The Lancet
December, 2021
Liver Disease in Europe
Liver disease is a leading cause of years of working life lost in Europe, second only to ischaemic heart disease.
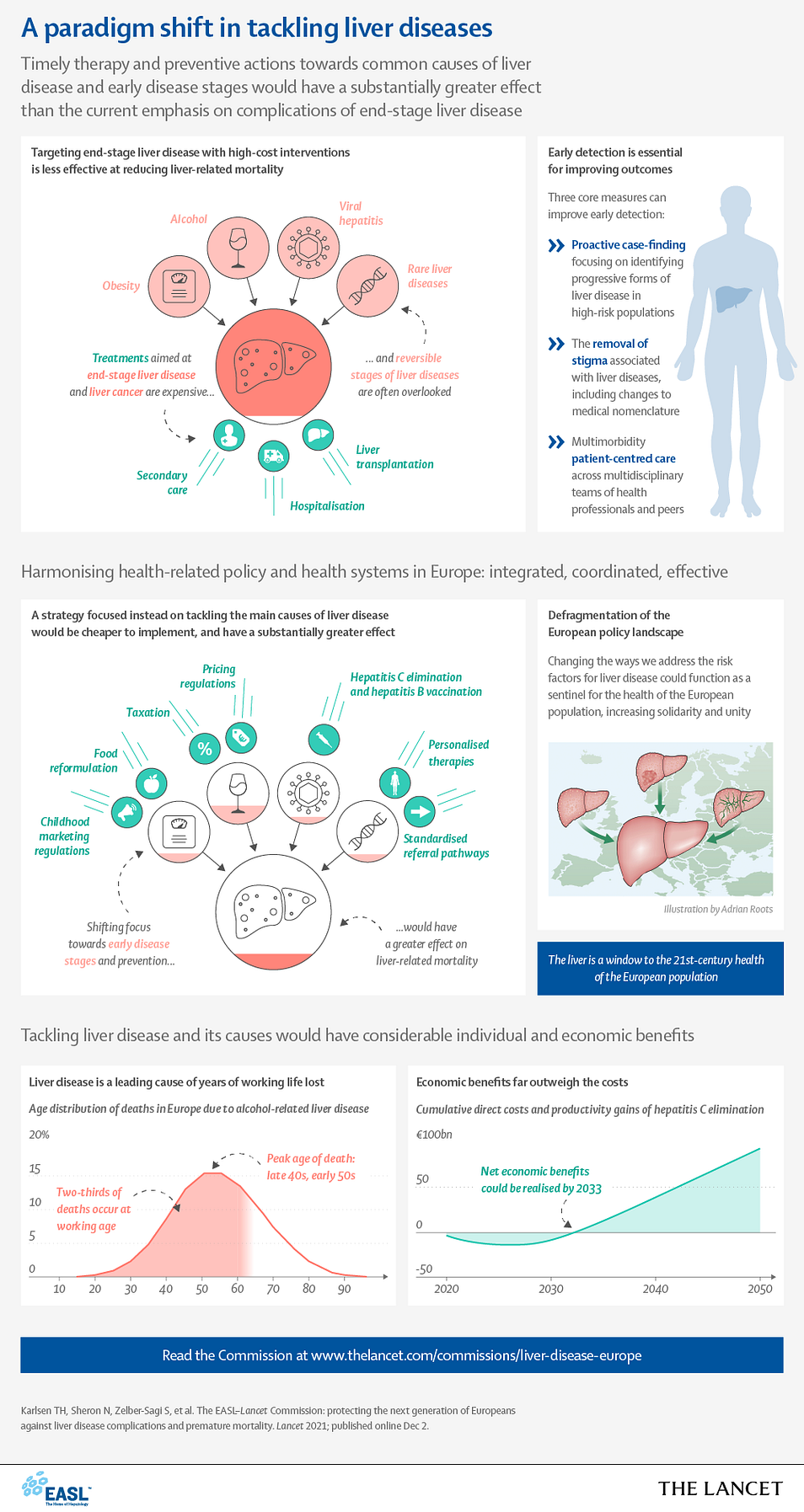
One of the continuing problems has been the focus on end-stage liver disease and its complications — cirrhosis and cancer.
