modern health
institute
for continuous health transformation
& digital health strategy
Joaquim Cardoso MSc.
Founder and CEO
Chief Research and Strategy Officer (CRSO) —
for the Research & Strategy Institute
Chief Editor — for the Knowledge Portal; and
Independent Senior Advisor — for the Advisory Consulting Unit
September 18, 2023
What is the message?
- From 2013 to 2019 the share of U.S. health care visits delivered by non-physicians such as nurse practitioners or physician assistants increased from 14 to 26 percent.
- This rapid shift requires caregivers, medical educators, and policymakers to understand and manage this growing segment of the health care workforce.
- The research is the first nationally representative study of the share of health care delivered by nurse practitioners and physician assistants, collectively known as advanced practice providers.
Infographic
Fig 1
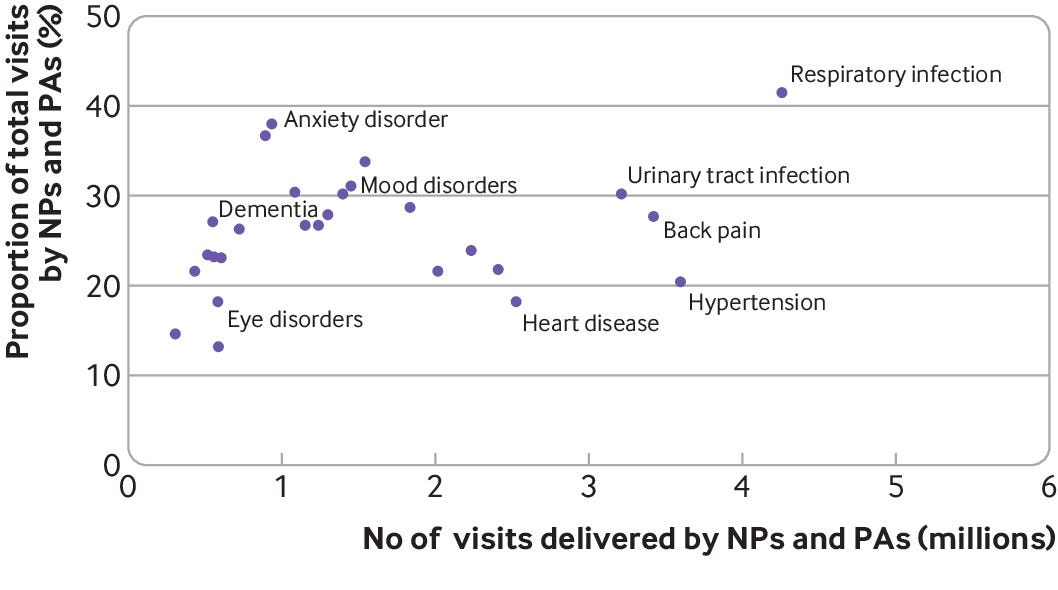
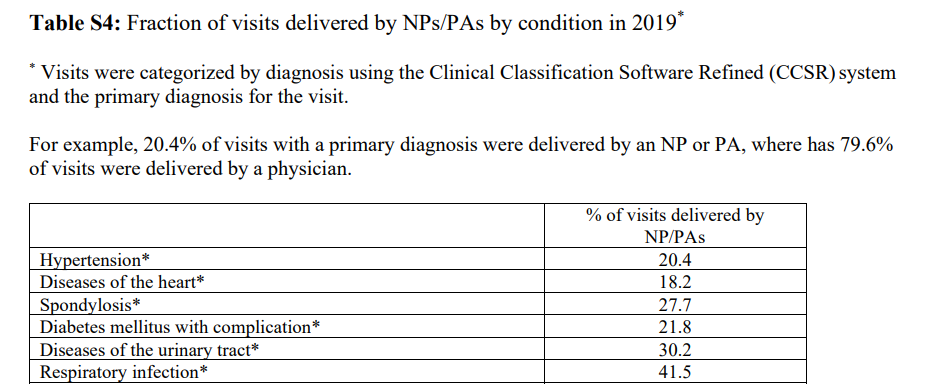
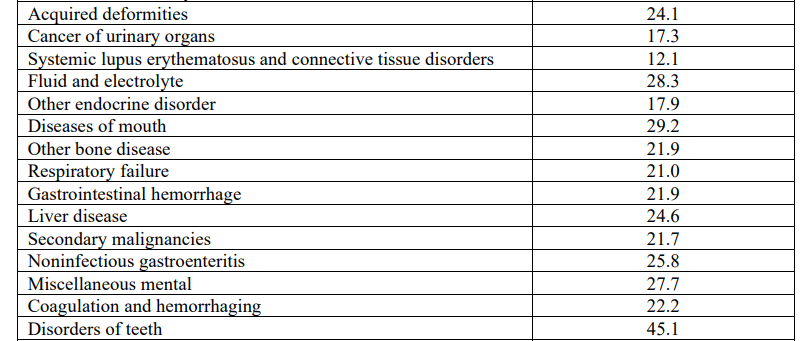
Trends in the number of nurse practitioner (NP) and physician assistant (PA) visits per patient, the percentage receiving any NP or PA visit, and fraction of total visits delivered by NPs and PAs, 2013–19
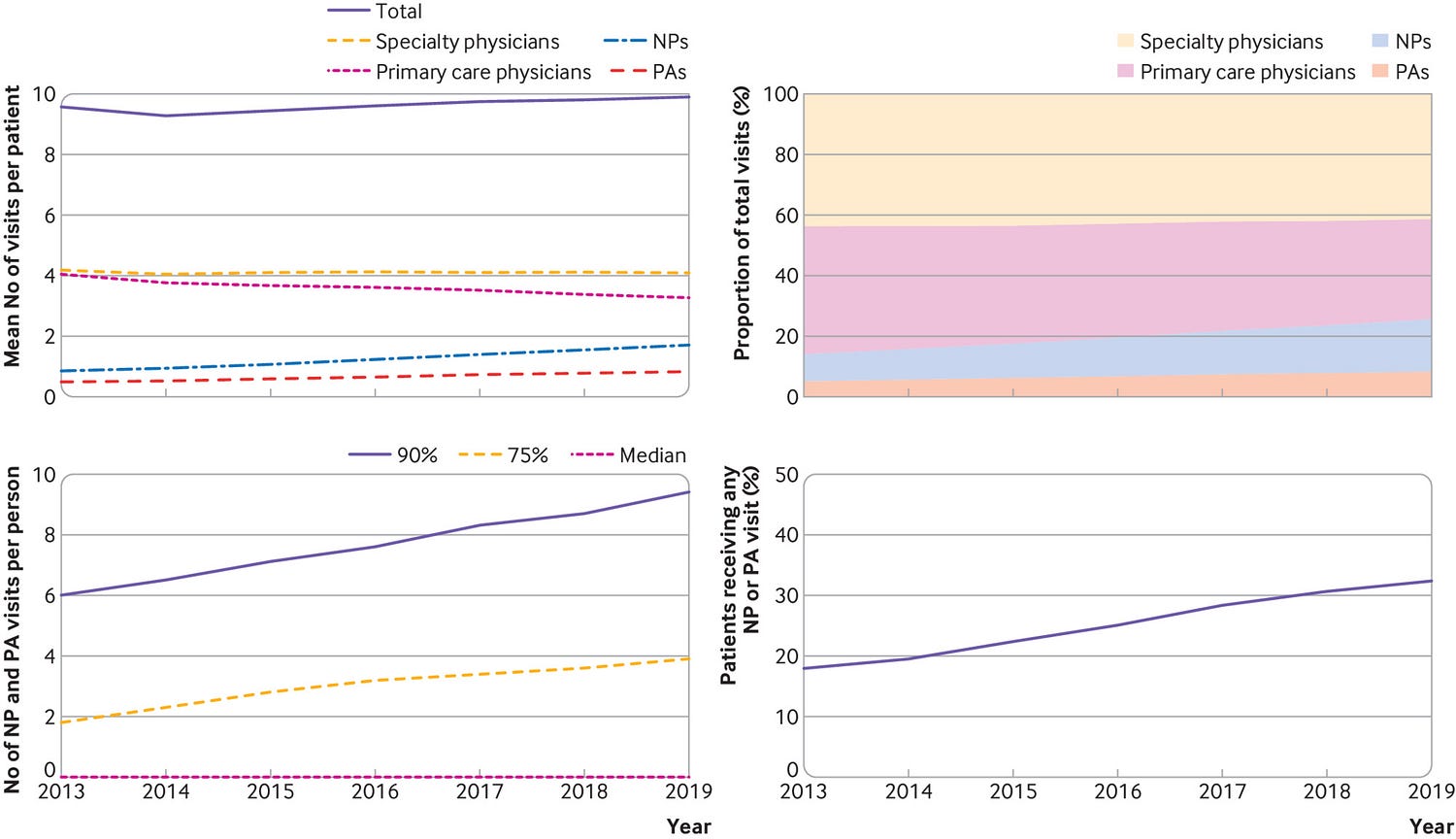
Fig 2
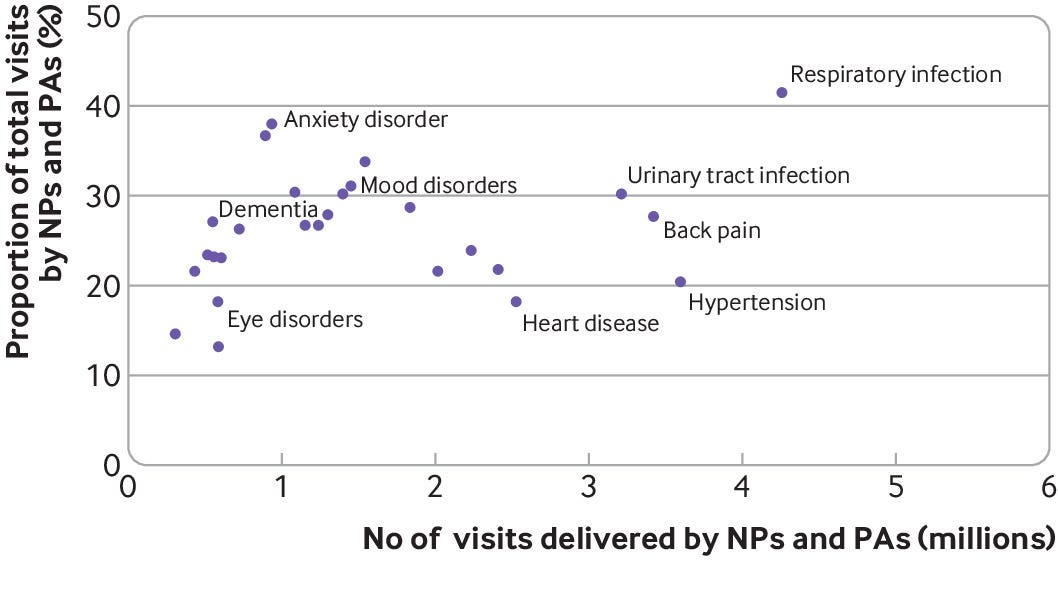
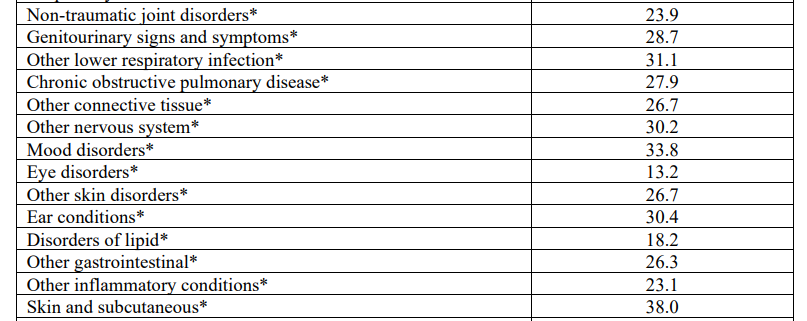
