What is the message ?
Transitioning to value-based care through data-driven innovation improves patient outcomes and reduces healthcare costs.

Adapted from “Turning data into value”, published by Siemens Healthineers, written by Hee Hwang, Joanne Grau, and Ralph Wiegner , in 2021 (Issue 21)
Executive summary
How can a society as a whole become healthier? This would require preventing chronic conditions from happening in the first place and providing treatment that works. And the less money a society spends on healthcare, the better.
While this may sound like an obvious concept, the conventional fee-for-service model is not conducive to reaching that goal as it offers little incentive to deliver efficient care.
Providers, particularly large organizations, often focus on expensive treatments rather than disease prevention. Patients receive more tests and procedures than they need.
Fortunately, the healthcare industry has been steadily pivoting away from such fee-for-service systems to alternative “value-based care” system. Value in healthcare means maximizing patient outcomes while reducing costs.
Under this system, providers are reimbursed based on quality and outcomes, driving hospitals and health systems from reacting to anticipating the needs of their patients.
To be successful under this model, insights surrounding every aspect of care delivery — quality, cost, utilization, variations in care, patient behaviors and patient outcomes — are required.
Data and analytics are one of the keys to obtaining such insights. There is a wealth of untapped information flooding in and the amount of healthcare data being generated continues to skyrocket.
Yet without innovative, digitalized solutions, data becomes disparate and cannot be leveraged effectively.
There needs to be a platform that connects this data automatically and acts as the central host of a broad range of Artificial Intelligence (AI)-powered applications for better decision-making.
Standardizing quality decision-making using this data and making it accessible by caregivers at any level can turn data into value.
Seoul National University Bundang Hospital (SNUBH) in South Korea has successfully made use of its patient data by developing its own integrated platform after years of research.
This allows for the use of AI-powered software to support hospital staff to make evidence-based decisions for better patient care and operational outcomes.
The key to its success lies in its ability to mobilize hospital staff and provide the right tools for them to collect and use data for better patient outcomes.
By having a comprehensive view of the patient, care can be more precise and prevention more attainable.
Its efficient use of resources through digitalization has helped SNUBH to grow its revenue more than 11-fold since it embarked on this journey in 2003.[2]

DEEP DIVE
Background
South Korea is facing a demographic crisis due to low birthrates and an aging population,[3] which is a problem that many developed countries are facing. With that comes the challenges of workforce shortages and the rise of chronic diseases. To combat that, the government in South Korea has been committed to promoting value-based, preventive care and investing in information and communication technology (ICT) to improve the health of its people.[4]
South Korea’s response to COVID-19 has been impressive. Building on its experience in handling Middle East Respiratory Syndrome (MERS), South Korea was able to flatten the epidemic curve quickly without closing businesses, issuing stay-at-home orders, or implementing many of the stricter measures adopted by other high-income countries in 2020. Besides the clear guidelines from the government and its “test, trace, isolate” strategy, the readiness of healthcare providers and hospitals played a critical role.
The importance of value-based care was put to a pressure test during the COVID-19 pandemic. Do institutions that have switched over to an evidence-based care approach manage the pandemic better? Is the investment in value-based care infrastructure, such as healthcare information technology and data integration platform, paying off?
A case in South Korea proves such investments to be invaluable. When it was founded in 2003, the managing board of SNUBH located in Seoul, South Korea already set its strategy to tackle the challenges posed by an aging population with a focus on digitalization. It firmly believes that digitalization is one of the key paths to increase efficiency and make preventive medicine a reality.
SNUBH is a tertiary hospital that has been progressively adopting information technology (IT) for better patient care.
Dr. Hee Hwang, a professor of pediatric neurology, took the helm of SNUBH’s IT department as the Chief Information Officer in 2004. Under his leadership, SNUBH is recognized globally as a leading digital hospital and also the first hospital outside the U.S. to achieve HIMSS EMR Adoption Model (EMRAM) Stage 7 status and revalidation, meeting the new criteria set up by HIMSS Analytics. EMRAM is an eight-stage model (0 to 7) that measures digital maturity in hospitals. Achieving EMRAM Stage 7 represents an advanced patient record environment that is truly paperless and uses information and technology in a way that creates benefits for both patients and clinicians.
