In anticipation of the next novel infectious disease, The World Obesity Federation urge governments and health service providers to adopt the policies outlined in the ROOTS Call for Action.
The Health Strategist
the blog of Joaquim Cardoso MSc
October 10th, 2021
This is a brief article, based on the Executive Summary of the report in the 2nd part of this post.
Key messages (1 Page Summary):
What is the problem?
- Obesity is recognised as both a disease in its own right and a condition that increases the likelihood of developing a wide range of non-communicable diseases.
- Less well-known is the fact that obesity also increases the likelihood that infectious diseases will lead to serious consequences. This is most clearly apparent in the global spread of the SARS-CoV-2 virus and the resulting pandemic of COVID-19.
- An overweight population is an unhealthy population, and a pandemic waiting to happen.
What is the cost of obesity during Covid-19 (human & financial) ?
- Of the 2.5 million COVID-19 deaths reported by the end of February 2021, 2.2 million (88%) were in countries where more than half the population is classified as overweight.
- … up to a third of the (pandemic) costs (33%) — between $6 trillion and $7 trillion over the longer period — might be attributable to these predisposing risks (lack of physical activity and excess body weight);
What is the importance of fighting obesity?
- Obesity is a disease that does not receive prioritisation commensurate with its prevalence and impact, which is rising fastest in emerging economies.
- It is a gateway to many other noncommunicable diseases and mental-health illness and is now a major factor in COVID-19 complications and mortality.
- There is a window of opportunity to advocate for, fund and implement these actions in all countries to ensure better, more resilient and sustainable health for all, now and in our postCOVID-19 future.
What is the opportunity?
- The COVID-19 pandemic has shown that a societal, worldwide response to a disease is possible.
- COVID-19 has also exposed the imperative to address other global health challenges such as obesity.
- Evolving evidence on the close association between COVID-19 and underlying obesity provides a new urgency — and inspiration — for political and collective action.
What are the recommendations?
In anticipation of the next novel infectious disease, we (The World Obesity Federation) urge governments and health service providers to adopt the policies outlined in our ROOTS Call for Action.
- R — Recognise that obesity is a disease in its own right as well as a risk factor for other conditions, including significantly worsening the outcomes of COVID-19 infection.
- O — Obesity monitoring and surveillance must be enhanced to strengthen effective strategies for preventing and treating obesity.
- O — Obesity prevention strategies must be developed, tested and implemented across the life course, from pre-conception, through childhood, and into older age.
- T — Treatment of obesity — including behavioural, pharmacological, digital, nutritional, physicalactivity based and surgical interventions — should be accessible to all people with obesity.
- S — Systems-based approaches should be applied to the treatment and prevention of obesity. In the recovery from COVID-19 we call for action across the following systems: (1) Health; (2) Food; (3) Transport; (4) Water and sanitation and (5) Education
Editor
Joaquim Cardoso, MSc
ORIGINAL PUBLICATION
______________________________________________________________
COVID-19 and Obesity: The 2021 Atlas
The cost of not addressing the global obesity crisis
World Obesity.Org
March 2021
Executive Summary
Obesity is recognised as both a disease in its own right and a condition that increases the likelihood of developing a wide range of non-communicable diseases.
Less well-known is the fact that obesity also increases the likelihood that infectious diseases will lead to serious consequences.
This is most clearly apparent in the global spread of the SARS-CoV-2 virus and the resulting pandemic of COVID-19.
Through detailed analyses of the latest peer-reviewed data, we demonstrate how overweight is a highly significant predictor of developing complications from COVID-19, including the need for hospitalisation, for intensive care and for mechanical ventilation.
Overweight is also a predictor of death from COVID-19.
This report shows that in countries where less than half the adult population is classified as overweight[1], the likelihood of death from COVID-19 is a small fraction — around one tenth — of the level seen in countries where more than half the population is classified as overweight.
Of the 2.5 million COVID-19 deaths reported by the end of February 2021, 2.2 million (88%) were in countries where more than half the population is classified as overweight.