Trends in the mean number of nurse practitioner (NP) and physician assistant (PA) visits by setting from 2013 to 2019 and relative growth in NP and PA visits from 2013 by setting.
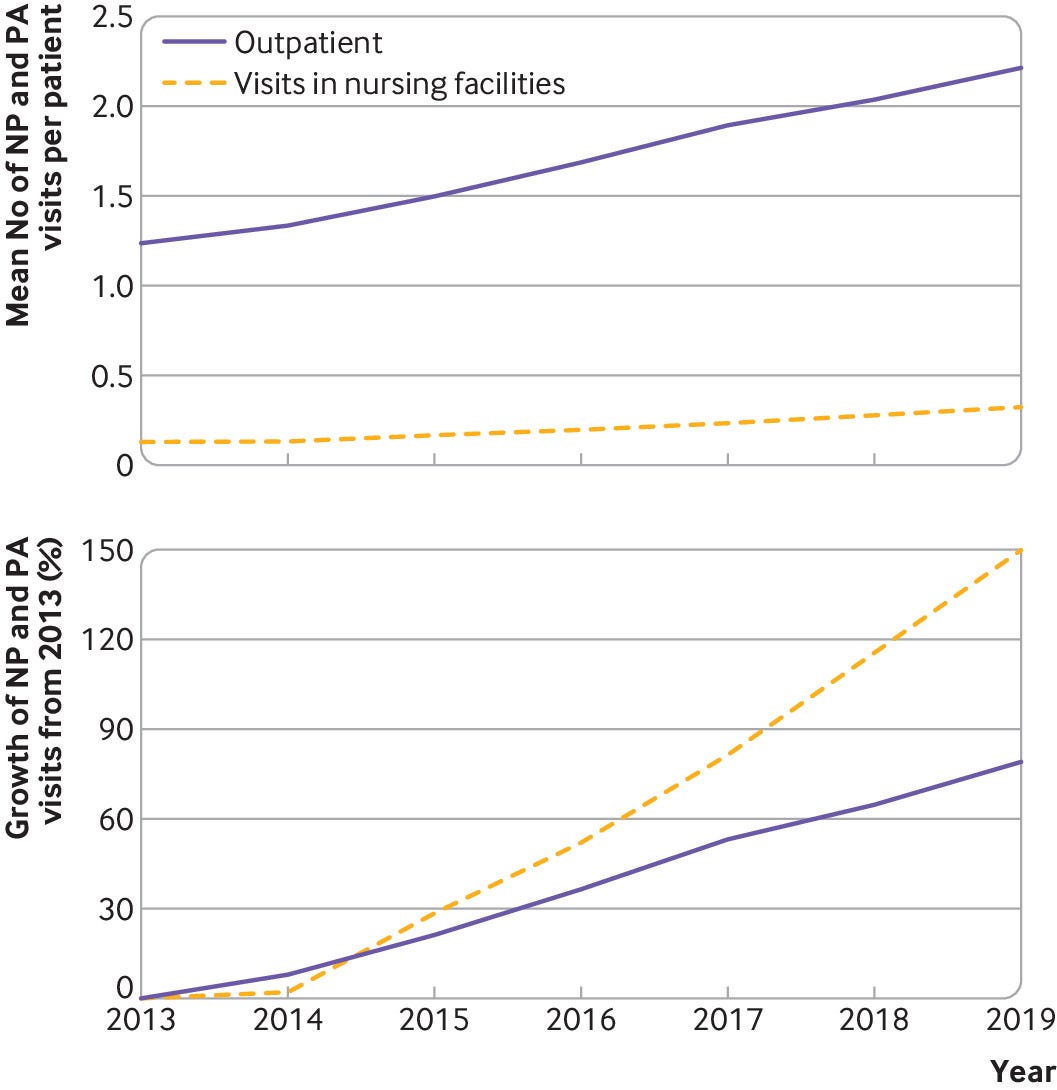
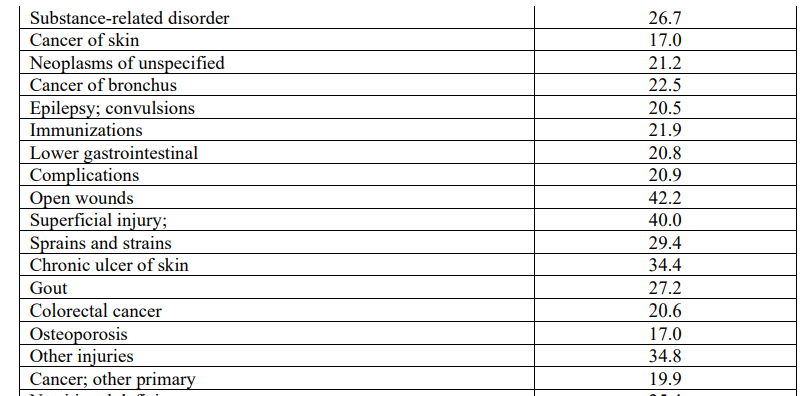
Fig 4
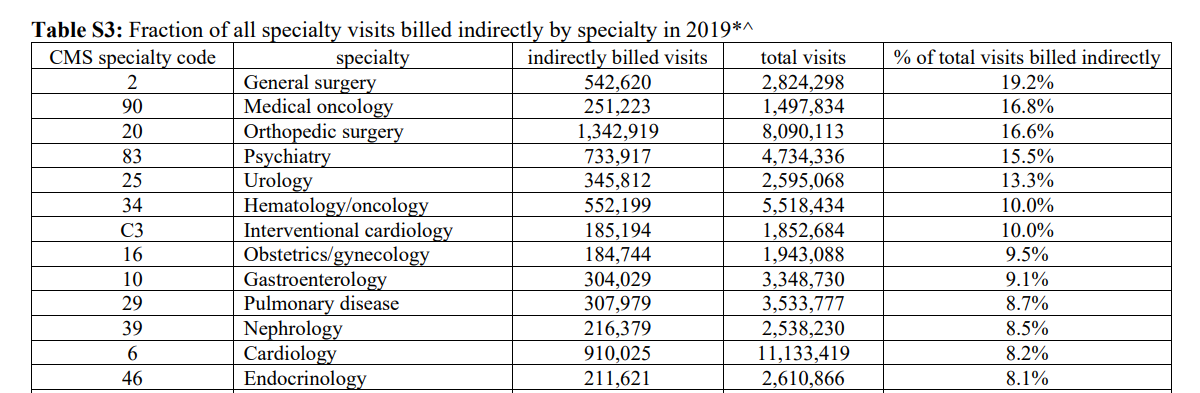
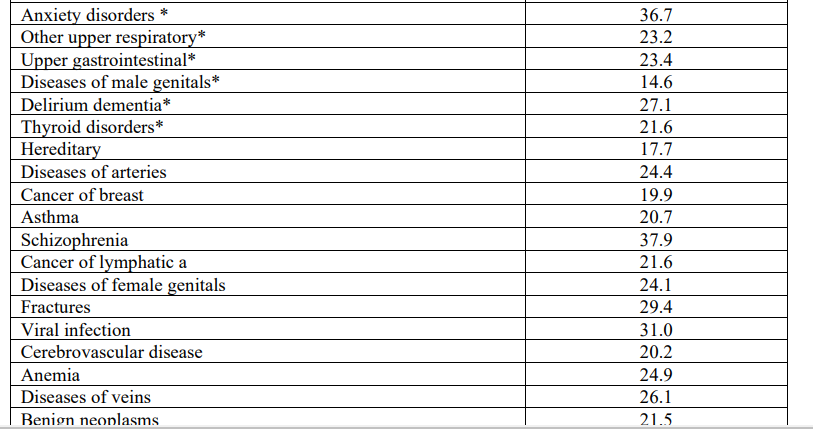
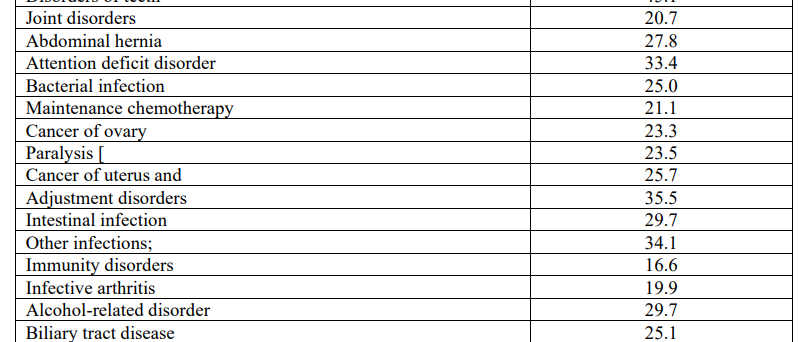
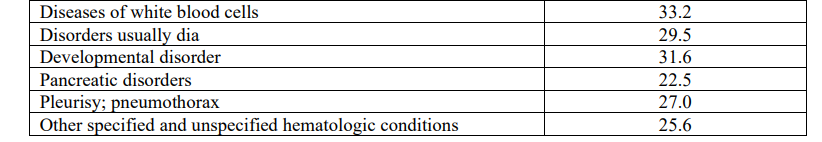
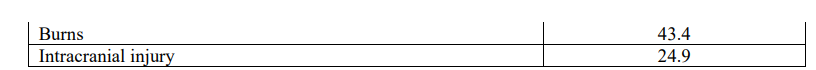
Proportion of total visits delivered by nurse practitioners (NPs) and physician assistants (PAs) for each condition by percentage of total visits for each condition in 2019.
DEEP DIVE

Harvard Medical School
By JAKE MILLER
September 14, 2023
Health care provided by nurse practitioners and physician assistants expected to rise as their ranks grow faster than physicians’
The proportion of health care visits delivered by nurse practitioners and physician assistants in the U.S. is increasing rapidly and now accounts for a quarter of all health care visits, according to a study published Sept. 14 in the BMJ.
The analysis, led by researchers from the Department of Health Care Policy in the Blavatnik Institute at Harvard Medical School, highlights the rising importance of this rapidly growing segment of the U.S. health care system.
The research is the first nationally representative study of the share of health care delivered by nurse practitioners and physician assistants, collectively known as advanced practice providers. It is also the first study to look at care delivered across different clinical conditions.
The researchers analyzed 276 million visits from a nationally representative sample of Medicare insured patients.
Study co-authors Ateev Mehrotra, professor of health care policy at HMS, and Sadiq Patel, a former NIH postdoctoral fellow at HMS, spoke with Harvard Medicine News about the increasingly important role these providers play in our health care system.
That’s the average, but it varied across different conditions.
- 47% of respiratory infection visits and
- 31 % of visits for anxiety disorders were conducted by nurse practitioners and physician assistants,
- but it was only 13 % for eye disorders and
- 20 % for hypertension.
