This is a republication of the article below, with the title above, by the Editor of this Blog — Joaquim Cardoso MSc.
Hidden waits — The lasting impact of the pandemic on children’s services in the community (UK, NHS)
Over 900,000 children and adults are waiting for services as part of a community services care backlog
Delays to accessing children and young people’s community services can have a profoundly negative impact on an individual child or young person’s educational outcomes, social development and mental health and wellbeing.
NHS Confederation
April 2022
Key messages
- The COVID-19 pandemic has had a unique and significant impact on children and young people, particularly on social development, education and mental health.
However, this impact has not been felt equally across society with some groups (particularly those from more disadvantaged backgrounds and those with disabilities) disproportionately affected. - Access to community health services for children and young people has been significantly affected by the pandemic.
At points during the pandemic effort, community services staff were redeployed from some children and young people’s services to prioritise an urgent and timely response to the pandemic.
While this may have been the right clinical prioritisation during a national crisis, its impact may be long lasting for some children and young people. - NHS England and NHS Improvement (NHSEI) data from January 2022 estimates that over 900,000 children and adults are waiting for services as part of a community services care backlog.
For community children and young people’s services, the most significant waits are in speech and language therapy, community paediatrics, occupational therapy, physiotherapy and neuro-developmental assessments for those with suspected autism and attention deficit hyperactive disorder.
For community children and young people’s services, the most significant waits are in speech and language therapy, community paediatrics, occupational therapy, physiotherapy and neuro-developmental assessments for those with suspected autism and attention deficit hyperactive disorder.
- While not part of official backlog figures, a reduced service offer during the pandemic has had an impact on children and young people and their families.
For instance, face-to-face health visiting can support early interventions and build important relationships with families.
Some of these key windows of opportunity have been missed. - Community providers have been using data, digital tools and a health inequalities lens to tackle care backlogs in the sector, including for children and young people’s services.
However, providers need more support to scale up this work.
Community providers have been using data, digital tools and a health inequalities lens to tackle care backlogs in the sector, including for children and young people’s services.
However, providers need more support to scale up this work.
- Workforce pressures, including shortages of staff in some key services, make it difficult for community providers to increase delivery to address backlogs of care.
- Complex commissioning and contracting arrangements, which are often based on historic agreements, also make it challenging to address the backlog of care in these services.
- Backlogs of care and reduced offers in community children and young people’s services have negative and far-reaching impacts for individuals and families and in socio-economic terms.
Delays to accessing these essential services can impact on social development and educational outcomes for individuals, and on wider society and the economy. - Colleagues in NHSEI and community providers are committed to radically improving the national dataset for community services to ensure prioritisation in national strategies and policy, but data to make the case for a greater focus on community provision remains inconsistent.
Also, data submitted to the community services data set does not appear in national waiting list figures, which reduces the visibility of community backlogs and acts as a barrier to accessing dedicated, central funding.
… data to make the case for a greater focus on community provision remains inconsistent. … Also, data submitted to the community services data set does not appear in national waiting list figures,

This Community Network briefing brings together new evidence about backlogs and increasing demand for children and young people’s services. It also demonstrates what community providers are currently doing to meet demand, including how they are innovating, and makes a series of recommendations on the national support needed, both now and in the longer term. The Community Network is hosted by the NHS Confederation and NHS Providers.
What do community providers need to address the backlogs of care in children and young people’s community services?
1. Short term
- Greater political focus, public profile and transparency around backlogs of care in the community sector and their impact, including for children and young people.
- Access to additional national funding and support (like the Elective Recovery Fund) to enable community providers to scale up and expand innovative work that is already taking place to address the backlogs of care across community services, and in particular children and young people’s services.
- Explicit national endorsement for community providers to use a health improvement approach to address backlogs of care in the sector, as is the case for the acute sector. This would allow them to focus on narrowing health inequalities rather than only driving down numbers. This would need to be accompanied by central support and guidance to develop data analysis, pathway design and approaches to clinical prioritisation.
- Continue work with community providers and NHS England and NHS Improvement to develop national, transparent data on community services and the backlogs in the sector.
- Engagement with national policymakers to explore the tools available to address backlogs in the community sector, like patient-initiated follow ups (as outlined in the elective recovery plan).
2. Longer term
- Better prioritisation of children and young people’s needs and services by integrated care systems (ICSs) and place-based partnerships, as required in the integrated care board model constitution.
- Reprioritisation of the role that community services play in joining up the delivery of care for children and young people.
- Explore potential new data collections to better understand the impacts of delayed care on outcomes, which is an important component in addressing health equalities, and the introduction of access standards for community health services.