Of the 2.5 million COVID-19 deaths reported by the end of February 2021, 2.2 million (88%) were in countries where more than half the population is classified as overweight.
We recognise that these figures are by necessity incomplete, and that a clearer picture may emerge as the pandemic develops further.
The figures are affected by the ability of a country to control its borders and by the speed with which the virus and its variants spread through populations and into more remote areas.
Patterns of the disease will change as some counties vaccinate their populations more rapidly than others. Nonetheless, our findings have serious public health implications.
The figures are affected by the age structure of national populations and a country’s relative wealth and reporting capacity, but our findings appear to be independent of these contributory factors.
Furthermore, other studies have found that overweight remains a highly significant predictor of the need for COVID-19 health care after accounting for these other influences.
- The International Monetary Fund has calculated that COVID-19 will cause a total of at least $10 trillion losses in global output over the period 2020–2021,
- and accumulating to $22 trillion over the period 2020–2025.
- Based on the UK experience, where an estimated 36% of COVID-19 hospitalisations have been attributed to lack of physical activity and excess body weight (Hamer, Kivimati et al 2020),
- it can be suggested that up to a third of the costs (33%) — between $6 trillion and $7 trillion over the longer period — might be attributable to these predisposing risks.
… up to a third of the (pandemic) costs (33%) — between $6 trillion and $7 trillion over the longer period — might be attributable to these predisposing risks.
COVID-19 is not the first respiratory viral infection exacerbated by overweight.
Data from the last two decades on the impact of MERS, H1N1 influenza and other influenza-related infections show worse outcomes linked to excess bodyweight.
An overweight population is an unhealthy population, and a pandemic waiting to happen.
An overweight population is an unhealthy population, and a pandemic waiting to happen.
In anticipation of the next novel infectious disease, we urge governments and health service providers to adopt the policies outlined in our ROOTS Call for Action described on page 7.
In anticipation of the next novel infectious disease, we urge governments and health service providers to adopt the policies outlined in our ROOTS Call for Action
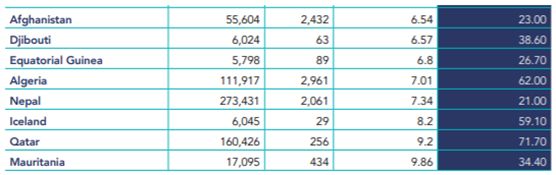
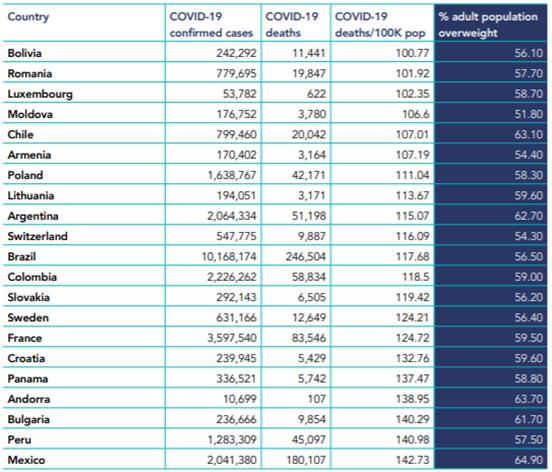
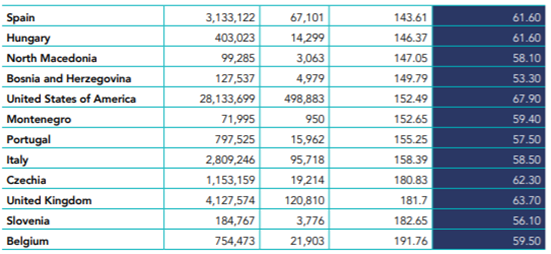
Countries with lowest and highest rates of death from COVID-19 compared for their adult overweight prevalence.
Sources: COVID-19 reported deaths, Johns Hopkins Coronavirus Resource Center, (downloaded Feb 23 2021), and WHO Global Health Observatory adult overweight estimates.