The U.S. Bureau of Labor Statistics estimates that between 2019 and 2031
- the number of nurse practitioners in the U.S. will increase by 80 percent and
- the number of physician assistants by nearly 50 percent.
In contrast, the growth rate for physicians over the next decade or so is estimated at
- less than 5 percent.
That’s another reason it’s so important to get this right.
We’ve known that these groups often have greater difficulty accessing care, and nurse practitioners and physician assistants are critical to providing this access.
Most of the research agrees that all three professions can do a good job delivering care in most settings, especially primary care.
And it turns out that there is not a significant difference in spending. But there are clinical conditions that might be better suited to one profession or another.
The high use of nurse practitioners and physician assistants for anxiety disorders is another interesting example.
There simply aren’t enough psychiatrists to treat all the people who need care for mental health conditions.
But the good news is that there are highly effective evidence-based treatments that can help a lot of people with depression and anxiety that do not require a physician to deliver.
This interview was edited for length and clarity.
Originally published at https://hms.harvard.edu on September 14, 2023.
Names mentioned
Ateev Mehrotra, professor of health care policy at HMS, and
Sadiq Patel, a former NIH postdoctoral fellow at HMS,
Reference Publication (excerpt version)
Provision of evaluation and management visits by nurse practitioners and physician assistants in the USA from 2013 to 2019: cross-sectional time series study
BMJ 2023; 382 doi: https://doi.org/10.1136/bmj-2022-073933 (
Published
14 September 2023)
Abstract
Objective To examine the proportion of healthcare visits are delivered by nurse practitioners and physician assistants versus physicians and how this has changed over time and by clinical setting, diagnosis, and patient demographics.
Design Cross-sectional time series study.
Setting National data from the traditional Medicare insurance program in the USA.
Participants Of people using Medicare (ie, those older than 65 years, permanently disabled, and people with end stage renal disease), a 20% random sample was taken.
Main outcome measures
- The proportion of physician, nurse practitioner, and physician assistant visits in the outpatient and skilled nursing facility settings delivered by physicians, nurse practitioners, and physician assistants,
- and how this proportion varies by type of visit and diagnosis.
Results
- From 1 January 2013 to 31 December 2019, 276 million visits were included in the sample.
- The proportion of all visits delivered by nurse practitioners and physician assistants in a year increased from 14.0% (95% confidence interval 14.0% to 14.0%) to 25.6% (25.6% to 25.6%).
- In 2019, the proportion of visits delivered by a nurse practitioner or physician assistant varied across conditions, ranging from 13.2% for eye disorders and 20.4% for hypertension to 36.7% for anxiety disorders and 41.5% for respiratory infections.
- Among all patients with at least one visit in 2019, 41.9% had one or more nurse practitioner or physician assistant visits.
- Compared with patients who had no visits from a nurse practitioner or physician assistant, the likelihood of receiving any care was greatest among patients who were lower income (2.9% greater), rural residents (19.7%), and disabled (5.6%).
Conclusion
- The proportion of visits delivered by nurse practitioners and physician assistants in the USA is increasing rapidly and now accounts for a quarter of all healthcare visits.

What is already known on this topic?
- An increasing number of nurse practitioners and physician assistants provide care in the US and many other countries, but little work has characterized the care that they provide
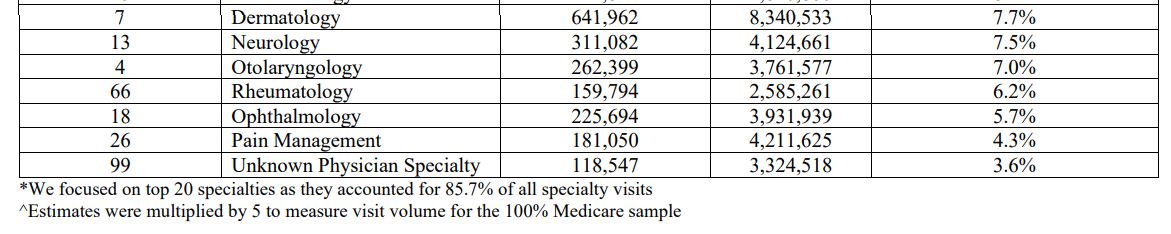
- Quantifying the care provided by nurse practitioners and physician assistants has been hampered in the US by the use of indirect billing, where the bill is submitted under a supervising physician
- Research that only examined visits directly billed by a nurse practitioners or physician assistants substantially underestimates their involvement in the US health care system and conversely overestimates the involvement of physicians
What this study adds?