- Workforce planning and funding to target the development of community roles where there are significant workforce pressures, including through alternative training, education and access routes.
- A review of existing contracting and commissioning of children and young people’s services to identify how ICSs (and place-based partnerships) can improve the commissioning of end-to-end services and reduce unwarranted variation in access.

BACKGROUND
What are community children and young people’s services?
Supporting children and young people to live well in the community is crucial to ensuring the health of future generations and supporting individuals’ life chances. Community providers, alongside wider system partners, play a key role in delivering this support.
Community health services — for both adults and children — form a core part of the health and care system, delivering 100 million patient contacts a year and employing one fifth of the NHS workforce. They also play a key role in delivering the future strategic ambitions of the health and care system by keeping people well at home, or in community settings as close to home as possible.
Community teams deliver a wide range of essential services for children and young people; from community paediatric services to specialist diagnostics, such as for autism spectrum disorders (ASD), health visiting services and children’s community nursing services (including complex care at home for children with long-term conditions or neurodisabilities).
Meeting the physical and mental health needs of children and young people in a holistic way is critical.
In 2020/21, around 40 per cent of children and young people with a diagnosable mental health condition were treated through NHS-commissioned community services. Community providers — alongside mental health trusts, acute trusts, voluntary, community and social enterprise providers and beyond — play a key role in delivering these mental health services.
Responding to the mental health needs of children and young people requires a whole-system approach across healthcare, education and wider settings. In terms of the NHS service delivery landscape, there are standalone mental health trusts, combined mental health and community trusts, and standalone community providers (including community interest companies) all delivering different (and sometimes overlapping) physical and mental health services for children and young people.
Responding to the mental health needs of children and young people requires a whole-system approach across healthcare, education and wider settings
Trusts that only provide community services and community interest companies tend to lead on delivering preventative and early intervention mental health services. They also deliver some elements of specialist care, such as services for people with autism. Trusts that also, or solely, provide mental health services often lead on delivering other parts of specialist care (for instance community mental health services for people with severe mental illnesses, eating disorder services) and specialist inpatient provision.
As in other service areas, community teams delivering mental health services to children and young people can act as a glue with wider voluntary and social care support. They play an important role in admission avoidance, and where individuals are admitted, provide essential ‘step-down’ support when they return to the community.
The impact of the COVID-19 pandemic on children and young people
The COVID-19 pandemic has caused huge disruption across society including well documented, significant impacts on children and young people, who have faced interruption to in-person education and a lack of social contact with peers at crucial points in their development.
This has led to growing concerns about the impact the pandemic, and associated lockdowns, have had on this group.
However, the pandemic has not affected all children and young people equally.
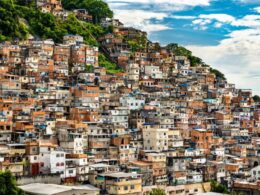
In the decade preceding the pandemic, child poverty and deprivation were rising (with rapid increases in the North of England).
Although there are no official figures to date, the expectation is that the pandemic has exacerbated this trend, with analysis by the Institute for Public Policy Research estimating that 200,000 more children were living under the pre-COVID-19 poverty line by the end of 2020. This is important because poverty is a key driver of health inequalities. COVID-19 admission rates were 2.9 times higher in the most deprived areas compared to the least deprived, while mortality rates were 2.4 times higher.
Poverty and health inequalities intersect with ethnicity. The rate of poverty is significantly higher for black and minority ethnic families than their white counterparts; 46 per cent of people living in families where the head of household is black, African, Caribbean or black British are in poverty, compared to just 19 per cent of those living in families where the head of household is white. People in black and minority ethnic families are also between two and three times more likely to be in persistent poverty than people in white families.
Moreover, black, Asian and minority ethnic groups made up a third of the critical care admissions for COVID-19, even though they make up less than 14 per cent of the UK population. Inevitably, a higher rate of serious illness among black, Asian and minority ethnic adults, and those facing deprivation and poverty, will have an impact on children and young people from these groups, who are more likely to encounter the disruption and distress related to this than their wider peers.
Furthermore, reduced social contact during the pandemic has increased risks of harm for vulnerable children and young people — community providers are concerned by a drop in safeguarding referrals during the pandemic, which may indicate hidden needs. Throughout the pandemic, providers from all sectors have reported an increase in children and young people presenting to health services when they actually require safeguarding support. Data reported by local councils in England (August 2021) shows that serious child harm cases rose by nearly 20 per cent during the first year of the pandemic.
Early evidence also suggests that COVID-19-related disruptions may have exacerbated triggers for poor mental health.
