health and tech
institute
knowledge portal unit
Joaquim Cardoso MSc
Senior Advisor and
Chief Researcher & Editor
January 16, 2023
EXECUTIVE SUMMARY
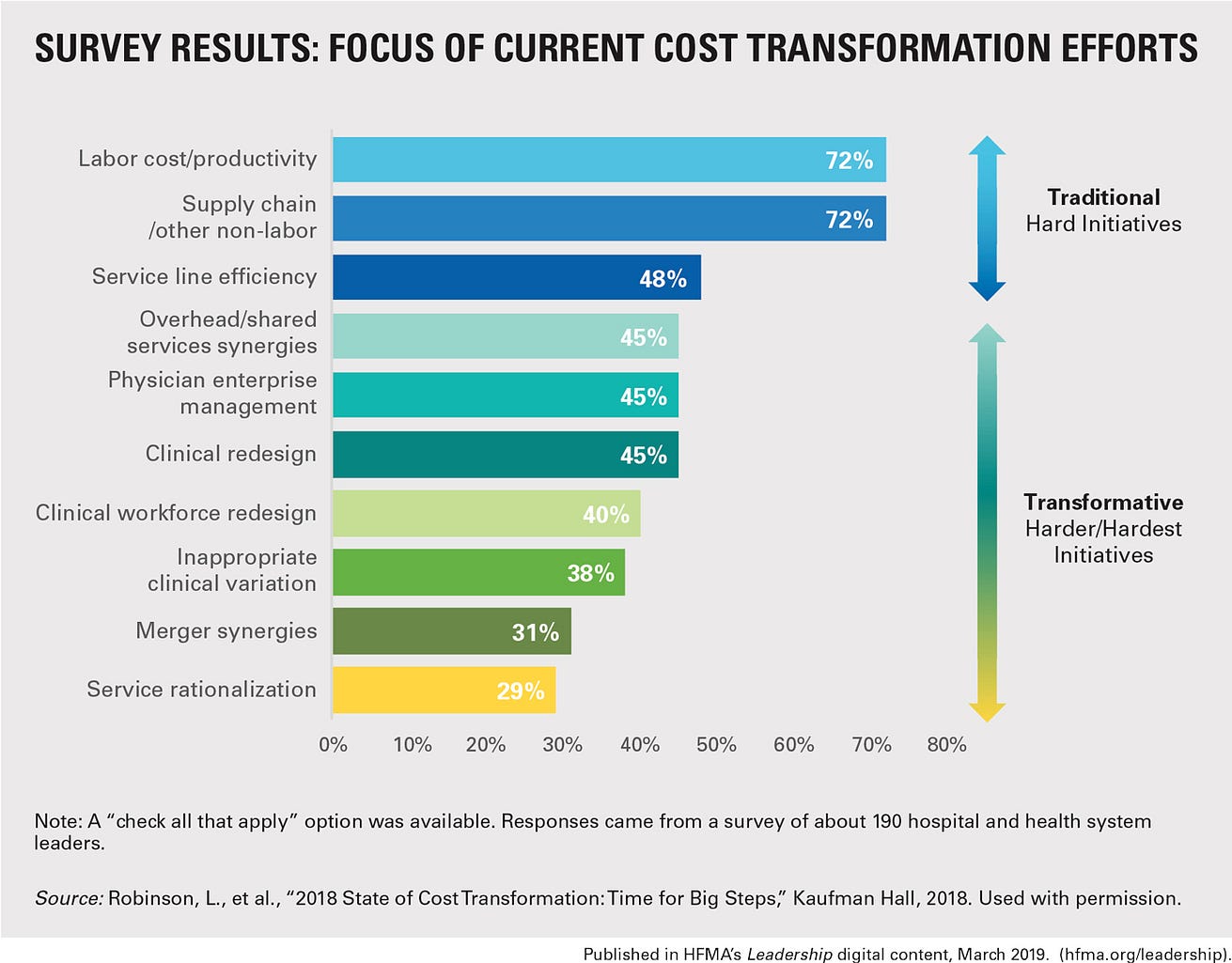
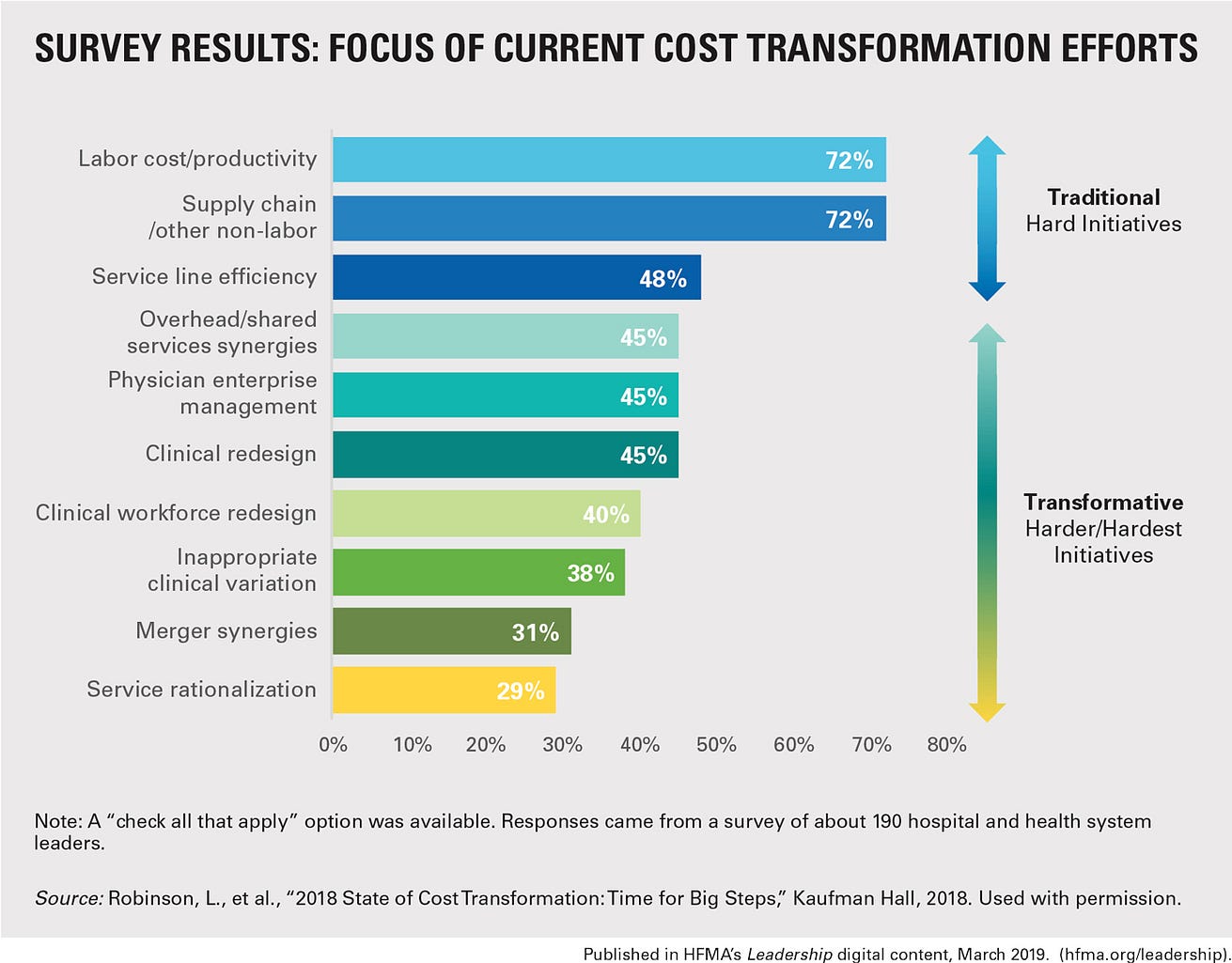
Many healthcare organizations struggle to achieve true cost transformation despite launching processes to identify savings from clinical redesign, service line efficiency, and reduced clinical variation.
- A lack of accountability within the organizational culture is often to blame.
- A survey of nearly 190 senior hospital and health system leaders by Kaufman Hall in 2018 found that over half of the organizations surveyed set cost reduction targets only at the enterprise level, and not at the vice president, service line, or department level.
- Improving leader accountability is key to cost transformation efforts, as it sets leaders on the path towards transformative change.
- One example of this is at Henry Ford Wyandotte Hospital in Michigan, where they have created a variance-comparison spreadsheet tool that includes budgeted and actual expenses, adjusted for volume.
- Clinical leaders can review their operating variances with members of the finance team, senior executives, and their peers to identify cost reduction opportunities, creating accountability and promoting learning.
INFOGRAPHIC