SNUBH has been consistently ranked first in quality measurements of general hospitals and has received awards and recognitions from Health Insurance Review and Assessment Service.[5]
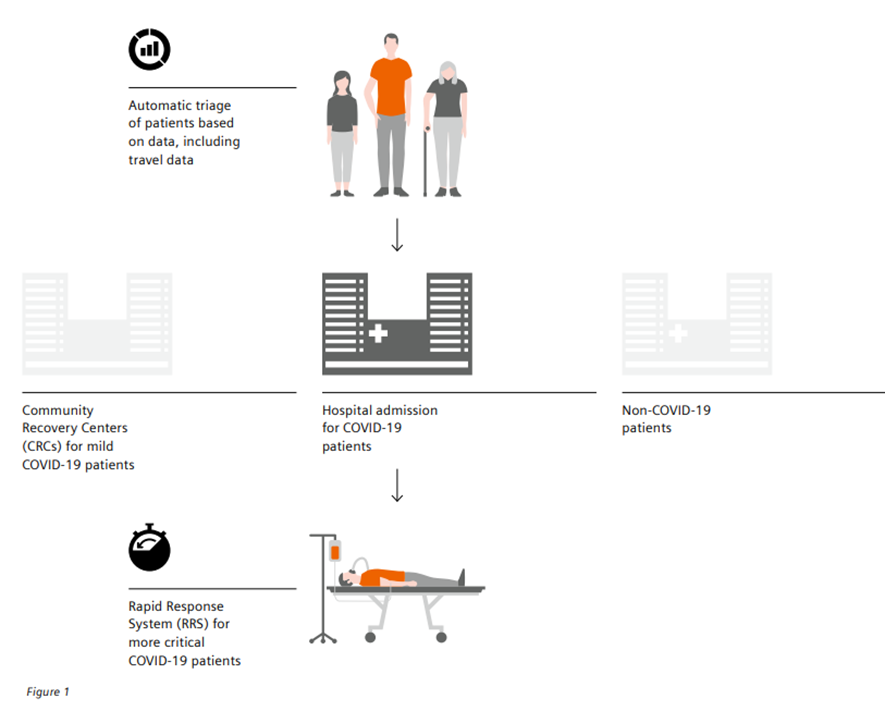
When the pandemic hit, SNUBH was ready to face the challenge. SNUBH was able to integrate and retrieve patients’ travel record and automatically triage them to minimize exposure of staff and patients to potential infection risk.
SNUBH was operating 1,360 inpatient beds and caring for an average of 7,000 inpatients daily.
With the spike in COVID-19 patient volumes, it was quick to establish Community Recovery Centers (CRCs) to cope with the workload. CRCs are facilities that serve patients who have been diagnosed with mild COVID-19, and the exchange of data allows medical staff to care for these patients remotely.
SNUBH also developed a Rapid Response System (RRS), which was fully integrated into its home-grown Electronic Health Record (EHR) system and monitors all inpatient test results and vital signs 24/7 since 2013.
The system works particularly well in wards where COVID-19 patients are hospitalized. Medical personnel can monitor the status of all COVID-19 patients at a glance without direct physical contact.
SNUBH can swiftly adapt and keep the situation under control, thanks to its well developed IT infrastructure and data integration readiness that stems from its commitment on high value care.
Figure 1
How healthcare IT has helped SNUBH manage the COVID-19 pandemic
The challenge
Despite the advantages of value-based care, its expansion has been slow.
One obstacle is the culture of healthcare. The healthcare profession has historically focused on science and treatment, and many innovations have come out of that. Yet the shift to value-based care also puts a spotlight on a patient’s individual life context, as a thorough understanding of the social environment surrounding the patient is the key to successful prevention and treatment. This requires physicians and nurses to change the way they practice. Yet many have been slow to embrace the change for a host of reasons.
Research shows that one main reason is that they feel excluded from the process.[6] Physicians clearly understand the challenge posed by rising costs for clinical care and prescription drugs, but many do not feel they are in a position to help rein in costs. Physicians who are not aligned and engaged with their organization have more reasons to resist new systems.