More children are now experiencing mental health problems than before the pandemic; in 2021 one in six children had a reported mental health problem, up from one in nine in 2017. In an NHS Providers survey of trust leaders in May 2021, 78 per cent of trust leaders said they were concerned about their trust/local system(s) ability to meet the level of anticipated demand within the next 12–18 months for mental health care among children and young people.
Furthermore, vulnerable children and young people, and those from black, Asian and minority ethnic backgrounds, are more likely to have faced some of the risk factors for poor mental health (such as family illness and financial insecurity).
Early evidence also suggests that COVID-19-related disruptions may have exacerbated triggers for poor mental health.
At the same time, the COVID-19 pandemic has had a significant impact on access to support in the community.
In response to the first wave of the COVID-19 pandemic, guidance was issued by NHS England and NHS Improvement (NHSEI) instructing community providers to reprioritise services and redeploy community staff (including for children and young people’s services) to support hospital discharge efforts in preparation for an expected wave of COVID-19 infections. As an example, evidence from the Royal College of Paediatrics and Child Health shows that reported redeployments of community child health trainees was as high as 46 per cent in April 2020.
Although a framework was published in June 2020 to restore children and young people’s community services, at different stages of the pandemic community staff have been redeployed to support COVID-19 vaccination efforts.
While mental health providers continued to run services with as much capacity as possible during the pandemic, service delivery and continuity of care were inevitably impacted. For example, important work to roll out mental health support teams in schools and colleges to improve children and young people’s early access to mental health support was also disrupted. Likewise, access to emotional health and wellbeing services in schools, which can provide early intervention support and reduce the need for mental health services, was reduced during the pandemic.
While prioritising discharges and the COVID-19 vaccine programme have been important decisions, redeploying community staff to support these efforts has contributed to increasing backlogs of care in the sector.
Community provider leaders tell us that there were significant waiting lists for community children and young people’s services before the pandemic, but this has now been exacerbated by COVID-19-related measures, and growing demand for services as lockdowns have lifted.
In addition, there are concerns about the impact of reduced service provision in some areas, and how this will impact on future demand and outcomes.
In many instances, health visitors paused face-to-face visits during the peaks of the pandemic, meaning some crucial opportunities for early intervention and relationship building with families may have been missed. Although this does not appear in official figures, this type of reduced service provision is likely to impact on individual children and young people as well as the wider health and care system.
The pandemic has also made it more difficult to address these backlogs, with increased workforce pressures (relating to vacancies, sickness and redeployments), and enhanced infection prevention control requirements reducing the capacity of community teams to increase service delivery.
In areas of significant concern like speech and language therapy for children and young people, NHSEI data from January 2022 shows that 47 per cent of restored or partially restored services have reduced activity levels compared to pre-COVID-19. This is broadly in line with figures from August 2021, demonstrating ongoing challenges with increasing activity levels to meet demand.
Which children and young people’s community services have the longest waiting lists?
National data on backlogs in the community sector is limited, but NHSEI’s Situation Report (SitRep) data from January 2022 shows that the backlog of care in both adult and children and young people’s community services stood at over 900,000 at the beginning of the year.
This data shows that the largest volume of long waits for children and young people’s community health services are for speech and language therapy, audiology, community paediatrics, occupational therapy and physiotherapy. Community providers also report that there are significant pressures on health visiting services and community dentistry services for both children and young people and adults.
The latest NHSEI data from January 2022 suggests that there were waiting lists of:
- over 66,000 for community paediatrics services
- 65,600 for speech and language therapy for children and young people
- over 22,000 for audiology for children and young people
- almost 20,000 for occupational therapy and over 18,000 for physiotherapy.
At the January 2022 SitRep, 39 per cent of community providers reported that waiting lists for children and young people’s services have increased since October 2019. The greatest increases have been in speech and language therapy, where 73 per cent of community providers report an increase in waiting lists since October 2019, and within that, 39 per cent report that their waiting list has grown by 51 per cent or more. Likewise, for audiology services, 61 per cent are reporting an increase in waiting lists, and within that a quarter said this has increased by 51 per cent or more.
Even compared to NHSEI SitRep data from August 2021, there has been a significant increase in the number of children waiting in these key service areas; for instance, the reported wait for community paediatrics has increased from 40,100 (August 2021) to over 66,000 (January 2022). Omicron pressures and guidance to redeploy community staff during December and January 2021/22 are likely to have contributed to growing waiting lists. Even before the pandemic, the community services with long waits were those struggling with significant workforce shortages, and this has only been exacerbated by the pandemic.
