This is an excerpt of the publication below, with the title above, focusing on the topic in question.
Nature Medicine
Ani Nalbandian, Kartik Sehgal, …Elaine Y. Wan, et all
22 March 2021
Excerpt by
Joaquim Cardoso MSc.
Health Transformation Institute
continuous transformation
for better health, care, costs and universal health
July 3, 2022
What is the context?
- COVID-19 is now recognized as a multi-organ disease with a broad spectrum of manifestations.
- Similarly to post-acute viral syndromes described in survivors of other virulent coronavirus epidemics, there are increasing reports of persistent and prolonged effects after acute COVID-19.
Overview:
- Early reports suggest residual effects of SARS-CoV-2 infection, such as fatigue, dyspnea, chest pain, cognitive disturbances, arthralgia and decline in quality of life.
- Cellular damage, a robust innate immune response with inflammatory cytokine production, and a pro-coagulant state induced by SARS-CoV-2 infection may contribute to these sequelae.
- Survivors of previous coronavirus infections, including the SARS epidemic of 2003 and the Middle East respiratory syndrome (MERS) outbreak of 2012, have demonstrated a similar constellation of persistent symptoms, reinforcing concern for clinically significant sequelae of COVID-19
Summary of post-acute COVID-19 by organ system
Herein, we summarize the epidemiology and organ-specific sequelae of post-acute COVID-19 and address management considerations for the interdisciplinary.
Pulmonary
- Dyspnea, decreased exercise capacity and hypoxia are commonly persistent symptoms and signs
- Reduced diffusion capacity, restrictive pulmonary physiology, and ground-glass opacities and fibrotic changes on imaging have been noted at follow-up of COVID-19 survivors
- Assessment of progression or recovery of pulmonary disease and function may include home pulse oximetry, 6MWTs, PFTs, high-resolution computed tomography of the chest and computed tomography pulmonary angiogram as clinically appropriate
Hematologic
- Thromboembolic events have been noted to be <5% in post-acute COVID-19 in retrospective studies
- The duration of the hyperinflammatory state induced by infection with SARS-CoV-2 is unknown
- Direct oral anticoagulants and low-molecular-weight heparin may be considered for extended thromboprophylaxis after risk–benefit discussion in patients with predisposing risk factors for immobility, persistently elevated D-dimer levels (greater than twice the upper limit of normal) and other high-risk comorbidities such as cancer
Cardiovascular
- Persistent symptoms may include palpitations, dyspnea and chest pain
- Long-term sequelae may include increased cardiometabolic demand, myocardial fibrosis or scarring (detectable via cardiac MRI), arrhythmias, tachycardia and autonomic dysfunction