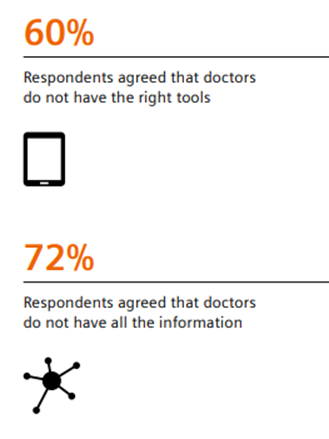
A second obstacle is the availability of tools. Even if doctors are engaged, do they have the right tools to succeed?
According to a research with 451 primary care physicians and health plan executives, nearly 60% said that doctors did not have the right tools to be effective, and nearly three-quarters (72%) of respondents said physicians did not have all the information they needed about their patients.[7]
Much of the current medical infrastructure and technology is built to support the treatment of severe conditions rather than promote health and wellness.
To promote preventive care, there needs to be an efficient way to collect patient information from various sources.
Data entry is viewed as an administrative task. If doctors have to type in data in a structured format and it slows them down or creates an additional burden, they are less likely to support it.
Once data is collected, hospital IT and electronic medical record systems also need to make this data usable by solving the challenge of analyzing and deploying data so that it can facilitate communication and support decision making.
Figure 2
Do the doctors feel they have the right tools and all the information they need to succeed? [8]
· 60% of respondents agreed that doctors do not have the right tools
· 72 % of respondents agreed that doctors do not have all the information
The solution
When Dr. Hwang took on the responsibilities of CIO, he was clear that his mission was to help SNUBH deliver its promise of offering world class patient-centered care through digitalization.
Yet he was frustrated with the lack of available options in the market at the time. He decided to look inward for a creative solution.
He embarked on a journey to develop a platform that not only would fulfill the needs of internal stakeholders, but also comply with various international and national healthcare accreditation systems.
The core of his strategy lies in bringing caregivers and end-users to the center of the digital transformation process, and offering them the right digital tools they need to succeed.
SNUBH’s own home-grown EHR solution, named BESTCare 2.0 (Bundang Hospital Electronic System for Total Care), integrates the patients’ clinical, financial, medication, genetic sequencing, travel, and personal records of daily life, i.e. lifelog, data, thereby opening up the opportunity to apply a comprehensive range of applications to make evidence-based decisions from diagnosis to therapy to follow up.
This holistic view of the patient enables caregivers to give the patients the best care possible with the lowest cost.
Figure 3
SNUBH’s data integration strategic framework
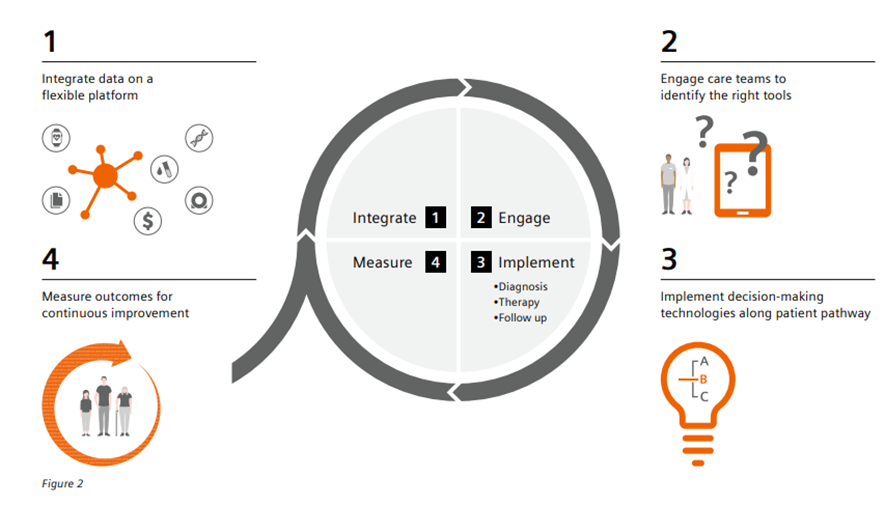
· 1.Integrate data on a flexible platform
· 2. Engaging care teams to identify the right tools
· 3. Implement decision-making tools along the patient pathway
· 4. Measure outcomes for continuous improvement

1.data on a flexible platform
SNUBH’s BESTCare system is an integrated platform of comprehensive applications for direct care and support care of outpatients, inpatients, intensive care units, emergency room, and operating room units.
