics.”
We have already seen the beginning of integrating pathology and radiology disciplines that both form the core of cancer diagnosis.
Both share a mission of diagnosing disease through images and biomarkers.
The integrated reports of pathologists and radiologists working collaboratively would achieve higher levels of quality.
A single pathology-radiology report has already become a reality at several University Medical Centers.
The science and research agendas of molecular imaging and molecular diagnostics already show extensive overlaps.
However, it will be a long time — if at all — before the two specialist areas are merged into an integrated knowledge base, a uniform professional identity, and a newly designed, joint residency training.
Is the radiologist and pathologist as we know them today an extinct species? Will there be “diagnosticians” in the future? That gives us a lot to ponder — these are some exciting times.

After ten years in GE Healthcare, can you admit: “yes, we can today diagnose patients better what leads to better patient outcomes”?
One important goal in radiology is to detect tissue changes at an early stage.
There is no doubt that medical technology has made enormous progress in the last decade, which patients benefit from.
AI algorithms, for example, provide radiologists with groundbreaking help when viewing images, so that suspicious findings are pre-marked by recognizing patterns, which are then checked for plausibility by the experienced radiologist, evaluated, and approved or rejected accordingly.
This generally leads to an earlier and more accurate diagnosis, which can lead to a better patient outcome.
The progress in radiology is impressive. The doctors have access to high-quality images with an extraordinary resolution, and AI algorithms support their decision-making.
But still, the patient journey for cancer patients is simply too long or complex — many cases are diagnosed too late.
What is the next step for radiology to improve this? What is missing to leverage the potential of technologies we have already developed?
In cancer care, the idea is to focus on the patient’s overall journey rather than the contribution of each specialty or caring function independently.
Patient and care team engagement are crucial at the time of cancer diagnosis and care initiation but are complicated by the necessity to orchestrate many interdependent consultations and care events in a short time.
Therefore, multispecialty physicians and caregivers must work together in teams, esp. in cancer care.
The AI-empowered radiologist can play the key role of jumping in to investigate disease — diagnosing, staging, monitoring, and following it over time and offering expertise and consultation on disease states.
Radiology often serves as the patient entry point into the cancer care system.
Therefore, it is uniquely positioned to play a value-adding role in facilitating patient and team engagement, especially during cancer care initiation.
I don’t get tired of proposing radiology to assume the “Quarterback” function during this process and engaging the patients and their care team in timely, coordinated activities.
After initial consultations and treatment plan development, the Quarterback function is transitioned to surgery or medical oncology.
This model provides radiologists with opportunities for truly value-added services and solidifies radiology’s relevance in the evolving healthcare environment.
It is a tremendous opportunity to get radiologists from behind the monitor and bring them back into daylight by empowering them to become more “doctor” than ever before.
I don’t get tired of proposing radiology to assume the “Quarterback” function during this process and engaging the patients and their care team in timely, coordinated activities.
You are a strong supporter of digital health tech, often presented as a perfect world where data is connected, advanced wearables monitor people’s health 24/7, and health services become accessible and affordable for all.
But what is your more realistic vision of digital healthcare?
For me, a realistic future of digital healthcare consists of a connected and highly accessible network of virtual and in-person care, with real-time and predictive insights supporting care collaboration across the patient journey.
In tandem, AI-enabled workflow optimization can help improve operational efficiency so that healthcare professionals get to focus on what they do best: providing patient care.
And by enabling people to take better care of their health and well-being with personalized digital health solutions, we can promote a shift from sick care to true health care.
Taken together, that’s how digital transformation can support better health outcomes, improved patient and staff experience, and lower cost of care.
Everybody who follows you on LinkedIn recognizes your unique communication style.
You rarely talk about technology, solutions, inventions, science but rather pay attention to simple things or people.
Is it a tailored communication strategy or a sentiment for more humanity in a digitalized world?
I like your analysis. I could now claim that an armada of social media specialists is behind selecting the content, but that would not be the truth. I do it alone and just enjoy LinkedIn.
I let scientists communicate in a highly scientific way.
Still, I like to summarize current research content in a compact and hopefully understandable language.
LinkedIn is first and foremost a business network, I respect that, but it is certainly not forbidden to post some things with a winking eye. And yes, the observation is correct. I also try to bring a personal, human touch to my posts.
What worries you more when you observe the medicine here and today: data leaks and cybersecurity or that 10–20% of societies still don’t trust the science?
Both topics are extremely important.
Over 40 million people in the United States alone had their personal health information exposed in data breaches last year. There are a few ways these types of breaches can harm patients: people can have private information exposed and could have to deal with the financial repercussions of having their medical identity stolen.
Hacks and attacks on healthcare institutions that shut down hospital computer systems can make it harder for them to deliver quality care — that can be harmful to the people treated there. Unfortunately, many healthcare organizations haven’t prioritized investment in cybersecurity, even as the risk of cyberattacks continues to increase.
The topic is so important because health is a matter of trust. As a patient, I must be sure that my health data is protected. If this is not guaranteed, there will be a major breach of trust, which can potentially shake my faith in science itself.
Therefore, Science Communication is so important. In my opinion, it is imperative to nurture and strengthen public confidence in science. Clear, accurate, transparent public communication from scientists is essential, especially in a pandemic.
The COVID-19 pandemic has seen more scientists than usual enter the public arena, many of them for the first time. Every day, researchers are interviewed in the media, advise policymakers and write social media posts. They might be discussing the latest coronavirus data, explaining and interpreting new research, or commenting on government policies.
In general, scientists and health officials should expect their research to be questioned and challenged and should welcome constructive feedback. But threats of violence and extreme online abuse do nothing to encourage debate — and risk undermining science communication at a time when it has never mattered more.
To wrap up, please ask yourself one question that you’ve never received in an interview, but you wanted to be asked about it. And of course answer it!
My question would be:
“If you could compare yourself with any animal, which would it be and why?”
My answer would be:
“Definitely a meerkat.”
First of all, their body is long and slender. 🙂
Meerkats are very social animals. They like to snuggle up very closely to maintain physical contact, and the colony also takes care of sick or injured meerkats and grants the animals’ special protection.
Because they love warmth, these diurnal animals can often be seen sitting in the sun in front of their burrows. They sunbathe to warm up, especially in the morning hours.
When resting, they sit on their buttocks, hind legs, and tail pointed forward.
The close cohesion of the group ensures their survival in Africa.
Originally published at http://aboutdigitalhealth.com on February 19, 2022