the health strategist
platform
the most compreehensive knowledge portal
for continuous health transformation
and digital health- for all
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
December 5, 2023
What is the message?
The article emphasizes the urgent need for the healthcare sector, particularly hospitals and health systems, to take significant actions to reduce greenhouse gas (GHG) emissions and mitigate their contributions to climate change.
It argues that climate change is a critical public health issue and that healthcare leaders have a unique responsibility to address their carbon footprint.
The central message is a call to action for the healthcare industry to prioritize decarbonization efforts and outlines various reasons, benefits, and motivators for hospitals and health systems to engage in such initiatives.
What are the key points?
Health Impacts of Climate Change:
Describes the severe health impacts of climate change, including increased respiratory and cardiovascular diseases, injuries, and premature deaths. Stresses that certain populations, especially historically marginalized communities, are disproportionately affected.
Global Recognition of the Issue:
Highlights the World Health Organization’s declaration of climate change as a defining public health issue and the United Nations Secretary-General’s characterization of the climate crisis as a “code red for humanity.”
Urgency for Action:
Cites warnings from the Intergovernmental Panel on Climate Change about irreversible impacts of global warming and emphasizes the brief window of time available to avoid the worst consequences.
Responsibility of Healthcare Leaders:
Argues that healthcare leaders have a unique duty to address climate change due to the sector’s significant contribution to greenhouse gas emissions.
Current State of Healthcare Sustainability: Notes that the healthcare sector lags behind other industries in sustainability management and disclosures, with calls for mandatory reporting of healthcare emissions gaining traction.
Financial and Business Benefits:
Counters the myth that decarbonization initiatives are costly, providing evidence of positive impacts on financial and business performance, cost savings, risk reduction, and improved corporate performance.
Alignment with High-Value Care:
Proposes that reducing GHG emissions aligns with improving care quality and is considered a fundamental aspect of delivering high-value care.
Societal and Economic Benefits:
Emphasizes the societal benefits of reducing climate-related morbidity and mortality, leading to substantial cost savings in healthcare and beyond.
Health Equity and Economic Benefit:
Highlights the connection between climate change, health equity, and the economic benefits of addressing the climate crisis, especially for vulnerable communities.
Cost Reduction Strategies:
Discusses specific strategies for cost reduction, including energy efficiency, waste reduction, and the use of renewable energy sources.
Employee Recruitment and Retention:
Suggests that decarbonization efforts can enhance recruitment and retention of healthcare workers, particularly among younger generations who prioritize environmental responsibility.
Emergency Management and Resilience:
Stresses the importance of resilience planning to mitigate the impacts of extreme weather events and the economic benefits of such preparedness.
Reputation and Reputational Risk:
Argues that hospitals with transparent and significant decarbonization practices can enhance their reputation and build trust with stakeholders, while the failure to take climate action may pose reputational risks.
External Motivators and Incentives:
Discusses the role of external motivators, incentives, and regulations at the federal and state levels, including tax credits, regulatory requirements, and certification programs.
CMS Influence:
Highlights the potential role of the Centers for Medicare & Medicaid Services (CMS) in driving change by incentivizing or requiring hospitals to measure and report emissions.
State-level Requirements:
Provides examples of state-level laws and requirements related to GHG emissions reporting and energy efficiency measures.
SEC’s Proposed Rule: Discusses the potential impact of the U.S. Securities and Exchange Commission’s proposed rule on strengthening climate disclosure requirements for publicly traded companies.
DEEP DIVE

Crossing the Decarbonization Chasm: A Call to Action for Hospital and Health System Leaders to Reduce Their Greenhouse Gas Emissions
National Academy of Medicine
By Hardeep Singh, Walt Vernon, Terri Scannell, and Kathy Gerwig
November 29, 2023

Introduction
Human activity is warming the climate in unprecedented ways. Climate change is intensifying existing health problems and leading to the emergence of new health threats (Romanello et al., 2023). These impacts include increased respiratory and cardiovascular disease, injuries and premature deaths related to extreme weather events, air pollution and heat waves, changes in the prevalence and geographical distribution of foodborne and waterborne illnesses and other infectious diseases, and negative impacts on mental health (Watts et al., 2020; USGCRP, 2016). The World Health Organization (WHO) has declared climate change to be the defining public health issue of our time, while the United Nations (UN) Secretary-General has called the climate crisis a “code red for humanity” (UN, 2021). The Intergovernmental Panel on Climate Change has warned that many of the impacts of global warming are now irreversible; however, there is “still a brief window of time to avoid the very worst” impacts (Pörtner et al., 2022). Certain populations are being disproportionately affected, including those who belong to historically marginalized communities, such as communities of color, low-income communities, and older adults (Romanello et al., 2022).