Low COVID death rates
All countries reporting fewer than 10 deaths due to COVID-19 per 100,000 population
For the large majority, under half of adults are living with excess weight.
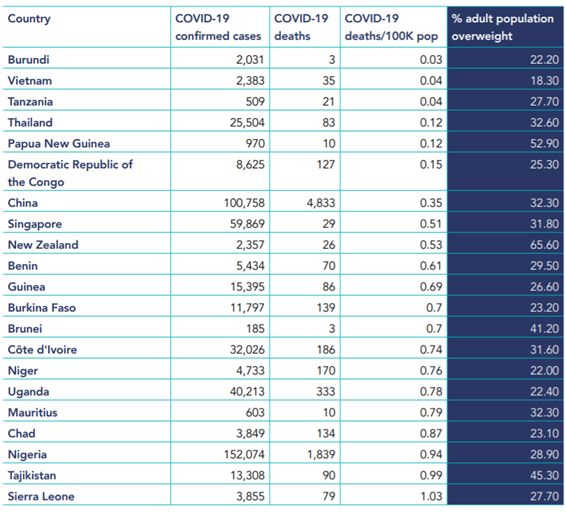
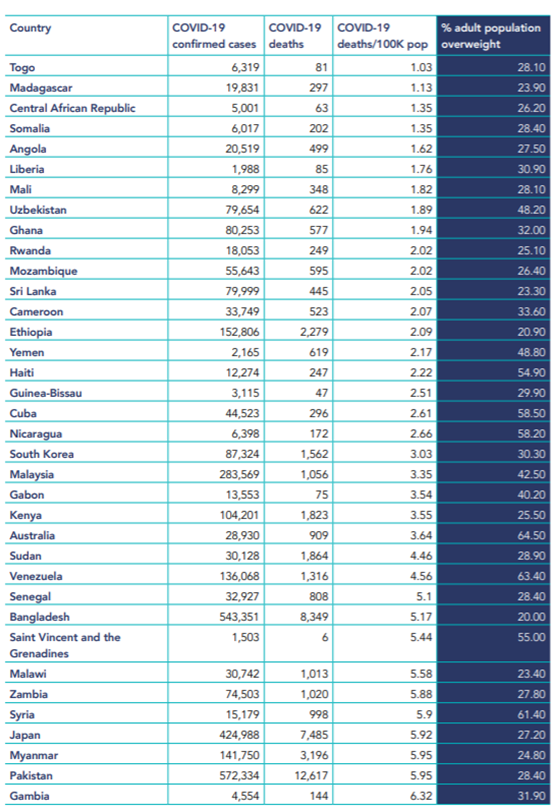
High COVID death rates
All countries reporting more than 100 deaths due COVID-19 per 100,000 population (i.e. more than one death per thousand population)
For every country, more than half of adults are living with excess weight.
World Obesity Federation’s ROOTS: A Call for Action
Obesity and the response to COVID-19
Building stronger economies by investing in health
The COVID-19 pandemic has shown that a societal, worldwide response to a disease is possible.
COVID-19 has also exposed the imperative to address other global health challenges such as obesity.
Evolving evidence on the close association between COVID-19 and underlying obesity provides a new urgency — and inspiration — for political and collective action.
Obesity is a disease that does not receive prioritisation commensurate with its prevalence and impact, which is rising fastest in emerging economies.
It is a gateway to many other noncommunicable diseases and mental-health illness and is now a major factor in COVID-19 complications and mortality.
There is a window of opportunity to advocate for, fund and implement these actions in all countries to ensure better, more resilient and sustainable health for all, now and in our postCOVID-19 future.
This Declaration is inspired by calls from the World Health Organization, the United Nations and the OECD to ‘build back better’ from COVID-19, to improve the health of people and the planet.
It reflects a consensus reached at the 2020 Global Obesity Forum.