SNUBH ensures its platform fully complies with international standards such as Health Level 7 (HL7) V2.X messaging and HL7 Clinical Document Architecture (CDA).[9]
The mapping of the terminology to the standard takes place in the backend so that changes do not disrupt the workflow of the caregivers.
Two engineers and one nurse are dedicated to ensure high data quality by running precision comparison tests routinely.
When the pandemic hit, a datalink was established between the national immigration service and SNUBH’s flexible platform to enable automatic triage which minimized infections within the hospital.
The platform also allows healthcare professionals to access the EHR system with full functionality from outside the hospital either by using a mobile EMR system through Virtual Private Network (VPN), or using Virtual Desktop Infrastructure (VDI) account to access original EHR with a laptop or tablet.
This enables caregivers to visit patients’ homes without any paper or printed records and to both access and capture patients’ data on site, resulting in improved quality of care and efficient access to medical records.
SNUBH integrates various sources of patient data
• Clinical data
• Medication data
• Financial data
• Genetic sequencing data
• Wearables data
• Travel data
• Record of daily life
Another key concept of the platform is to provide caregivers with a holistic view of the patient. Based on the data, the platform generates a patient journey map for caregivers which shows all patient-related longitudinal events in the outpatient clinic, inpatient department, emergency department, and various examination suites in a visualized form.
It also shows the patient’s history of surgical procedures, diagnoses, discharge summaries, test results, and medications to enable medical staff to understand complex patient information at a glance.
The platform further supports caregivers by enabling a host of applications and tools that covers the continuum of care from diagnosis, to therapy, to follow-up.
2. Engaging care teams to identify the right tools
How did SNUBH overcome the cultural barrier to get caregivers and patients engaged? A practical way to make digital transformation a reality is to bring caregivers into the center of the decision-making process. Caregivers who are engaged in decision-making are much more satisfied with the working environment and are more willing to lead change.[10]
One thing that SNUBH has done well is listening to real users. During the process of developing their own platform, Dr. Hwang and his team actively involved doctors and end-users through constant communication.
There were diverse task forces for decision-making to make sure the platform was adjusted to effectively support the users’ complex tasks. Dr. Hwang is especially interested in inviting critics of digitalization to the decision-making process.
During the development of a quality measurement tool, for example, a task force was formed consisting of doctors, nurses, pharmacists, staff members from the medical information team, the health insurance team, and the quality assurance (QA) team.
It is known that EHR user interfaces and data entry procedures are a major obstacle to healthcare professionals’ use and acceptance of EHRs, meeting this design challenge is the most important factor that will influence future success.
In this platform, end-users can also configure and use their own user interface (UI) rather than using fixed, common UI. Making the platform user-friendly and easy to use is the key to increase its adoption.
The medical informatics team also provides training sessions regularly to users at every level.
By designing a platform that incorporates user feedback, they have been able to accomplish two important goals: more data can be captured which leads to higher accuracy, and it offers caregivers the right tools they need to deliver value-based care.
Understanding a patient’s life as a whole instead of focusing on simply treating an illness is a crucial factor in value-based care. Hospitals would need comprehensive information about patient’s daily life, yet it would not be feasible to add the data entry burden to overworked caregivers.
To avoid the tedious data entry and to engage patients to take charge of their health, the platform also enables patients to access their medical records, fill out pre-visit questionnaires online, send in data through their wearable devices, facilitate the use of their data in clinical and epidemiological research, and communicate with healthcare professionals about their current health status in a timely fashion.
This is accomplished through an innovative EHR-tethered Patient Health Record (PHR) system that was developed through a co-creation workshop with clinicians.
