the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
October 31, 2023
What is the message?
The article discusses the pressing issue of clinical workforce shortages in healthcare and the need for transformative actions to address it.
It emphasizes the role of boards in overseeing these changes and suggests a five-fold approach (De-Risk, Reduce, Retain, Recruit, and Reimagine) to build clinical capacity for today and the future.
The healthcare systems should use a human + machine approach, incorporating automation and technology to free up clinicians from non-essential tasks, allowing them to focus on meaningful patient care.

What are the key points?
Snowballing Clinical Workforce Shortages:
- The clinical workforce shortage in healthcare is a significant problem, worsened by the pandemic.
- High turnover rates among hospital staff, particularly registered nurses, have increased attrition and vacancies.
- A substantial portion of the nursing workforce is expected to retire in the next decade.
Recruiting Alone is Not the Solution:
- Addressing workforce shortages through recruiting alone is challenging and expensive, with rising contract labor costs.
- Clinicians are burdened with tasks that don’t require their expertise, contributing to burnout and attrition.
The Power of a Human + Machine Approach:
- Combining human ingenuity with technology, such as automation and artificial intelligence, can transform the clinical workforce.
- Automation isn’t about replacing people but freeing them from routine tasks, allowing clinicians to focus on critical decisions and patient care.
- Real-world examples, like Cedars-Sinai Medical Center, show how automation can improve the focus of clinical teams.
Define Your Future-Forward Clinical Workforce Strategy:
- Health systems can use automation to address short-term workforce shortages while preparing for long-term changes.
- Five fundamental strategies are proposed: (De)-Risk, Reduce, Retain, Recruit, and Reimagine.
- Strategies include data-driven attrition analysis, reducing low-impact tasks, retaining talent through skills development and support, recruiting tailored to candidate needs, and laying the foundation for technology-driven change.
The Top Takeaways for Boards:
- Boards play a crucial role in overseeing and driving organizational readiness for change.
- Boards should focus on supporting agility, measuring and promoting psychological safety, investing in technology, modernizing workforce IT solutions, and fostering partnerships for clinical training pipelines.
The Human Element:
- While technology and automation are critical in addressing workforce shortages, the human element remains central.
- Automation empowers clinicians to refocus on their core responsibilities and rediscover the human aspects of their careers.
- The intersection of technology and humanity is key to successfully addressing the clinical workforce shortage.
DEEP DIVE
Refocusing Clinical Workforce on Moments that Matter
AHA Trustee Services
By Kristin Ficery
De-Risk, Reduce, Retain, Recruit and Reimagine
The clinical workforce shortage is one of the most pressing problems in health care. Bold actions now are necessary to mitigate the challenge, and boards have a critical role to play in overseeing change. By giving clinicians the support they need to work with purpose and passion, health systems can build clinical capacity for today — and tomorrow.
Snowballing clinical workforce shortages
A combination of workloads, stress and burnout drove a wave of attrition across the clinical workforce during the pandemic. But the crisis only exacerbated an already systemic issue. According to NSI Nursing Solution, Inc., the hospital turnover rate increased from 19% in 2018 to 26% today, and the turnover rate for registered nurses jumped from 17% in 2018 to 27% during the same period. And the problem is expected to continue. Consultant 360 reports that one-third of the nursing workforce is set to retire over the next 10 to 15 years.
Recruiting alone is not the solution
Closing the gaps created by high attrition and vacancies across the clinical workforce is increasingly challenging. With contract labor costs skyrocketing, there is not a cost-effective “safety-valve” for health systems to fill open roles quickly. In fact, contract nurses’ median hourly rates grew by an astounding 106% between 2019 and 2022, according to Kaufman Hall.
All this has a negative effect on clinical personnel who remain. Today’s clinicians are burdened with too many “moments that don’t matter,” triaging skills gaps and performing simple but time-consuming tasks like medication verification, clinical documentation and service and supply coordination. It is a troubling reality that sets up an endless cycle of burnout and attrition, poised to make a bad situation even worse.
To stop this cycle and address the clinical workforce crisis, health systems should go beyond recruiting or teaching new skills to clinicians who stay. It is time to fundamentally change health care delivery, transforming both the work and the workforce experience for clinical care teams. It is not just the Chief Human Resources Officer who must lead the transformation. This issue touches the entire executive team and board members. All leaders must champion new ways of working and organizational agility.