A new report argues that there should be a fundamental change to prevent the development of advanced liver disease by embracing simple methods for early identification of progressive liver fibrosis together with strategies for disease prevention.
Explore the key messages below, and read the EASL-Lancet Commission: Protecting the next generation of Europeans against liver disease complications and premature mortality.

The EASL–Lancet Liver Commission: protecting the next generation of Europeans against liver disease complications and premature mortality
Prof Tom H Karlsen, MD *, Prof Nick Sheron, FRCP †, Shira Zelber-Sagi, PhD, Patrizia Carrieri, PhD, Prof Geoffrey Dusheiko, MD, Prof Elisabetta Bugianesi, MD †, et all
Published:December 02, 2021
Executive summary
Liver diseases have become a major health threat across Europe, and the face of European hepatology is changing due to
- the cure of viral hepatitis C and the control of chronic viral hepatitis B,
- the increasingly widespread unhealthy use of alcohol,
- the epidemic of obesity,
- and undiagnosed or untreated liver disease in migrant populations.
Consequently, Europe is facing a looming syndemic, in which socioeconomic and health inequities combine to adversely affect liver disease prevalence, outcomes, and opportunities to receive care.
In addition, the COVID-19 pandemic has magnified pre-existing challenges to uniform implementation of policies and equity of access to care in Europe, arising from national borders and the cultural and historical heterogeneity of European societies.
In following up on work from the Lancet Commission on liver disease in the UK and epidemiological studies led by the European Association for the Study of the Liver (EASL), our multidisciplinary Commission, comprising a wide range of public health, medical, and nursing specialty groups, along with patient representatives, set out to provide a snapshot of the European landscape on liver diseases and to propose a framework for the principal actions required to improve liver health in Europe.
We believe that a joint European process of thinking, and construction of uniform policies and action, implementation, and evaluation can serve as a powerful mechanism to improve liver care in Europe and set the way for similar changes globally.
On the basis of these data, we present ten actionable recommendations, half of which are oriented towards health-care providers and half of which focus primarily on health policy.
A fundamental shift must occur, in which health promotion, prevention, proactive case-finding, early identification of progressive liver fibrosis, and early treatment of liver diseases replace the current emphasis on the management of end-stage liver disease complications.
A considerable focus should be put on underserved and marginalised communities, including early diagnosis and management in children, and we provide proposals on how to better target disadvantaged communities through health promotion, prevention, and care using multilevel interventions acting on current barriers.
Underlying this transformative shift is the need to enhance awareness of the preventable and treatable nature of many liver diseases.
Therapeutic nihilism, which is prevalent in current clinical practice across a range of medical specialities as well as in many patients themselves, has to end.
We wish to challenge medical specialty protectionism and invite a broad range of stakeholders, including primary care physicians, nurses, patients, peers, and members of relevant communities, along with medical specialists trained in obesity, diabetes, liver disease, oncology, cardiovascular disease, public health, addictions, infectious diseases, and more, to engage in integrated person-centred liver patient care across classical medical specialty boundaries.
This shift includes a revision in how we converse about liver disease and speak with our patients, and a reappraisal of disease-related medical nomenclature conducted to increase awareness and reduce the social stigmatisation associated with liver disease.
Reimbursement mechanisms and insurance systems must be harmonised to account for patient-centric, multimorbidity models of care across a range of medical specialties, and the World Health Assembly resolution to improve the transparency and fairness of market prices for medicines throughout Europe should be reinforced.
Finally, we outline how Europe can move forward with implementation of effective policy action on taxation, food reformulation, and product labelling, advertising, and availability, similar to that implemented for tobacco, to reduce consumption of alcohol, ultra-processed foods, and foods with added sugar, especially among young people.
We should utilise the window of opportunity created by the COVID-19 pandemic to overcome fragmentation and the variability of health prevention policies and research across Europe.
We argue that the liver is a window to the 21st-century health of the European population.
Through our proposed syndemic approach to liver disease and social and health inequities in Europe, the liver will serve as a sentinel for improving the overall health of European populations.