Patients’ wearable data is automatically retrieved to a hospital EHR system, and patients can record their daily food intake and activity through an app. The ability to collect biological, environmental, and behavioral data of a patient can help clinicians to gain better insights for more individualized care.
While it was initially designed to manage non-communicable chronic diseases, it became an effective tool to manage highly contagious disease such as the COVID-19 outbreak.
3. Implement decision-making tools along the patient pathway
With key information readily on hand, clinicians can benefit from a variety of digital tools to help them make faster and better decisions along the patient pathway.
Diagnosis
The platform developed by SNUBH enables Clinical Decision Support System (CDSS) rules to help clinicians make decisions on diagnosis and treatment with the latest scientific evidence. The CDSS can check for overlapping prescriptions, drug-drug interaction, renal dosing guidelines, overdose prevention, contradictions for age, pregnancy and breast feeding, and drug-disease interaction, resulting in much higher safety and avoiding negative outcomes for patients. One example use case is the automatic Acute Kidney Injury (AKI) alert. The system screens for AKI events every midnight by comparing patients’ serum creatinine data to the baseline. When there is an AKI event, it automatically generates a pop-up message in the medical record and alerts the doctor to send a consultation request to the nephrology division. The alert has significantly lowered the odds of overlooked AKI events and severe AKI events, resulting in an increased rate of early consultation more than four-fold and significant improvement in AKI recovery rate.[11]
Therapy
The platform also leverages on analytics and AI technologies to support clinical decision-making through Clinical Pathways (CP). The CP takes patients’ clinical status and compares it against the current guidelines for various diseases to ensure standardized care and best practices are followed. Once the CP is confirmed in the EMR system, it activates the CP workflow and provides the next desired steps. SNUBH has built direct communication functionality tools such as telephone, email, cell phone, messenger, video call, and video conference systems into its platform. If there is a variation of standard treatment process and consultation is needed, communication with other departments is just one click away. SNUBH has designed and implemented more than 150 CPs from 13 departments[12] (see Table 1), which means it has a CP application rate of 85%. Clinical pathways ensure that best practices are applied every time which reduce variations in care and unnecessary tests and procedures. Combined with barcodes and Radio Frequency Identification (RFID) technology for cross-checking patient information with medical orders, it ensures that the right patient will get the right drug, at the right dose, with the right route, at the right time.
Follow-up
Value-based care leads to better health outcomes because it encourages patients to play a more dynamic role in their healthcare and promotes preventive care. With the EHR-tethered PHR system, the platform allows patients to enter their health information and communicate directly with caregivers. One use case is in the management of diabetes. Patient-specific messages about glucose, diet, and physical activity are sent directly to patients’ mobile phones and on the website based on their data. A study has shown that patients’ hemoglobin A1C levels, an important marker for management for diabetes, were significantly decreased compared to those who did not use such service. The percentage of patients who reached their HbA1c goal was doubled in the group using such service compared to the group who did not.[13] With such tools, patients can not only get interventions earlier, but they can avoid getting sick in the first place.
SNUBH researchers, physicians, and nurses could analyze data in near-real time by using the tools without assistance from IT staff. With that, caregivers are empowered to take an active role in delivering highest quality care possible.
4. Measure outcomes for continuous improvement
How do we know whether these tools are delivering value? To answer that question, SNUBH continuously monitors and improves the quality of care by applying four types of electronic indicators: clinical indicators, performance indicators, safety indicators, and patient experience indicators.
This is enabled by the Clinical Data Warehouse (CDW) system which includes functions to retrieve unstructured medical records such as physician comments in text data, nursing records, prescription data, and sensor and bar code information from medical devices. The clinical indicators are a collection of indicators related to treatment activities and it objectively measures and continually monitors medical quality of care.[14] Through continuous monitoring, it identifies and avoids predictable and preventable outcomes which reduces costs. As an example, SNUBH has been able to reduce the antibiotic cycle for preoperative patients from 6 days to 1 day, minimizing overprescribing.[15] Today, the hospital manages 320 clinical indicators (see Table 2) with only six nurses — compared to as many as 100 caregivers in other hospitals of similar size.[16] SNUBH also sets up various task forces to continuously collect user feedback and make decisions to upgrade tools, keeping them relevant to caregivers’ daily work and enabling them to drive better outcomes for patients.