- From 2013 to 2019, the proportion of all traditional healthcare visits delivered by nurse practitioners and physician assistants increased from 14.0% to 25.6%
- For some clinical conditions, such as respiratory infections, nurse practitioners and physician assistants provide a larger proportion of healthcare visits
- Our results highlight the rapidly growing involvement of nurse practitioners and physician assistants in the US

Introduction
The number of nurse practitioners and physician assistants is increasing in the United States of America. From 2019 to 2031, the Bureau of Labour Statistics estimates that the number of nurse practitioners will increase from 200 000 to 359 000 (80 percent growth), whereas the number of physician assistants will increase from 120 000 to 178 000 (48 percent growth).1 However, to date, quantifying the proportion of care and the type of care provided by nurse practitioners and physician assistants has been hampered by the use of indirect billing (also called incident-to or shared visit billing). With indirect billing, the nurse practitioner or physician assistant provides most of the care for a patient but the bill for the service is submitted under a supervising physician.2 A novel method, published in 2022, described how to identify indirect billing visits and estimated that nationally between 2010 and 2018, 44% of all nurse practitioner and physician assistant visits in the US were billed indirectly.3 Therefore, prior research that only examines the visits directly billed by an nurse practitioner or physician assistant substantially underestimates their involvement in the US health care system and conversely overestimates the involvement of physicians.34
To better characterise the involvement of nurse practitioners and physician assistants in the US health care system, we identified indirect billing in traditional Medicare claims to estimate the proportion of visits delivered by nurse practitioners and physician assistants and how this varied by clinical setting and diagnosis and by patient demographics.3 We also characterize which patients are more likely to receive care from an nurse practitioner or physician assistant.
Methods & Results
See the original publication
Discussion
Principal findings
From 2013 to 2019, the proportion of all visits delivered by nurse practitioners and physician assistants to people enrolled on the traditional Medicare program increased from 14.0% to 25.6%. In 2019, the proportion of total visits delivered by a nurse practitioner or physician assistant varied substantially, ranging from 13.2% for eye disorders to 41.5% for respiratory infections. Consistent with prior literature,2728 concurrent with the growth in nurse practitioner and physician assistant visits, primary care physician visits per patient per year decreased by 18%. Among all patients who had at least one visit, 42% had at least one visit with a nurse practitioner or physician assistant and the likelihood of receiving any care from a nurse practitioner or physician assistant was greatest among patients with lower incomes, residing in rural areas, and who are disabled.
Comparison with other studies
Our estimate of 25.6% visits provided by a nurse practitioner or physician assistant is consistent with a prior study examining primary care visits in a single electronic health record system, which found 27.2% were provided via a nurse practitioner or physician assistant.4 Our study extends this work by looking at visits on a national scale, across all clinical specialties, and by clinical condition.
These results illustrate the rapidly growing involvement of nurse practitioners and physician assistants in the US health care system. The proportion of care provided by nurse practitioners and physician assistants will likely only increase over time because substantially more new nurse practitioners and physician assistants are entering the workforce compared with physicians.1 Although Americans have historically seen a physician as their usual clinician, increasingly that usual clinician will now be a nurse practitioner or physician assistant.29 One survey indicated that 54% of Americans had difficulty differentiating between the role of the nurse practitioner and the physician with varying opinions about differences in qualifications.29 This confusion may increase in the future given the shift of some nurse practitioner education programs to doctor of nursing practice degrees,30 which means that some nurse practitioners may also be called doctors.
However, our results do not support the idea that nurse practitioners and physician assistants are simply replacing physicians in a one-to-one fashion. Rather, clinicians are complementing each other with nurse practitioners and physician assistants having a greater focus on some types of visits, possibly where their training and expertise is best suited. Across conditions, we observe substantial differences in the involvement of nurse practitioner and physician assistants with higher involvement in low acuity acute problems (eg, respiratory infections and urinary tract infections) and mental illness, and a lesser role for heart disease and eye disorders. Compared with nurse practitioners and physician assistants, primary care physicians are more likely to provide new patient visits and less likely to provide annual exams. Surprisingly, we found that in areas of the US with fewer physician visits per capita, fewer numbers of nurse practitioner and physician assistant visits were recorded. We hypothesize that this finding reflects a shift to team based care and that nurse practitioners and physician assistants often practice alongside physicians. Our findings echo prior work in which substantial variation has been reported in the role of nurse practitioners and physician assistants in multidisciplinary teams across patient counseling, educational services, and the provision of primary care.31323334 A large body of research has directly compared nurse practitioners and physicians on the quality of care and spending. Although exceptions exist,35 in general, many studies have found similar quality and spending.36373839404142 One criticism of this published literature is that these studies make direct comparisons of clinicians with different training. We believe more research is needed to understand how nurse practitioners and physician assistants are integrated into practice, and if configurations are optimal in terms of the mix of clinicians on the quality and efficiency of care delivered.36373839404142
Our results also show that younger patients who are more likely to be disabled or have lower income and those who live in rural areas are more likely to receive care from a nurse practitioner or physician assistant. Nurse practitioners and physician assistants are also increasingly involved in care for older patients in nursing facilities. Taken together, these results suggest that nurse practitioners and physician assistants provide more care to underserved communities in the US.