- Patients with cardiovascular complications during acute infection or those experiencing persistent cardiac symptoms may be monitored with serial clinical, echocardiogram and electrocardiogram follow-up
Neuropsychiatric
- Persistent abnormalities may include fatigue, myalgia, headache, dysautonomia and cognitive impairment (brain fog)
- Anxiety, depression, sleep disturbances and PTSD have been reported in 30–40% of COVID-19 survivors, similar to survivors of other pathogenic coronaviruses
- The pathophysiology of neuropsychiatric complications is mechanistically diverse and entails immune dysregulation, inflammation, microvascular thrombosis, iatrogenic effects of medications and psychosocial impacts of infection
Renal
- Resolution of AKI during acute COVID-19 occurs in the majority of patients; however, reduced eGFR has been reported at 6 months follow-up
- COVAN may be the predominant pattern of renal injury in individuals of African descent
- COVID-19 survivors with persistent impaired renal function may benefit from early and close follow-up in AKI survivor clinics
Endocrine
- Endocrine sequelae may include new or worsening control of existing diabetes mellitus, subacute thyroiditis and bone demineralization
- Patients with newly diagnosed diabetes in the absence of traditional risk factors for type 2 diabetes, suspected hypothalamic–pituitary–adrenal axis suppression or hyperthyroidism should undergo the appropriate laboratory testing and should be referred to endocrinology
Gastrointestinal and hepatobiliary
- Prolonged viral fecal shedding can occur in COVID-19 even after negative nasopharyngeal swab testing
- COVID-19 has the potential to alter the gut microbiome, including enrichment of opportunistic organisms and depletion of beneficial commensals
Dermatologic
- Hair loss is the predominant symptom and has been reported in approximately 20% of COVID-19 survivors
MIS-C
- Diagnostic criteria: <21 years old with fever, elevated inflammatory markers, multiple organ dysfunction, current or recent SARS-CoV-2 infection and exclusion of other plausible diagnoses
- Typically affects children >7 years and disproportionately of African, Afro-Caribbean or Hispanic origin
- Cardiovascular (coronary artery aneurysm) and neurologic (headache, encephalopathy, stroke and seizure) complications can occur
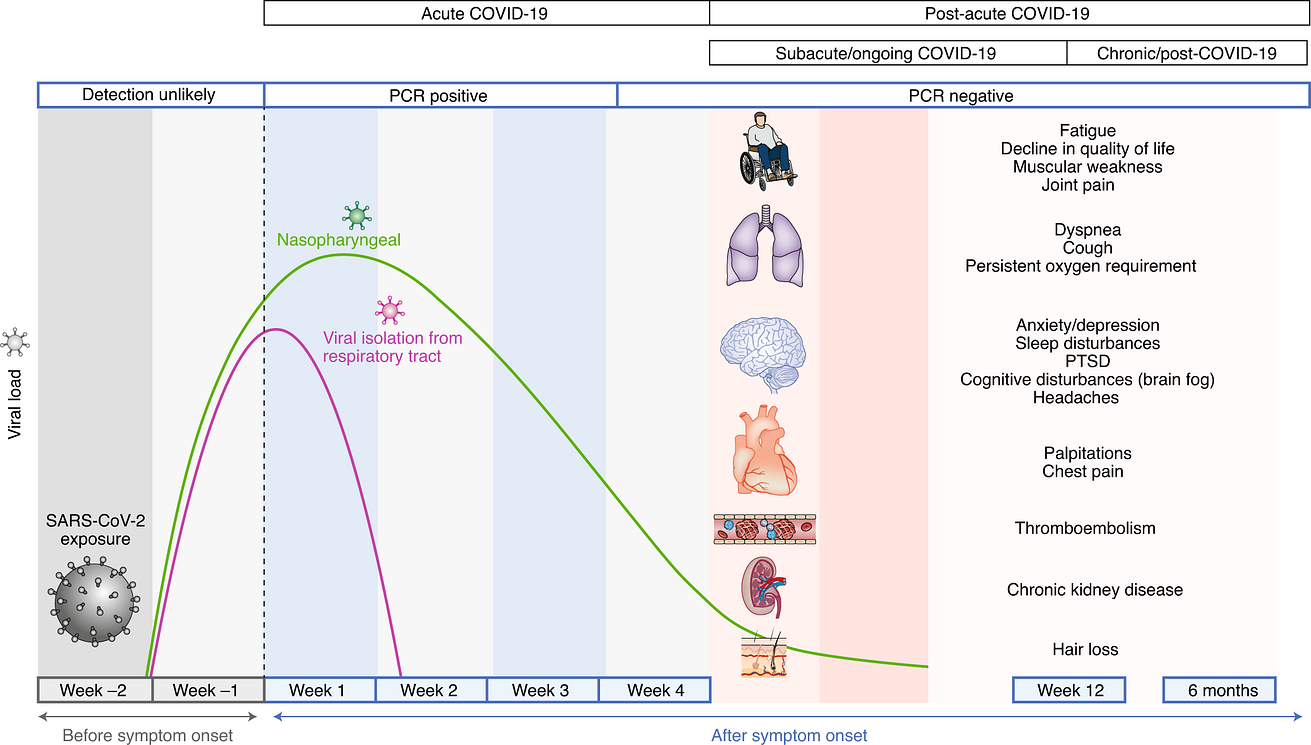
Acute COVID-19 usually lasts until 4 weeks from the onset of symptoms, beyond which replication-competent SARS-CoV-2 has not been isolated.
Post-acute COVID-19 is defined as persistent symptoms and/or delayed or long-term complications beyond 4 weeks from the onset of symptoms. The common symptoms observed in post-acute COVID-19 are summarized.