DEEP DIVE

Who Should Own a Healthcare Organization’s Cost Transformation Efforts?
HFMA
Laura Ramos Hegwer
May 15, 2019
Why do so many hospitals’ cost transformation efforts get stuck after leaders have trimmed labor and supply costs?
Often, a lack of ownership within the organizational culture is to blame.
Even after launching formal processes to identify cost savings that can be gained from efforts to promote clinical redesign, improve service line efficiency, and reduce inappropriate clinical variation, many hospitals are unable to achieve true cost transformation.
The reason: They lack an infrastructure that fosters accountability among leaders at every level, says Lance Robinson, managing director and leader of Kaufman Hall’s Performance Improvement practice in Chicago.
“What we have found is that accountability often stops at the C-suite,” Robinson says.
In fact, more than half of nearly 190 senior hospital and health system leaders surveyed by Kaufman Hall in 2018 say their organizations set cost reduction targets only at the enterprise level-not at the vice president, service line, or department level. 1
The reason: They lack an infrastructure that fosters accountability among leaders at every level,… “What we have found is that accountability often stops at the C-suite,”
… more than half of nearly 190 senior hospital and health system leaders surveyed by Kaufman Hall in 2018 say their organizations set cost reduction targets only at the enterprise level-not at the vice president, service line, or department level
Yet when a sense of accountability pervades an organization’s culture, it can set leaders on the path toward transformative change.
Owning Efforts to Address Operating Variances
Improving leader accountability is at the heart of recent cost transformation efforts at Henry Ford Wyandotte Hospital in Wyandotte, Mich.
“We wanted to create an environment where our clinical leaders and nonclinical leaders have greater ownership of the business operations in their departments,” says Peter Karadjoff , former interim president.
“Finance can’t hold these leaders accountable-the organization has to decide that it will hold them accountable.”
“We wanted to create an environment where our clinical leaders and nonclinical leaders have greater ownership of the business operations in their departments,” …
“Finance can’t hold these leaders accountable-the organization has to decide that it will hold them accountable.”
To instill a greater sense of ownership among leaders, Karadjoff partnered with the finance team and an outside consultant to create a homegrown, variance-comparison spreadsheet tool that includes budgeted and actual expenses, adjusted for volume.
Using the tool, clinical leaders can review their operating variances with members of the finance team, senior executives, and their peers to identify cost reduction opportunities.
Clinical leaders with variances are invited to meetings (biweekly for payroll variances, monthly for variances in supplies and other expenses) to explain their variance in front of their peers, which creates accountability and promotes learning.
“What we hold them accountable for is putting in a solid effort to develop a data-driven answer and to engage their financial support partners,” Karadjoff says.
Clinical leaders with variances are invited to meetings (biweekly for payroll variances, monthly for variances in supplies and other expenses) to explain their variance in front of their peers, which creates accountability and promotes learning.

Promoting Collaboration
Initially, the tighter working relationship between clinical and finance leaders created some anxiety among both groups, given that they were being pulled outside their comfort zones, Karadjoff says.
But those concerns have faded as they have worked together to meet their targets. “They have learned a lot from each other, and their capabilities have grown tremendously,” he says.
The finance team can develop credibility with clinical leaders by helping them apply data-driven approaches to improve their quality performance as well, says Karadjoff, who is now senior vice president of performance excellence at Trinity Health in Livonia, Mich.
This work can help finance leaders sustain buy-in from clinical leaders for cost transformation efforts.
The finance team can develop credibility with clinical leaders by helping them apply data-driven approaches to improve their quality performance as well
Henry Ford Wyandotte leaders also have partnered with independent medical staff to improve throughput and reduce length of stay (LOS).
Physicians are paired with nurse leaders in dyad teams to identify strategies for improving throughput, such as by streamlining patient movement between levels of care and conducting physician rounding earlier in the day.
In early 2018, leaders trimmed 1,760 excess patient days from the geometric mean LOS in just over three months, cutting approximately $1 million of operating expense, Karadjoff says.
In early 2018, leaders trimmed 1,760 excess patient days from the geometric mean LOS in just over three months, cutting approximately $1 million of operating expense, Karadjoff says.
Top-Cited Impediments to Achieving Cost Transformation Goals

Continuing the Push for Change
When rolling out cost transformation initiatives, Robinson says, leaders should be deliberate about which projects they select.
The priorities should be those that are likely to deliver the greatest impact on financial and quality outcomes.
That approach can help combat the “change fatigue” associated with many cost-reduction strategies and prevent staff from quickly losing interest.
“You want to create a culture of engagement and change around your efforts,” Robinson says. “This can help ensure that the transformation is sustained over time.”
When rolling out cost transformation initiatives, Robinson says, leaders should be deliberate about which projects they select.
The priorities should be those that are likely to deliver the greatest impact on financial and quality outcomes.

Footnote
1. Robinson, L., et al., “2018 State of Cost Transformation: Time for Big Steps,” Kaufman Hall, 2018.
Laura Ramos Hegwer is a freelance writer and editor based in Lake Bluff, Ill.
Interviewed for this article:
Peter Karadjoff, FACHE, former interim president, Henry Ford Wyandotte Hospital, Wyandotte, Mich., and now senior vice president of performance excellence, Trinity Health, Livonia, Mich.;
Lance Robinson, managing director and leader of Kaufman Hall’s Performance Improvement practice, Chicago.
Originally published at https://www.hfma.org on May 15, 2019.