Only six nurses are needed to manage 320 clinical indicators (compared to up to 100 caregivers in other similar sized hospitals)
Conclusion
The sheer volume of health care data is growing at an astronomical rate. It is estimated that more than 2,000 exabytes of data were generated in 2020,[17] translating to an equivalent of more than 5 billion Netflix streaming hours every day. Not only that, the overall rate of data volume is increasing by at least 48% annually.[18]
This data comes from health records, medical imaging, genomic sequencing, payor records, smartphones, wearables and more.[19]
Hospitals that want to succeed in offering value-based care would need to be ready to successfully integrate data from various sources to harness its power to provide optimal care.
The experience of SNUBH highlights the importance of actively listening to and involving the doctors, nurses, and staff. At the center of value-based care is patient experience and satisfaction. Care teams have the in-depth knowledge of what patients need and sidelining them will only undercut the effort. Engaging the whole care team as well as patients to employ the right tools to collect, share, and use data will be key for the value-based care model to live up to its promise.
The right digital tools for the care team are the ones that prioritize patient care and experience, and are also flexible to meet their changing needs. One of the trends is to utilize a scalable and flexible cloud-based integration platform that integrates various sources of data.
A single vendor but device-neutral platform can foster cross-departmental and cross-institutional interoperability for clinical and operational efficiency.
Once the data is integrated, innovative AI-powered software and applications can translate data into actionable insights for caregivers to provide the most optimal care.
Clearly, the needs of each hospital are unique. Healthcare-focused consulting companies can conduct a more in-depth analysis of data integration needs and provide tailored recommendations.
One could also consider joining a healthcare IT professional community specialized in data integration topics to get the latest information and share experiences.
SNUBH’s early decision to manage data as strategic asset and its investment in digital transformation were the keys to its success in handling the COVID-19 pandemic. Its comprehensive approach to data integration overcomes both the cultural and technological barriers by putting care teams and patients in the center of its development.
It shows us that the reality of value-based care is within reach, and its success is an inspiration for all of us.
References
1. Gwang-seok C. [Special] SNU Bungdang Hospital’s revenue jumps 11 folds in 15 years [Internet]. KBR. 2018 [cited 2021Apr14]. Available from: koreabiomed.com/news/ articleView.html?idxno=3660
2. Mohw.go.kr. 2021. Ministry of Health & Welfare: Policies Challenges & Tasks Ahead. [online] Available at: mohw.go.kr/eng/pl/pl0103. jsp?PAR_MENU_ ID=1003&MENU_ID=100326
3. Seoul National University Bundang Hospital: [Internet]. Seoul National University Bundang Hospital [cited 2021Apr14]. Available from: snubh.org/dh/main/index. do?DP_CD=EN&MENU_ ID=001035
4. Doctors Feel Excluded from Health Care Value Efforts [Internet]. Harvard Business Review. 2017 [cited 2021Apr12]. Available from: hbr.org/2017/10/doctorsfeel-excluded-fromhealth-care-value-efforts
5. Diagnostics, Q., 2021. New Study Reveals Stalled Progress Toward Value-Based Care. [online] Prnewswire.com. Available at: prnewswire. com/news-releases/newstudy-reveals-stalledprogress-toward-valuebased-care-300681686.html
6. Yoo S, Lee KH, Lee HJ, Ha K, Lim C, Chin HJ, et al. Seoul National University Bundang Hospital’s Electronic System for Total Care. Healthc Inform Res. 2012;18(2):145–52.
7. Park, S., Baek, S., Ahn, S., Lee, K., Hwang, H., Ryu, J., Ahn, S., Chin, H., Na, K., Chae, D. and Kim, S., 2018. Impact of Electronic Acute Kidney Injury (AKI) Alerts With Automated Nephrologist Consultation on Detection and Severity of AKI: A Quality Improvement Study. American Journal of Kidney Diseases, 71(1), pp.9–19.