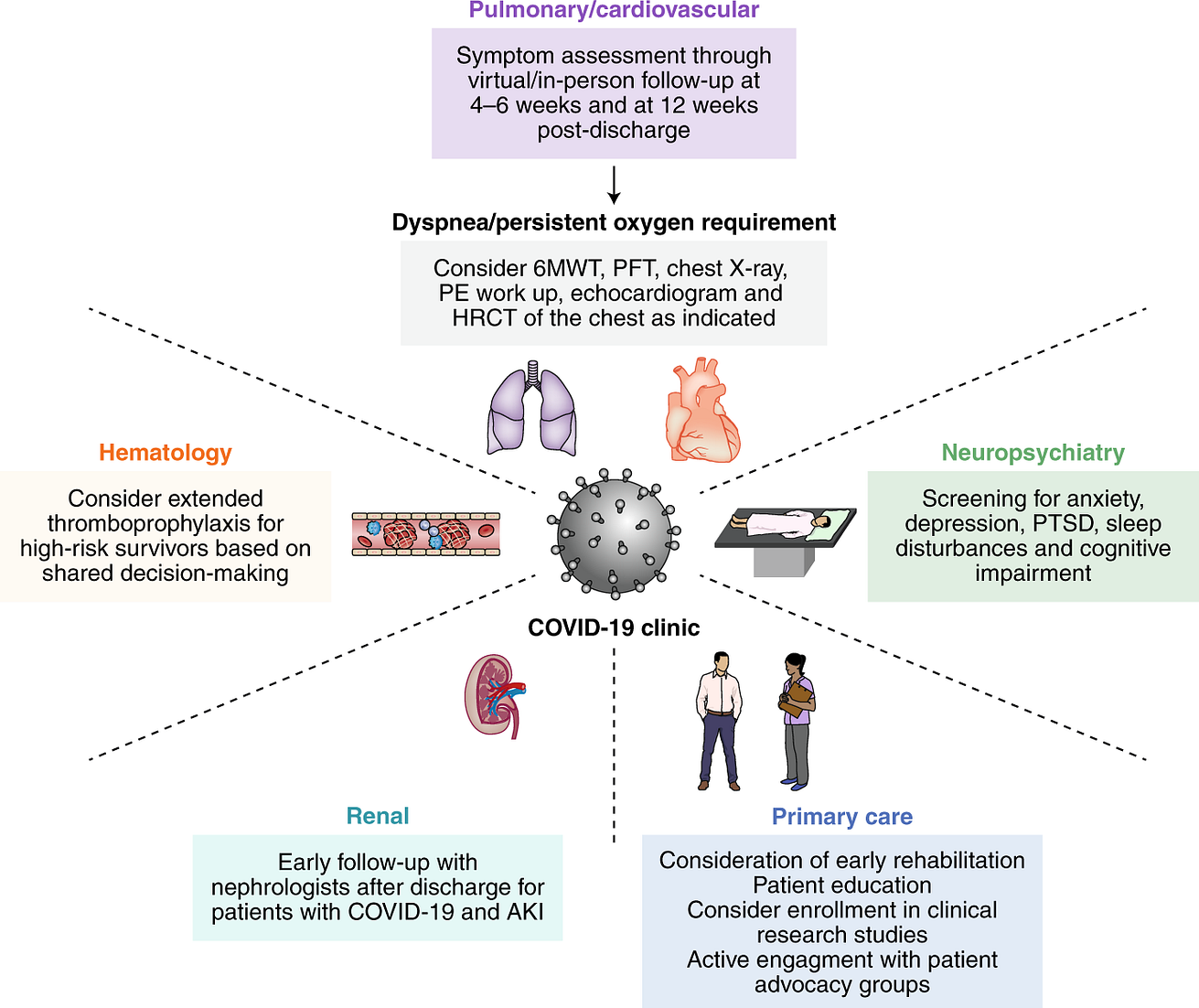
Multidisciplinary collaboration is essential to provide integrated outpatient care to survivors of acute COVID-19 in COVID-19 clinics.
Depending on resources, prioritization may be considered for those at high risk for post-acute COVID-19, defined as those with severe illness during acute COVID-19 and/or requirement for care in an ICU, advanced age and the presence of organ comorbidities (pre-existing respiratory disease, obesity, diabetes, hypertension, chronic cardiovascular disease, chronic kidney disease, post-organ transplant or active cancer).
The pulmonary/cardiovascular management plan was adapted from a guidance document for patients hospitalized with COVID-19 pneumonia76. HRCT, high-resolution computed tomography; PE, pulmonary embolism.
Originally published at https://www.nature.com
RELATED ARTICLES