All sectors of society must take urgent action to address this threat. The 28th UN Conference of the Parties (COP 28) will host the first-ever dedicated Health Day on December 3, 2023 and is expected to launch a critical call to action, which includes a Declaration on Climate and Health and calls to increase climate financing for health (Ghebreyesus et al., 2023). Within health care, hospital and health care delivery system leaders have a unique duty to take action because their fundamental mission is to provide care, improve health, and do no harm. Given that 8.5% of U.S. greenhouse gas emissions (GHGs) are from health care activities, health care must first be accountable for its own decarbonization, i.e., a broad array of activities that institutions can participate in to reduce their GHG emissions and mitigate their contributions to climate change (Laktos et al., 2023; Eckelman et al. 2020). Health care emissions stem from health care facility operations, purchased energy, supply chain of goods and services, and investments (Eckelman et al., 2020). While health care also needs to adapt to the impact of climate change and improve its resiliency, this paper is primarily a call to action for all health care leaders to take on the responsibility to mitigate emissions from the delivery system organizations they lead.
Building the Case for Hospitals and Health Systems to Reduce GHGs
Currently, U.S. health care lags behind other industries in terms of sustainability management and disclosures (Senay et al., 2022). For instance, >90% of Standard & Poor’s 500 Companies and many private and nongovernmental entities publish annual sustainability reports (Governance and Accountability Institute, 2020). Companies report on their environmental, social, and governance (ESG) performance based on standardized frameworks that provide guidance on organizing, gathering, tracking, and reporting sustainability information using the accounting concept of the triple bottom line—people, planet, profit. This helps quantitatively measure the environmental, social, and financial costs of business operations. But few in health care have adopted this level of accountability and transparency. While selected health care organization pioneers have started to implement new initiatives, standardized and systematic approaches for emissions reporting or mitigation are largely absent. Unsurprisingly, calls for mandatory reporting of health care emissions by all health care organizations are growing (Senay et al., 2022; Singh et al., 2022).
Decarbonization initiatives can no longer be considered aspirational. There is a general myth that such programs may be costly or burdensome. However, evidence increasingly suggests positive impacts on financial and business performance, cost savings, risk reduction, and improved corporate performance (Dancey and Mendiluce, 2023; Senay et al., 2022). Reporting on ESG or emissions may not remain optional anymore, given the increasing external pressures from several stakeholders and rapidly evolving climate crisis. For instance, in December 2021, President Biden signed an Executive Order (EO 14057 Catalyzing Clean Energy Industries and Jobs Through Federal Sustainability) requiring all federal agencies to reduce their impact on the environment and to reduce the impact of climate change (The White House, 2021). Federal agencies were tasked to lead the nation on a path to net-zero emissions by 2050, and all federal health systems—including the Department of Veterans Affairs (VA) that delivers care to nearly 10 million veterans—are impacted. Because there are no such goals or current mandates for private U.S. health care, this call to action lays out a compelling case below for all health care leaders on why they should set similar goals and begin their decarbonization journey (see Figure 1).
High-Value Care
Reduction of GHGs is a fundamental aspect of improving care quality and is often conceived as the seventh dimension of quality, adding to the six domains proposed by the Institute of Medicine (now National Academy of Medicine)—patient safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity (Sherman and Singh, 2023). About one-third of U.S. health care spending is of low value or wasteful, providing a compelling rationale to act (Cafarella Lallemand, 2012).
Many strategies to reduce GHG emissions from hospitals and health systems align with improving quality and are the basis for the delivery of high-value care. For example, several actions to promote decarbonization can potentially reduce the cost of care delivery but also optimize resource consumption, minimize environmental impact, improve patient experience, and improve population health. Examples include placing a greater emphasis on disease prevention and chronic disease management to avoid more complex care that is expensive and environmentally harmful; delivering care in the least energy- or waste-intensive setting, such as using telehealth, primary care, or ambulatory care when appropriate vs. emergency or inpatient care; and minimizing low-value tests, procedures, and treatments that are not only costly but can harm patients.