8. Yoo, S., Hwang, H. and Jheon, S., 2016. Hospital information systems: experience at the fully digitized Seoul National University Bundang Hospital. Journal of Thoracic Disease, 8(S8), pp.S637–S641.
9. Lim, S., Kang, S., Kim, K., Moon, J., Choi, S., Hwang, H., Jung, H., Park, K., Ryu, J. and Jang, H., 2015. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetologica, 53(2), pp.189–198.
10. Yoo, S., Kim, S., Lee, K., Jeong, C., Youn, S., Park, K., Moon, S. and Hwang, H., 2014. Electronically implemented clinical indicators based on a data warehouse in a tertiary hospital: Its clinical benefit and effectiveness. International Journal of Medical Informatics, 83(7), pp.507
11. Microexcelhealthcare.com. 2021. [online] Available at: microexcelhealthcare. com/pdf/Seoul-NationalUniversity-Case-Study.pdf
12. Statista. 2021. Healthcare data volume globally 2020 forecast | Statista. [online] Available at: statista.com/ statistics/1037970/globalhealthcare-data-volume/
13. Micron.com. 2021. Big Data Can Revolutionize Health Care. [online] Available at: micron.com/insight/ big-data-can-revolutionizehealth-care
Table 1: Examples of Clinical Pathway (CP) implemented in SNUBH
Table 2: Examples of clinical indicators in SNUBH
About the authors
Dr. Hee Hwang
Chief Information Officer and Professor Seoul National University Bundang Hospital
As a professor and the CIO of Seoul National University Bundang Hospital (SNUBH), Dr. Hee Hwang has contributed to both innovations in medical management and developing new business opportunities by converging medicine with ICT. SNUBH is recognized globally as a leading digital hospital since achieving the HIMSS EMRAM Stage7 in 2010 and 2016. As the CIO, he facilitated the development of SNUBH’s next-generation hospital information system (HIS) in 2013. Beyond improving the hospital’s IT environment, he contributed to implementing a standard-based nationwide health information exchange system in South Korea. He conducted to adopt In-Memory based analytics platform into the CDW, enabling real-time analytics of over 500 clinical indicators. He published articles in journals proving the benefit of utilizing Big Data to improve quality of care and patient safety. Throughout his career, he was dedicated to connecting the viewpoints between medical staff and IT professionals, providing intuitive awareness to them.
Joanne Grau
Thought Leadership Manager Digitalizing Healthcare at Siemens Healthineers
Joanne Grau focuses on current trends and thought leadership content for Digitalizing healthcare. Prior to this role, Joanne has had ten years of marketing experience in Siemens Healthineers as marketing director for the diagnostics division based in New York and as Head of Marketing for ASEAN countries based in Singapore. Joanne graduated from UCLA with a degree in Molecular, Cell, and Developmental biology. Before joining Siemens Healthineers, Joanne was a research scientist in Quest Diagnostics (formerly Celera) and has authored multiple publications. Joanne is also currently a faculty member in Union University of California.
Dr. Ralph Wiegner
Global Head of Digitalizing Healthcare at Siemens Healthineers
Ralph Wiegner and his team engage in thought leadership and portfolio-related activities for Digitalizing healthcare. Earlier, he worked as head of Improving patient experience, head of Marketing Strategy and in global key account management. Prior to joining Siemens Healthineers, Ralph worked for several years in the Banking and Asset Management practice of McKinsey & Company on various European and international assignments. Ralph holds a Ph.D. in Theoretical Physics from University of Erlangen, Germany, with several research engagements at the Oklahoma State University, USA.