As of December 2021 [ 1 ] the number of children and young people with open referrals for mental health care was 397,147. It is important to note that this figure only represents the number of children and young people that have been referred. As the latest prevalence data shows, one in six children and young people now have a diagnosable mental illness. There are many more who are missing from these waiting lists and would benefit from care and support.
The data is important in helping to develop a picture of where there are the longest waits and pressures in service delivery. But underlying this, there is unmet demand for children and young people’s services, which has long-term impacts for individuals and for other parts of the health and care system.
The impact of backlogs of care in children and young people’s community services
While it is important to address backlogs of care across all services in the NHS, the potential impact of long waits for children and young people are both significant and often less visible to the wider public.
Although NHS leaders tell us that delayed interventions for children and young people in the community can have lifelong consequences, it can be difficult to demonstrate these long-term consequences and the impact of unmet needs in a timely manner and particularly within the context of a national public health crisis where limited resources were prioritised.
While it is important to address backlogs of care across all services in the NHS, the potential impact of long waits for children and young people are both significant and often less visible to the wider public.
Delays to accessing children and young people’s community services can have a profoundly negative impact on an individual child or young person’s educational outcomes, social development and mental health and wellbeing.
To take one example, long waits for speech and language therapy creates barriers to communicating with peers in social settings and at school, which has a knock-on effect on learning and socialising, as well as a child or young person’s ability to fulfil their potential as an adult. Similarly, delays to ASD assessments and diagnoses can have an enduring impact on a child or young person’s life. Without a diagnosis and appropriate treatment, children and young people with ASD can be treated as having behavioural issues, causing undue distress to individuals and their families.
Delays to accessing children and young people’s community services can have a profoundly negative impact on an individual child or young person’s educational outcomes, social development and mental health and wellbeing.
Long waits for children and young people’s community services adds to pressure felt in other parts of the health and care system.
For example, long waits in areas like dentistry can cause children and young people (as well as adults) significant pain and discomfort, often impacting sleep and subsequently educational attainment.
It also prompts some to present at A&E. Delays in accessing treatment can also contribute to more complex needs, with community providers reporting an increased number of follow-up appointments required.
Community providers also say there is an increased need to deliver face-to-face appointments for children and young people who have faced long waits and are now presenting with more acute needs.
Furthermore, long waits for children and young people seeking support in the community can have an impact on the mental health and wellbeing of the parents and carers looking after them, potentially putting pressure on other adult services.
In the longer term, delays to the diagnosis and treatment of health problems for children and young people can create further pressures on the system and costs to the public purse.
For example, there is a link between ASD and other mental health conditions (70 per cent of people on the autism spectrum also have a co-concurring mental health condition).
The National Autistic Society has previously estimated that investing in ASD diagnosis would lead to cost savings for the NHS of up to £337 million over five years (2018), from reduced spending on mental health services.
Delays in accessing community services for children and young people with ASD and learning disabilities is therefore likely to add pressure to mental health services, including through increased admissions to acute treatment unit admissions.
While admissions are important for some, for other children and young people, being removed from the home environment can have a negative impact on experience and outcomes.
The National Autistic Society has previously estimated that investing in ASD diagnosis would lead to cost savings for the NHS of up to £337 million over five years (2018), from reduced spending on mental health services.
Long waits for assessment, diagnosis and treatment have the potential to exacerbate health inequalities.
Timely access to support for children and young people with additional needs — including specialist nursing support in schools — provides an opportunity to intervene early in the drivers of health inequalities, while long waits risk widening disparities in both the social determinants of health and health outcomes.
Many parents who can afford private treatment for services such as physiotherapy or speech and language therapy will understandably access this, while those who cannot continue to wait.
Community providers tell us that delayed interventions for children and young people can be particularly damaging to outcomes, meaning that a two-tier system of quick private interventions and long NHS waits will only serve to entrench existing inequalities.
Without timely diagnosis and intervention, children and young people are less likely to fulfil their full economic and social potential, which has an impact on the wider economy and other public services.
The impact of care backlogs for these crucial children and young people’s services is not confined to the health and care system.
Without timely diagnosis and intervention, children and young people are less likely to fulfil their full economic and social potential, which has an impact on the wider economy and other public services.
Challenges in addressing backlogs of care in community children and young people’s services
The NHS is striving to tackle care backlogs and deliver care to the record 6.1 million people waiting for hospital treatment.
These efforts are being supported by political prioritisation and national funding.
The Elective Recovery Plan was announced in February 2022 to tackle the waiting lists for elective care, and includes ambitions to deliver 30 per cent more elective activity by 2024/25 than before the pandemic and eliminate waits of longer than 12 months by 2025.