Societal Benefit
Climate change-related preventable harms to our patients and broadly to the public are now clear. In fact, health damages from U.S. health care pollution were estimated at 388,000 disability-adjusted life years lost in 2018 (Eckelman et al., 2020). According to the American Medical Association principles of medical ethics, physicians should recognize a responsibility to “participate in activities contributing to the improvement of the community and the betterment of public health” and to “seek changes in those requirements which are contrary to the best interests of the patient” (AMA, 2001). By extension, hospitals and health systems have a duty to protect the overall health of their patients and have a moral imperative to act collectively to protect and improve human health. Public health crises, such as climate change, are no exception. In addition, health care leaders employ some of society’s most trusted and respected professionals. Their actions will benefit not only the health of their patients and staff but also surrounding communities and the broader society (AMA, 2022).
In addition, by reducing climate-related morbidity and mortality, there are substantial cost savings to society due to unnecessary health care costs avoided, lost productivity, and human capital benefits. For example, the WHO indicates that climate change impacts globally will cause up to $4 billion in direct health impacts (not including costs of damage due to effects on agriculture, water, and sanitation) annually by 2030 (WHO, 2023). In the United States alone, one report suggests that health costs of air pollution and climate change exceed $800 billion per year and will be higher if there is not a stronger societal response (NRDC, 2021). These costs include doctor visits (for conditions such as heat stress, heat stroke, cardiovascular disease, and respiratory ailments), prescriptions, emergency room visits, physical therapy, allergy treatments, mental health care, and premature death.
According to another recent report, heat event days may lead to almost 235,000 emergency department visits and more than 56,000 hospital admissions for heat-related or heat-adjacent illness, costing health care about $1 billion each summer (Woolf et al., 2023). Climate change also results in additional costs from downstream human capital impacts, such as lost productivity and wages, as well as non-monetary costs, such as pain or suffering and inconvenience to families and others (Ebi et al., 2017). Thus, health care leaders are obligated to mitigate the climate crisis, including addressing their carbon footprint.
Health Equity
Health equity is the first pillar of the Centers for Medicare & Medicaid Services (CMS) Strategic Plan, and other private stakeholders, such as The Joint Commission (TJC), are also making similar commitments. CMS recently finalized a health equity-focused measure for all care settings and all hospitals (CMS, 2022). Health systems are already working on health equity initiatives. Climate change disproportionately affects members of communities of color; low-income communities; people with chronic diseases or disabilities; people with outdoor jobs, such as farm workers; and women, children, and older adults (Phillips, 2022; Romanello et al., 2021). The U.S. Environmental Protection Agency (EPA) found that “Black and African American individuals are 34% more likely to live in areas with the highest projected increases in childhood asthma diagnoses due to climate-driven changes in particulate air pollution. Hispanic and Latino individuals are 43% more likely than non-Hispanic and non-Latino individuals to currently live in areas with the highest projected labor hour losses in weather-exposed industries due to climate-driven increases in high-temperature days,” (EPA, 2021). Additionally, research indicates that pregnant individuals exposed to high temperatures or air pollution are more likely to have children who are premature, underweight, or stillborn. In this case, Black and African American mothers and babies are harmed at a much higher rate than the population at large (EPA, 2021). Residents of rural areas may also be more susceptible to water contamination and power outages after heavy precipitation (Ebi and Hess, 2020; Health Care Without Harm and Arup 2019; Nunn et al., 2019). Thus, activities to reduce the impact of climate change by reducing GHGs are directly in line with the equity mission of hospitals and health systems.
Economic Benefit
While hospitals and health systems may have a responsibility to their patients and communities to take climate action, it is important to recognize the economics that will influence their behavior. Concerns about financial stability are especially salient in the current environment as the country emerges from the impacts of COVID-19. Hospitals and health systems are already facing financial challenges, with over half facing negative margins in 2022 (Mensik, 2022). Surveys of hospital CEOs from the past few years indicate that financial challenges remain a top concern (ACHE, 2022). In this context, it may seem difficult for health care leaders to prioritize decarbonization. However, there are several actions that can generate cost savings related to energy efficiency, and some hospitals and health systems have already implemented these actions. This message needs to be spread through wider use of knowledge-sharing networks and involvement of professional organizations. An initial focus on activities that are more financially rewarding, such as energy-related cost savings, will also help gain more traction in the health sector, generating momentum for future efforts.