A ROOTS approach
On World Obesity Day 2020, the global obesity community came together to acknowledge the complexity of obesity and to develop the ROOTS framework, which sets out an integrated, equitable, comprehensive and person-centred approach to addressing obesity.
Building on the ROOTS framework, this Declaration sets out recommendations for immediate action across the obesity spectrum from prevention to treatment, within the context of COVID-19:
R
Recognise that obesity is a disease in its own right as well as a risk factor for other conditions, including significantly worsening the outcomes of COVID-19 infection. We call for:
- people living with obesity to be included among the groups prioritised for testing and vaccination;
- spaces in which people living with obesity receive COVID-19 care to be appropriately equipped, with trained health workers free from weight bias, who have knowledge on the complexity of obesity and obesity care needs;
- the recognition that, in many contexts, COVID-19 and obesity are linked through inequity/health disparities, and strategies to address both diseases should adopt a social determinants of health approach.
O
Obesity monitoring and surveillance must be enhanced to strengthen effective strategies for preventing and treating obesity. We call for:
- population-wide monitoring to assess how COVID-19 has affected the risk factors for and prevalence of obesity;
- monitoring of availability and accessibility to nutritionally adequate food supplies, especially among populations vulnerable to COVID-19 including those with obesity;
- monitoring the impact of policies and restrictions to limit the spread of COVID-19 for their impact on people with obesity;
- monitoring of compliance with the international code and resolutions on marketing of breastmilk substitutes, as there is evidence of violations occurring.
O
Obesity prevention strategies must be developed, tested and implemented across the life course, from pre-conception, through childhood, and into older age. We call for:
- primary and secondary obesity prevention efforts to be continued and enhanced for all without discrimination, as a critical means to increase population resilience to pandemics;
- co-creation and implementation of policies to reduce childhood obesity, working with young people and acknowledging that, for many children, COVID-19 control measures have increased risk;
- equity-based obesity prevention strategies focusing on populations most affected by the syndemic interactions between COVID-19, poverty and race.
T
Treatment of obesity — including behavioural, pharmacological, digital, nutritional, physicalactivity based and surgical interventions — should be accessible to all people with obesity. We call for:
- routine obesity treatment and management services not to be restricted during COVID-19, but instead invested in and prioritised to enhance equitable access;
- development of novel treatment strategies (for example, tele-medicine) to include solutions co-created with the participation of people living with obesity, including those with ‘long’ COVID.
S
Systems-based approaches should be applied to the treatment and prevention of obesity. In the recovery from COVID-19 we call for action across the following systems:
- Health: Cost-effective community-based prevention, including monitoring and screening should be integrated with clinical pathways for secondary prevention, obesity management and treatment.
- Food: National and local government-led action and incentives to pivot food systems towards sustainable growth models, focusing on ‘triple win’ policy solutions to address the Global Syndemic of over- and undernutrition and climate change.
- Transport: Investment in active transport systems to promote physical and mental health, while reducing COVID-19 transmission risk and mitigating climate change.
- Water and sanitation: Universal access to clean water, especially in countries where sugar-sweetened beverages may be more widely available than safe drinking water.
- Education: Provision of nutritious school meals, particularly for socioeconomically disadvantaged children, and the replacement of such meals when schools are closed; increased physical education. • Economic: Novel investment from global health donors and multilateral institutions to address the rising cost of obesity in lower income countries.
[1] The term ‘overweight’ is used here to mean adults with a body mass index (BMI) above 25 kg/m2, a widely recognised threshold indicating an increased risk of developing weight-related chronic diseases. ‘Obesity’ is classified as a BMI above 30 kg/m2. In some texts the term ‘overweight’ is used to mean a BMI between 25 and 30 kg/m2 (i.e. ‘overweight non-obese’).
Originally published at https://www.worldobesity.orgCOVID-19 and Obesity: The 2021 Atlas | World Obesity Federation
Our new report released for World Obesity Day 2021, analysing the cost of not addressing the global obesity crisis.www.worldobesity.org