Among industrialized countries, the US is in an outlier in that it has fewer physicians per capita.67 Our results highlight that the US has addressed this relative shortage through a growing reliance on nurse practitioners and physician assistants. Nurse practitioners and physician assistants now work in many other countries (appendix),67 and the trends we observe in the US could inform other countries because they consider how to address their own clinician shortages.
Limitations
Our study has several important limitations. Firstly, we cannot directly link a prescription to a given visit. We assumed that a prescription that was filled within a one day window around a visit was associated with that visit. However, we acknowledge that some misclassification is possible where the nurse practitioner or physician assistant writes prescriptions on behalf of the physician who provided care and where physicians write prescriptions on behalf of the nurse practitioner or physician assistant who provided care. Secondly, we limited our analysis to people who were enrolled in the traditional Medicare program with Part D coverage (roughly 47% of all people enrolled in Medicare) and therefore, may not be generalizable to other populations in the US health care system including those enrolled in Medicaid, commercial insurance, and Medicare Advantage programs. The latter may be particularly important, because during the study period enrollment in Medicare Advantage increased significantly.43 Third, we focused only on visits delivered by physicians, nurse practitioners, and physician assistants and did not include visits from many other clinicians, such as social workers and psychologists. Fourth, our method of identifying indirect billing visits necessarily focuses on visits with an associated prescription, and we then extrapolate the patterns observed in those visits to all visits through an inverse probability weighting procedure. Neither our method of linking prescriptions to visits nor our weighting procedure is perfect, and this may bias our findings. For example, if nurse practitioners and physician assistants prescribed at higher rates than physicians, our estimates for rates of nurse practitioner and physician assistant visits would be too high. Conversely, if physicians prescribed at higher rates than nurse practitioners and physician assistants, our estimates would be too low. We do not know the direction or magnitude of such a bias. Fifth, a limitation of administrative claims is the nurse practitioner and physician assistant specialisation is not generally specified and therefore we cannot describe the relative importance of different types of nurse practitioner and physician assistant training (for example, those with expertise in mental health, primary care, or obstetric care). Sixth, we used the primary diagnosis on the visit to categorize visits, but this diagnosis may not always accurately reflect the reason for the visit.
Conclusions
Despite these limitations, we believe our results provide the best available estimate of the involvement of nurse practitioners and physician assistants in the US health care system.
In summary, we found that from 2013 to 2019, the fraction of all traditional Medicare visits delivered by nurse practitioners and physician assistants increased from 14.0% to 25.6%.
Our results highlight the rapidly growing involvement of nurse practitioners and physician assistants in the US.
Future research is needed to understand the implications of this growth on the quality of care that Americans receive.
About the authors & affiliations:
- Sadiq Y Patel, postdoctoral research fellow1,
- David Auerbach, senior director7,
- Haiden A Huskamp, professor1,
- Austin Frakt, professor2 5 6,
- Hannah Neprash, assistant professor8,
- Michael L Barnett, associate professor2 4,
- Hannah O James, doctoral student9,
- Laura Barrie Smith, research associate10,
- Ateev Mehrotra, professor1 3
- 1Department of Health Care Policy, Harvard Medical School, Boston, MA, USA
- 2Department of Health Policy and Management, Harvard T H Chan School of Public Health, Boston, MA, USA
- 2Department of Health Care Policy, Harvard Medical School, Boston, MA, USA
- 3Division of General Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA
- 4Division of General Internal Medicine and Primary Care, Department of Medicine, Brigham and Women’s Hospital, Boston, MA, USA
- 5Boston University School of Public Health, Boston, MA, USA
- 6Veterans Affairs Boston Healthcare System, Boston, MA, USA
- 7Massachusetts Health Policy Commission, Boston, MA, USA
- 8Division of Health Policy and Management, University of Minnesota School of Public Health, Minneapolis, MN, USA
- 9Department of Health Services, Policy and Practice, Brown University School of Public Health, Providence, RI, USA
- 10Health Policy Center, Urban Institute, Washington, DC, USA
Appendix