Some efforts may not result in immediate cost savings but will be central and beneficial to the interests of hospitals and health systems. Importantly, an exclusive focus on direct cost savings and immediate return on investment does not capture the long-term organizational costs associated with failure to take climate action, including damages from impacts of climate change (e.g., infrastructure/physical damages and costs of care related to harm from weather or wildfire events) and reputational costs.
Costs Associated with Operations
Energy represents a significant portion of a hospital and health system’s expenses, as they operate energy-intensive facilities and consume purchased electricity and fuel, which can contribute to climate change and pollution. Implementing practices such as energy-efficient lighting and heating, ventilation, and air conditioning systems and relying on renewable energy sources can enable hospitals and health systems to reduce energy consumption and save money on utility bills. Moreover, efficiency-enhancing mechanisms could be implemented; for example, clinic space and equipment could be used for longer periods to reduce capital expenses while optimizing the physical space necessary for the same workload. Estimates indicate that as much as 30% of the energy consumed in hospitals and other commercial buildings is used unnecessarily (Schierhorn, 2016). Given that energy is approximately 50% of a facility manager’s budget (i.e., utilities and building management), hospitals can reduce their operating costs by using energy more efficiently (Schierhorn, 2016).
Several exemplars exist. For example, Midland Memorial Hospital in Texas implemented a systematic approach to reducing energy consumption, resulting in $87 million in savings since the hospital began its energy conservation initiative in 2008 (Schierhorn, 2016). Midland Memorial Hospital leveraged a cost-conscious approach of pursuing primarily easy-to-remedy inefficiencies, such as turning off or turning down heating and cooling when and where it wasn’t needed. In addition, Schierhorn writes that the health system “minimized energy-related capital investment by integrating energy conservation into other infrastructure projects,” and incorporated energy conservation best practices into new construction practices (Schierhorn, 2016). Gundersen Health System reached renewable energy independence in 2014 and estimated it saved over $3 million each year as a result (USDA, 2021). Atrium Health in North Carolina implemented several energy efficiency protocols, reducing facility energy consumption by 27% since 2012, reducing their annual energy expenses by $5 million (Atrium Health, 2022). A “Power Down” initiative to turn off all anesthesia and operating room lights and equipment not currently in use saved one health system $33,000 and 234.3 metric tons of CO2 emissions per year (Wormer et al., 2013). Finally, Kaiser Permanente has been certified by CarbonNeutral Protocol as carbon neutral since 2020 because it improved the energy efficiency in its buildings, increased use of on-site solar power, invested in new renewable energy generation, and purchased carbon offsets for currently unavoidable emissions from the natural gas power that heats and cools its hospitals. It was the first health system in the United States to achieve this certification (Kaiser Permanente, 2020).
Costs Associated with Physical Waste (Health Care, Food, and Others)
Hospitals and health systems generate significant amounts of medical and pharmaceutical waste, and disposal fees for such waste are typically higher than that of non-hazardous waste. Addressing waste via enhanced waste segregation strategies, recycling, and reuse can lead to significant cost savings by lowering disposal costs and decreasing the need to purchase new supplies (which would increase resource consumption and related emissions). Reducing waste also helps address the climate change crisis by limiting the amount of waste sent to landfills and the amount of raw materials being used, and reuse reduces the need to order new products.
The operating room is a significant source of waste within the hospital, and thus, efforts to promote sustainability in this setting can generate substantial savings. One study tallied the unused supplies discarded from an OR and estimated that in a single year, one hospital wasted $2.9 million in neurosurgery supplies alone (Zygourakis et al., 2017). Anecdotal self-reported information from 345 hospitals submitting information for Environmental Excellence Awards in 2022 suggests they saved an estimated $157 million on sustainability initiatives in 2021 while reducing more than 19 billion kBTUs of energy, diverting 374 million pounds of waste from the landfill, and avoiding 330,821 metric tons of carbon emissions through mitigation projects (Practice Greenhealth, 2023). The Association of Medical Device Reprocessors reported that medical device users in the United States, Canada, and Europe saved $470 million in 2018 by purchasing reprocessed medical devices rather than new ones and reduced solid waste disposal by 7,100 tons (MacNeill et al., 2020).