The power of a human + machine approach
Automating aspects of clinical care delivery will affect health care workers of all skill levels. Accenture expects that automation will affect 93% of health care provider roles.
Automating aspects of clinical care delivery will affect health care workers of all skill levels. Accenture expects that automation will affect 93% of health care provider roles.
By combining human ingenuity and technology, health systems can transform the clinical workforce—both what they do and how they do it. This human + machine approach uses automation, artificial intelligence (AI) as well as alternative sourcing and human-centered support for clinicians.
It’s important to understand that automation in the clinical setting isn’t about substituting for people. It’s about augmenting people by substituting for tasks. This way, clinical teams have more time and head space to make critical decisions and deliver high-quality care.
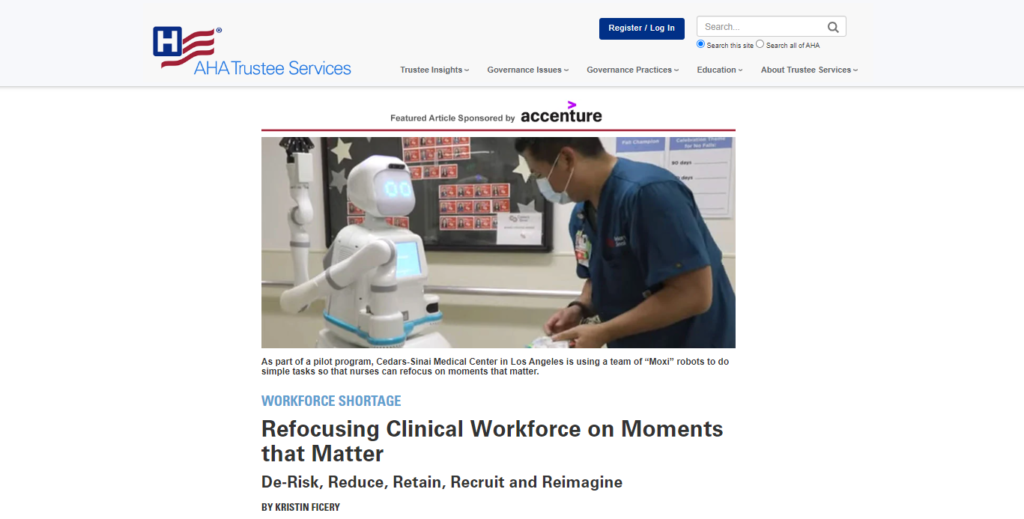
We’re already seeing this happen in health systems across the country. Take Cedars-Sinai Medical Center in Los Angeles, for example. As part of a pilot program, the health system is using a team of “Moxi” robots to do simple tasks so that nurses can refocus on moments that matter. Cedars-Sinai reports that clinical teams walked 300 miles less in the first six weeks when the machines were on the floor.
There is exciting potential to use automation and other digital technologies to refocus clinicians on the work they were trained to do, and that requires uniquely human skills and empathy. However, we aren’t going to wake up tomorrow to robots at the bedside. Expect this transformation to occur over the next five years. Also, expect the first frontier of automation in health care to occur across non-clinical roles where the human-to-human interactions are not as nuanced.
Define your future-forward clinical workforce strategy
While health systems won’t realize the full value of automation in clinical care for several years, they should consider it as they develop strategies to address the workforce shortage in the short term. The place to begin is by defining the strategy against five fundamentals.
1. (De)-Risk: What’s causing your people to leave? Who is most at risk?
Health systems can’t address the clinical workforce shortage in a precise and timely way without understanding the extent of the problem in their own institutions. So, leaders need a data-driven view of attrition at the department or even the role level.
One way to get this view is with dashboards that track increases in leaves of absence, trends in absenteeism and metrics associated with burnout. These tools are powered by retention analytics that identify key attributes that drive attrition, predict employees with high flight risk, and help health systems take preventive actions to retain these employees and reduce attrition costs.