[1] Adapted from “Turning data into value”, published by Siemens Healthineers, written by Hee Hwang, Joanne Grau, and Ralph Wiegner , in 2021 (Issue 21)
[2] Gwang-seok C. [Special] SNU Bungdang Hospital’s revenue jumps 11 folds in 15 years [Internet]. KBR. 2018 [cited 2021Apr14]. Available from: koreabiomed.com/news/ articleView.html?idxno=3660
[3] Mohw.go.kr. 2021. Ministry of Health & Welfare: Policies Challenges & Tasks Ahead. [online] Available at: mohw.go.kr/eng/pl/pl0103. jsp?PAR_MENU_ ID=1003&MENU_ID=100326
[4] Mohw.go.kr. 2021. Ministry of Health & Welfare: Policies Challenges & Tasks Ahead. [online] Available at: mohw.go.kr/eng/pl/pl0103. jsp?PAR_MENU_ ID=1003&MENU_ID=100326
[5] Seoul National University Bundang Hospital: [Internet]. Seoul National University Bundang Hospital [cited 2021Apr14]. Available from: snubh.org/dh/main/index. do?DP_CD=EN&MENU_ ID=001035
[6] Doctors Feel Excluded from Health Care Value Efforts [Internet]. Harvard Business Review. 2017 [cited 2021Apr12]. Available from: hbr.org/2017/10/doctorsfeel-excluded-fromhealth-care-value-efforts
[7] Diagnostics, Q., 2021. New Study Reveals Stalled Progress Toward Value-Based Care. [online] Prnewswire.com. Available at: prnewswire. com/news-releases/newstudy-reveals-stalledprogress-toward-valuebased-care-300681686.html
[8] Diagnostics, Q., 2021. New Study Reveals Stalled Progress Toward Value-Based Care. [online] Prnewswire.com. Available at: prnewswire. com/news-releases/newstudy-reveals-stalledprogress-toward-valuebased-care-300681686.html
[9] Yoo S, Lee KH, Lee HJ, Ha K, Lim C, Chin HJ, et al. Seoul National University Bundang Hospital’s Electronic System for Total Care. Healthc Inform Res. 2012;18(2):145–52.
[10] Doctors Feel Excluded from Health Care Value Efforts [Internet]. Harvard Business Review. 2017 [cited 2021Apr12]. Available from: hbr.org/2017/10/doctorsfeel-excluded-fromhealth-care-value-efforts
[11] Park, S., Baek, S., Ahn, S., Lee, K., Hwang, H., Ryu, J., Ahn, S., Chin, H., Na, K., Chae, D. and Kim, S., 2018. Impact of Electronic Acute Kidney Injury (AKI) Alerts With Automated Nephrologist Consultation on Detection and Severity of AKI: A Quality Improvement Study. American Journal of Kidney Diseases, 71(1), pp.9–19.
[12] Yoo, S., Hwang, H. and Jheon, S., 2016. Hospital information systems: experience at the fully digitized Seoul National University Bundang Hospital. Journal of Thoracic Disease, 8(S8), pp.S637–S641.
[13] Lim, S., Kang, S., Kim, K., Moon, J., Choi, S., Hwang, H., Jung, H., Park, K., Ryu, J. and Jang, H., 2015. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetologica, 53(2), pp.189–198.
[14] Yoo, S., Kim, S., Lee, K., Jeong, C., Youn, S., Park, K., Moon, S. and Hwang, H., 2014. Electronically implemented clinical indicators based on a data warehouse in a tertiary hospital: Its clinical benefit and effectiveness. International Journal of Medical Informatics, 83(7), pp.507
[15] Yoo, S., Kim, S., Lee, K., Jeong, C., Youn, S., Park, K., Moon, S. and Hwang, H., 2014. Electronically implemented clinical indicators based on a data warehouse in a tertiary hospital: Its clinical benefit and effectiveness. International Journal of Medical Informatics, 83(7), pp.507
[16] Microexcelhealthcare.com. 2021. [online] Available at: microexcelhealthcare. com/pdf/Seoul-NationalUniversity-Case-Study.pdf
[17] Statista. 2021. Healthcare data volume globally 2020 forecast | Statista. [online] Available at: statista.com/ statistics/1037970/globalhealthcare-data-volume/
[18] Yoo, S., Kim, S., Lee, K., Jeong, C., Youn, S., Park, K., Moon, S. and Hwang, H., 2014. Electronically implemented clinical indicators based on a data warehouse in a tertiary hospital: Its clinical benefit and effectiveness. International Journal of Medical Informatics, 83(7), pp.507
[19] Micron.com. 2021. Big Data Can Revolutionize Health Care. [online] Available at: micron.com/insight/ big-data-can-revolutionizehealth-care