Food waste has a cascading environmental impact because it requires more food grown or raised, requires energy and transportation, and has impacts related to methane and carbon dioxide from landfills (Alshqaqeeq et al., 2018). Efforts to reduce patient food waste can also potentially generate substantial cost savings for hospitals and health systems (Hegwer, 2019).
Transportation and Telehealth
Health care leaders can influence choices of transportation and related costs. Low-emission vehicles, such as electric or hybrid vehicles, emit fewer greenhouse gases than traditional vehicles. By using low-emission vehicles for patient transport and supply deliveries, hospitals and health systems can reduce their carbon footprint and potentially achieve cost savings. According to Consumer Reports, consumers who own electric vehicles spend about 60% less each year on vehicle energy costs compared to drivers of gas-powered cars (Harto, 2020). Already, in the United Kingdom, the National Health Service is trialing 21 zero-emission vehicles (ZEVs) of various types, and health care companies have introduced all-electric ZEVs in the United States (Healthcare Dive, 2022; NHS, 2022). The VA is also transitioning its approximately 23,000 vehicle fleet to ZEVs (Sampath et al., 2022).
Another promising strategy to reduce transportation-related emissions associated with patient travel is the broader dissemination of telehealth practices. In one recent study of more than 10 million patients and 63 million virtual care visits, virtual care avoided 3.2 billion kilometers of patient travel, 545 to 658 million kilograms (kg) of carbon dioxide emissions, and $465 to $599 million in expenses for gasoline, parking, or public transit (Welk et al., 2022). Estimates indicate that virtual visits may save 0.70 to 372 kg CO2e (carbon dioxide equivalent) per consultation (Purohit et al., 2021). CommonSpirit estimated that the 1.5 million virtual care visits conducted between March 2020 and April 2021 avoided the equivalent of 15,092 metric tons of carbon dioxide (DOE, 2022). The use of telehealth also presents potential cost savings to both health systems and patients (Patel et al., 2023a; Snoswell et al., 2020). Notably, telehealth offers the potential to enhance access to preventive care and enable patients to see clinicians virtually when they would have otherwise foregone such care (Patel et al., 2023b; Welk et al., 2022). Telehealth could help health systems reduce emissions (and costs) by allowing them to care for more patients without substantial increases in physical space because the number of exam rooms available often limits patient volume in many ambulatory clinics (Thiel et al., 2023).
Employee Recruitment and Retention
A key challenge facing hospital and health system administrators is employee and clinician recruitment and retention. Hospitals and health systems are already facing workforce shortages, and it is critically important to retain existing workers because health care worker attrition can be costly (Frogner and Dill, 2022; Johnson, 2022). A 2020 survey conducted by Nursing Solutions, Inc. reported the average cost of turnover for a bedside registered nurse to be $44,000 and range from $33,000 to $56,000 (Columbia Southern University, 2021). Replacing physicians can be even more expensive, potentially costing an organization between $500,000 and $1 million per physician (Berg, 2018).
Efforts to decarbonize hold promise for improving recruitment and retention. Many employees, particularly younger workers, are looking for employers committed to reducing the impact of climate change. A report by IBM Institute of Business Value in May 2021 found that over two-thirds of respondents believed environmental issues have significant importance to them personally (Bradd, 2021). Climate change and sustainability-related initiatives are considered increasingly important for attracting top talent and employee retention (Apte and Sheth, 2016). While health care has a unique mission of care excellence, one online market research survey highlights the importance of sustainability efforts to job candidates: “one in four respondents reported they would turn down a job offer if the company did not support climate action…nearly 40% of respondents said they would avoid applying to a job if they viewed the company as a climate polluter, and 70% said they are very likely or somewhat likely to depart from a company that does not implement sustainable business practices,” (Grey, 2022).
Maximizing and sustaining a healthy health care workforce is essential to combat the climate crisis and emerging health impacts.