2. Reduce: How can you help your people focus on the work they love?
The more that health systems keep clinicians operating at the top of their licenses, the more satisfied and engaged they will be—and the better patient care will be. This means reducing low-impact, high-occurrence clerical tasks, such as documenting visits or scheduling follow-ups, through automation and better-implemented technology. Shifting non-bedside tasks to these lower-cost solutions removes frustration and friction while allowing clinicians to focus on what they do best.
Consider what a large, faith-based health system did to reduce burden on nurses. It used a remote nurse expert to participate in huddles, integrate into floor activities and recognize opportunities to support the unit. The initiative also included a unit secretary concierge to catch patient alerts, track orders and provide as-needed assistance across the unit.
3. Retain: How do you keep the people you have today?
Health systems have tried to keep clinicians on staff by increasing their salaries and benefits. Yet the reality is that this approach becomes cost prohibitive very quickly. Plus, keeping skilled clinicians is also about meeting human needs that go well beyond a generous salary and benefits package.
Career progression is one of these human needs. It’s critical for health systems to establish unique and personalized skills development programs to help people develop their career paths. One post-acute care organization used a leadership development strategy that included out-of-the-box rewards tailored to the workforce, which lowered attrition rates. People also want to be valued at work. Health systems that focus on building trusting relationships, supporting personal well-being and championing equality can go a long way in keeping clinicians satisfied with the jobs they have.
4. Recruit: How can recruiting programs stay relevant in a changing landscape?
In a job seeker’s market like this one, it’s imperative that health systems shape recruitment approaches around candidates’ needs and expectations. People want clear communication, faster hiring and onboarding and flexible shift options. As they develop recruiting programs, health systems should use employer branding tactics to position the health system as an employer of choice.
Rethinking recruiting for today also means tapping into non-traditional talent pools and exploring new ways of sourcing work. For example, to reduce local nursing requirements and the recruitment and hiring burden, some health systems have turned to outsourcing specific nursing services.
5. Reimagine: How do you begin to create the future workforce?
Although the automation era in clinical care is in its early, task-level days, leaders should lay the foundation for change now. Bringing broader, platform-level automation into clinical care is not a matter of introducing more technology and watching outcomes happen. Health systems need to make deliberate, business-driven decisions around the right processes to automate for the greatest benefit at the lowest risk. Further, technology leaders need to be familiar with innovation in AI, robotics, machine learning and the metaverse—understanding integration issues and possibilities that synergies between capabilities can bring. Case in point: a major health care system running a cancer review board program created a virtual workspace for clinicians from different specialties to meet and review cases collectively.
Technology-supported strategies provide a foundation for new ways of working. With the right foresight, technology transformations can support task-shifting, process optimization and delivery model redesign that offer competitive experience and more agility at lower cost. The right combination of technologies, enlightened management and operating model redesign can mean a more empowered, psychologically-safe workforce that delivers exceptional care. This is key to a positive employee experience, which matters for clinical care teams, patients and health systems. Research shows that negative employee experience can have a significant impact on patient satisfaction, patient safety and profitability.
The top takeaways for boards
The reality is that change in health care will only accelerate, and the clinical workforce will continue to be on the frontlines of it. As health systems act on these five fundamentals, boards should be engaged in helping the CEO and executive team cultivate organizational readiness with intention—and flexibility.
This is critical because health systems require innate operational resiliency and agility as constraints drive new models of delivery. And it’s why boards, executives and managers—all leaders—should become skilled in modern management approaches. Boards in particular should prioritize the following strategies:
- Oversee transformation of operating models so that agility becomes part of the organizational DNA.
- Encourage management to codify measurement and support for the psychological safety and well-being of people at all levels.
- Monitor plans for major automation platform investments beyond electronic medical records.
- Get more engaged in efforts to modernize workforce IT solutions, ensuring that plans meet mission and cost imperatives.
- Be decisive about supporting new investments in clinical training pipeline partnerships to grow teams’ skills and support their upward career paths.
The human element is always the touchstone
Human + machine will revolutionize health care delivery and help the workforce refocus on the moments that matter. But the human element will always be the touchstone. Automation makes it possible for clinicians to not only focus on the work they were trained to do, but also to rediscover the human foundations of their chosen careers. As health systems balance short- and long-term solutions to the clinical workforce shortage, the most successful will meet at the intersection of technology and humanity.
Originally published at https://trustees.aha.org