The plan builds on previous funding announcements to support elective recovery — including £8 billion revenue funding between 2022/23 and 2024/25 and £5.9 billion in capital funding announced in the October 2021 Spending Review.
To date, no equivalent focus or funding has been assigned to backlogs of care in the community sector.
While there is significant work underway within NHSEI to improve data collection and quality, it is currently more difficult to make the case for equivalent focus and funding in the community sector due to ongoing challenges with national data on the sector.
For example, waiting times for treatment and pressures on demand are not routinely captured in national — and publicly available — data, so it is difficult to demonstrate the scale of the backlogs of care. Also, in the acute sector, there are clear and more immediate links between delayed elective care and emergency admissions; in the community sector it is more challenging to demonstrate the long-term impact of delays to children and young people accessing the services they need, and deserve.
Furthermore, while improved data collection through the community services data set is much needed and welcome, community pathways are generally not covered by the national referral to treatment (RTT) standards, and are therefore not included in national waiting list numbers.
Without this parity, backlogs in community health services will not receive the same national recognition and visibility as other sectors.
Reflecting challenges across the health and care system, workforce pressures also create a barrier to increasing capacity and tackling the backlogs of care in community children and young people’s services.
In the community sector these pressures have been exacerbated by workforce redeployments during the pandemic, as well as long-standing shortages in district nurses and allied health professionals.
Community children and young people’s services with the largest volume of long waiting lists (for instance, speech and language therapy, occupational therapy, physiotherapy, audiology and other services) tend to be those with the most intense workforce pressures, and some community providers suggest that it would be difficult to address these backlogs within existing workforce capacity.
These challenges are compounded by complicated contracting and commissioning arrangements for children and young people’s services delivered in the community.
For instance, some children and young people’s therapies are commissioned by clinical commissioning groups, others by local authorities, and some specialist services by NHSEI, while delivery is spread across community primary care and wider providers, depending on the level of support required. This can lead to a fragmented and confusing landscape of commissioning responsibilities, and a lack of effective strategic planning, which can lead to worrying gaps in provision.
One community provider reports that there is a local mental health service delivered by a community provider for 11–14 year olds and 16–18 year olds, but there is no such service provided for those aged 15.
This is not an isolated incident, but a widespread and systemic issue in the commissioning and delivery of these services. Some community providers tell us that they are commissioned to deliver ASD assessments, but with no provider in the same area commissioned to deliver care and support for those who receive a diagnosis. Others note that the level of investment for community ASD services is rooted in historic commissioning behaviours rather than patterns of demand creating unwarranted variation in access to services.
How have community providers responded so far?
Despite the difficulties, community providers are rising to the challenge and working incredibly hard to address backlogs of care in community services. NHSEI SitRep data from January 2022 shows that 73 per cent of services are now fully restored.
Community providers have been using a range of tools to support them to restore services and manage waiting lists.
Firstly, many community providers have been undertaking significant work at a local level to understand what community backlogs look like, and to inform their strategy for addressing these.
As part of this, some providers have been cleaning organisation-level data to develop an accurate picture of the people waiting for community services, and those that are missing from these lists but may require support.
In some place-based partnerships, community providers are taking a targeted approach to ensure that key areas like children and young people’s services are prioritised in this work.
This helps to both understand the task at hand, and where there may be blind spots in provision for key service lines that can contribute to wider health inequalities.
Alongside understanding local population needs, community providers are taking action to ensure that backlogs are managed in a way that reduces health inequalities.
Community providers agree that it important to reduce waits for all services, but suggest that a differential approach to waiting lists, which stratifies caseloads by clinical risk, can help to prevent exacerbating existing health inequalities.
When stratifying by clinical risk, a health improvement approach will take into account wider factors, like ethnicity and deprivation, to recognise that clinical risk is not about only about the level of acuity that an individual is currently presenting, but also the broader range of risk factors that might mean that, all things being equal, two people receiving the same treatment might have different outcomes.
Colleagues in the acute sector have received national endorsement for this approach, and community providers also need this support alongside recognition of the role that they can play in reducing health inequalities.
Community providers are also using new virtual tools and technologies to see as many patients as possible in a timely way.
For instance, using digital technologies, such as virtual consultations for children’s speech and language therapy. [ 2 ]
Others also note that they are working collaboratively with schools and local authorities to support the delivery of non-clinical support, and exploring how virtual tools like apps can be used to manage backlogs.
About the Community Network
The Community Network is the national voice of NHS community providers, hosted by the NHS Confederation and NHS Providers. We support trusts and not-for-profit organisations providing NHS community health services to deliver high-quality care by influencing national policy development, sharing good practice, and promoting a vision of integrated care in the community
Footnotes
See original publication