Emergency Management and Resilience Benefits
According to the recent fifth US National Climate Assessment, extreme events cost the US close to $150 billion annually, which is a conservative estimate not accounting for loss of life, health care-related costs, or damages to ecosystem services (USGCRP, 2023). All regions of the United States face some level of risk from extreme weather events, such as extreme heat, wildfires, floods, hurricanes, droughts, or severe winter storms. However, climate change will increasingly worsen the likelihood of extreme weather events, posing risks to human lives and the physical infrastructure of health systems and supply chains (USGCRP, 2018). The Federal Emergency Management Agency estimates that extreme weather events resulting in flooding, fire, or wind damage can cost a hospital anywhere from $600,000 to $2 billion in infrastructure damages, which include both emergency fixes and longer-term recovery efforts such as relocation of critical infrastructure (Thomas, 2011). Facilities that have suffered severe physical damage may be compelled to transfer patients to other locations or temporarily suspend operations altogether, which can lead to additional financial impacts.
The risks of extremely damaging and catastrophic events such as storms or floods are well publicized. Hospitals and health systems that take steps to prepare for the negative impacts of climate change can generate substantial returns on investment by minimizing the risk of future operational disruptions. Relatively small investments not only greatly reduce the costs incurred during an extreme weather event but also provide benefits by avoiding expenses associated with recovery from damage. In 2008, the International Strategy for Disaster Reduction (UN/ISDR), the WHO, and the Global Facility for Disaster Reduction and Recovery (GFDRR) of the World Bank launched a global campaign, “Hospitals Safe from Disasters.” The campaign asserted that incorporating mitigation measures into the design and construction of a new hospital is estimated to account for <4% of the total initial investment, and while retrofitting the hospital’s nonstructural contents (such as windows, doors, AC units, mechanical equipment) costs only 1%, it protects up to 90% of the value (UNDRR, 2008). Importantly, efforts to address resilience can reinforce efforts to promote decarbonization or sustainability. Facilities designed to survive extreme events and prioritize resource (energy and water) efficiency may be able to deliver care more reliably and operate unassisted longer when energy, water, and supply sources are limited or interrupted. Kaiser Permanente, with funding from the California Energy Commission, has deployed renewable energy microgrids as part of the emergency power system for its Richmond and Ontario hospitals in the state of California. These green microgrids that combine solar generation with battery storage have augmented the hospitals’ resiliency while also providing significant financial and emission reduction benefits. Solar energy can also be used for demand reduction and peak shaving (Bliss, 2019).
Reputation and Reputational Risk
While some decarbonization efforts may not be cost saving, they are important to undertake. In particular, hospitals and health systems known for their transparent and significant decarbonization and sustainability practices might be able to enhance their reputation and build trust with their patients, employees, and communities. Transparent reporting of emissions and disclosure of decarbonization initiatives would usher in a new era of public accountability (CDP, 2023). This could potentially lead to increased patient loyalty, better community relations, increased ability to attract funding, and more positive media coverage.
Conversely, failure to take climate action can put hospitals and health systems at a disadvantage. Notably, organizations may face the risk of reduced access to financing and capital as investors increasingly look to ESG performance, risk assessments, and opportunities (Senay et al., 2023; Boyd et al., 2022; Hut, 2022). Protection of physical and social infrastructure requires assessing and addressing risks related to climate change; access to capital, insurance, and finances may be impacted in the absence of these steps (TCFD, 2023). For example, in 2012, after Superstorm Sandy, Moody’s put a medical center’s A3 credit rating under review, citing concerns about delayed recovery of funds from insurers, FEMA, and philanthropists and the potential for decreased patient volume. This would have affected over $750 million in rated debt (Moody’s, 2012). The industry trends are evolving rapidly in this area and will inevitably impact health care. For instance, the International Sustainability Standards Board issued its inaugural standards for 2024, which would bring about a new era of sustainability-related disclosures in capital markets worldwide (IFRS, 2023).
External Motivators and Incentives to Promote Action
Hospitals and care systems around the country are increasingly saving resources by taking action to decarbonize, operate more sustainably, and conduct resilience planning from climate effects. However, it is important to recognize that each health care organization’s unique set of characteristics and context influences why and how it might address climate change. Different states have different energy sources, local policies, and climate-related conditions that will impact whether hospitals in that state decide to prioritize certain actions. For example, use of renewable energy may depend on its accessibility and cost.
For climate action to occur at scale in hospitals and health systems, many extrinsic motivators and incentives will be needed. These include financial and payment incentives to promote essential decarbonization activities, policies and regulations to ensure accountability, new standards, and community-benefit obligations. Additional actions are needed to reduce transportation, health care consumption, and supply chain-related emissions, which constitute the majority of health care emissions (Eckelman et al., 2020).
Recent developments and emerging trends point to the growing importance of external pressures to ensure climate action. The Inflation Reduction Act of 2022 (IRA) could drive change—the IRA greatly expanded tax credits for companies that adopt energy-saving renewable technologies and, importantly, made these credits available to nonprofit organizations, which would include about half of the nation’s hospitals (IRS, 2023). The Bipartisan Policy Center recently released a report outlining several recommendations and federal actions to help hospitals reduce their emissions. It specifically calls on federal agencies such as CMS, CDC, and the Government Accountability Office to implement certain actions (Cristrup et al., 2023).
CMS could play a key role in driving change. As the largest payer in the nation, CMS could incentivize or issue requirements for hospitals and health systems to measure and report emissions and implement emission reduction plans as part of Medicare or Medicaid requirements (Eckelman et al., 2020). CMS influence is already underway. In April 2023, CMS issued a categorical waiver for health care microgrid systems allowing health systems to use clean energy microgrid systems for emergency power generation instead of relying on fossil fuel-powered sources (CMS, 2023). Further, TJC recently launched a voluntary Sustainable Healthcare Certification program for the Hospital and Critical Access Hospital programs to address leadership, measurement, actions, and evaluation related to sustainability (TJC, 2023).
Requirements at the state level include a new law in California, SB 253, which “requires businesses, including hospitals and health care providers, with annual revenue in excess of $1 billion to publicly disclose their direct greenhouse gas emissions and indirect emissions related to electricity, heating, and cooling annually to the California Air Resources Board starting in 2026. Other upstream and downstream indirect emissions need to be reported starting in 2027,” (California Hospital Association, n.d.). Emissions must be reported using the Greenhouse Gas Protocol standards and guidance (Senate Bill No. 253, 2023). Washington State’s Clean Buildings law requires owners of large commercial buildings, including hospitals, to implement energy efficiency measures, determine a compliance pathway, and report to the state in accordance with their compliance schedule (Streeter, 2022).
While nonprofits may not be directly impacted, possible regulatory changes by the U.S. Securities and Exchange Commission (SEC) center around a renewed ESG focus. In June 2022, the SEC proposed a new rule aimed at strengthening climate disclosure requirements for publicly traded companies (SEC, 2022, Senay 2023).
While some of these extrinsic motivators and pressures are still evolving, hospitals and health systems that take action now may be at an advantage over their peers, benefiting from the ability to chart a more comprehensive and pioneering pathway for their institution to address climate change.
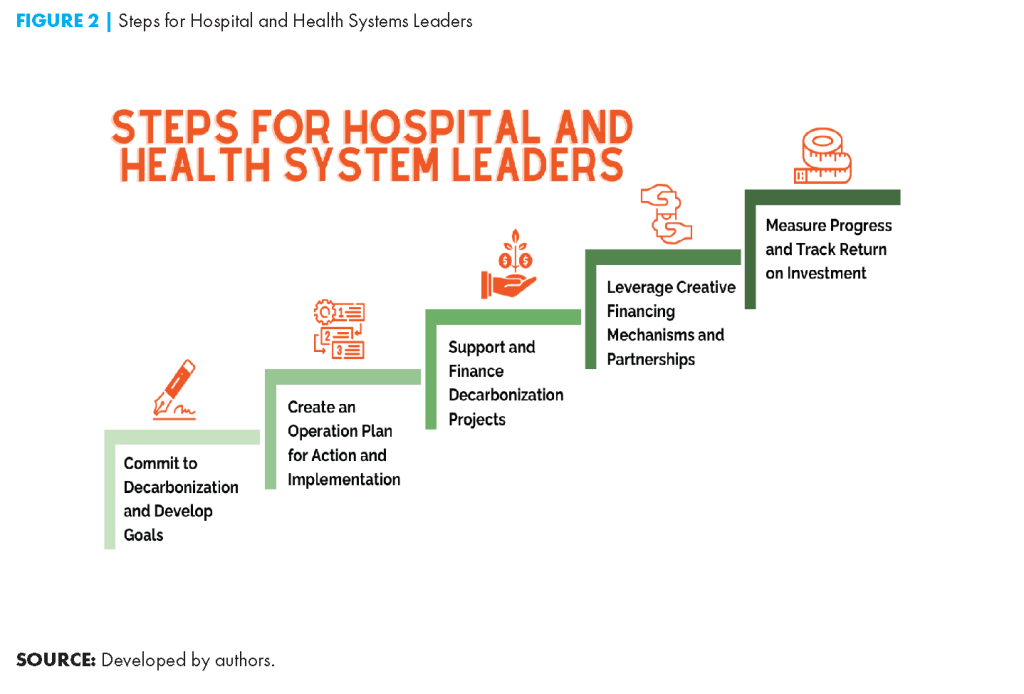
Next Steps for Hospital and Health System Leaders
C-suite leaders and governing board members of hospitals and health systems are critical in implementing decarbonization initiatives. Achieving real progress will require recognition of barriers to such efforts within health care organizations. These include competing priorities, lack of capital to make up-front investments, lack of staff expertise or capacity to implement decarbonization efforts, and cultural barriers (e.g., resistance to change). However, best practices in this space are now available, and to accelerate decarbonization, health care leaders need to help cross the implementation chasm between aspirations and reality (see Figure 2). Several steps summarized here have already been proposed to help hospital and health systems leaders overcome these barriers and promote decarbonization in their organizations (NAM, 2023; Sherman, 2022; Sampath et al., 2022):
- Commit to decarbonization and sustainability. Hospital and health care executive leaders and boards must articulate a transparent vision for climate action and communicate it to staff at all levels. This vision should be adopted as a key organizational priority and incorporated into public-facing statements and organizational strategic plans (Boyd et al., 2021). Goals for achieving emissions reductions should be set and should at least be similar to or more aggressive than the federal goals. The governing board should be involved and oversee the plans.
- Create an operational plan for climate action. Organizations should assess the current state of decarbonization efforts within their own walls, implement transparent measurement and reporting of greenhouse gases, and identify initial priorities based on organizational needs. Leaders should develop an actionable plan to address these priorities. Best practices and guidance on next steps are already available through NAM, the Agency for Healthcare Research and Quality, and other resources (NAM, 2023; Sampath et al., 2022).
- Support and finance decarbonization and sustainability projects. Leaders must ensure adequate staff capacity and financial support to carry out the plans. Staff time needs to be dedicated to work on projects. Certain projects will require initial capital investment before cost savings can be generated over time. Organizations could consider implementing interventions that will save money in the short term, then use savings realized from those interventions to fund future projects with longer time horizons or less direct financial impacts.
- Leverage creative financing mechanisms and partnerships as appropriate. Organizations should consider creative financing mechanisms to cover up-front investments. For example, the Cleveland Clinic established a $7.5 million Green Fund in 2016 to finance investments in energy efficiency. Savings realized from these projects are reinvested into the fund. AAMCNews reported that “initiatives have included an LED retrofit that has reduced electric consumption by 28.6 million kilowatts per year (an annual savings of $2 million) and the installation of systems that shut off lights in unoccupied areas…About one-third of the savings from these efforts have come from operating room improvements” (Budd, 2019). Outside partnerships and collaborative efforts can help hospitals and health systems access initial capital or guidance. For example, the Department of Energy’s Better Buildings Financing Navigator helps public and private sector organizations find financing solutions for energy efficiency and renewable energy projects (DOE, n.d.). The Department of Health and Human Services Office of Climate Change and Health Equity has also developed a compendium of federal resources that may assist health care stakeholders in emissions reduction and climate change adaptation (HHS, 2022).
- Measure progress and track return on investment. Decarbonization efforts should be continuously monitored to assess effectiveness and return on investment. This will help demonstrate the value of such efforts and generate momentum for continued change. In the future, tools such as New York University’s Return on Sustainability Investment (ROSI™) may be used to help quantify the full range of costs and benefits of investment in sustainability; the methodology is currently being deployed to create tools for health systems to analyze potential financial returns of decarbonization strategies (The Commonwealth Fund, 2022).
Conclusion
The case for hospitals and health systems to take urgent action to decarbonize is compelling and has never been stronger. Health care leaders should make climate action a fundamental aspect of their mission and help cross the decarbonization chasm between where we are and where we need to be. In addition to improving care, addressing climate change has societal, financial, and reputational benefits and is essential to addressing health inequities and employee retention. The COP 28 meeting is a watershed moment when health becomes a centerpiece of climate change conversations. Health care leaders must heed this call to action with a robust response.
Originally published at https://nam.edu