Key messages
- Liver disease is now the second leading cause of years of working life lost in Europe, after only ischaemic heart disease
- The clinical focus in patients with liver disease is oriented towards cirrhosis and its complications, whereas early and reversible disease stages are frequently disregarded and overlooked
- The dissociation between primary and secondary care and the considerable heterogeneity across clinical pathways and inconsistent models of care cause delays in diagnosis of both rare and common liver diseases
- Stigma has a major impact on liver diseases in Europe, leading to discrimination, reduction in health-care seeking behaviour, and reduced allocation of resources, which all result in poor clinical outcomes
- Europe has the highest level of alcohol consumption in the world, which, together with ultra-processed food consumption and high prevalence of obesity, are the major drivers of liver-related morbidity and mortality
- A scarcity of consistent and efficient screening and vaccination programmes for viral hepatitis combined with the high costs of drugs due to variable European reimbursement systems result in reduced access to treatment and delays in elimination programmes
- COVID-19, alongside imposing delays in diagnostic pathways of liver diseases, has brought overlapping metabolic risk factors and social inequities into the spotlight as crucial barriers to liver health for the next generation of Europeans
- Liver diseases are generally avoidable or treatable if measures for prevention and early detection are properly implemented; achieving this would reduce premature morbidity and mortality, saving the lives of almost 300 000 people across Europe each year
Table 2 — Recommendations of the EASL–Lancet Commission on liver disease in Europe
1.We recommend a simplified outreach approach (figure 18) using standardised liver blood tests with laboratory reflex-testing to facilitate early case-finding among individuals at high risk of liver disease, along with a consistent emphasis on fibrosis testing using FIB4 to rule out patients with advanced fibrosis; social inequalities are intimately linked to susceptibility to liver disease, meaning dedicated strategies are needed to engage disadvantaged groups in care
2.We recommend investment to scale up case-finding and screening for viral hepatitis in selected (eg, primary care serving immigrants, harm reduction or drug services, and prisons) and broader community settings (eg, coupled with SARS-CoV-2-antibody testing), with reflex testing for viraemia for those with antibodies
3.We recommend that EASL and other medical specialist organisations collaborate to develop a European-wide syllabus for primary care hepatology with an emphasis on simplified patient-centred pathways and multimorbidity models of care, accounting for the collaboration between hepatologists and primary care clinicians, nurses, peer educators, and other medical specialties
4.We recommend that all non-viral liver diseases be classed as NCDs to allow the commonalities of NCDs to prompt a network of chronic care models, which include specialists, primary care physicians, and nurses, trained in obesity, diabetes, liver disease, cardiovascular disease, and chronic kidney disease, as well as peers and members of the community, to facilitate engagement in liver patient care across classical medical specialty boundaries
5.We recommend a range of initiatives to oppose all forms and sources of stigma and discrimination of people at risk of or with liver disease using multilevel interventions that also involve peers and members of the community
6.We recommend public disclosure of pricing information of approved antiviral drugs currently used to treat viral hepatitis in Europe, which would reinforce the WHO and World Health Assembly resolution to improve the transparency and fairness of market prices for medicines
7.We recommend that European governments introduce uniform and effective policies to reduce the harmful use of alcohol; specifically, we recommend that a minimum price of €1/cL of pure alcohol (MPC) is introduced across all countries of the EU and associated countries and that the MPC is accompanied by appropriate increases in alcohol taxation to ensure that any MPC windfall to retailers is returned to government finances
8.Recognising the deleterious impact of the marketing of alcohol and ultra-processed, high-sugar food and drinks to children, we call for attention to unregulated narrowcasting of marketing messages to mobile phones by digital and social media; experience from the tobacco industry has shown that the only effective means to protect children is through a complete ban on the marketing of alcohol and HFSS foods, and hence we call for such a complete ban in all social and digital media
9.We call for policy measures to promote industry-led food reformulation and the minimisation of social inequities by subsidising healthy foods
10.We call for a coordinated and systematic public health case to be made to rebut the nanny-state and pseudoprotective arguments, which favour exclusion of specific groups and obstruct population-level policies to reduce liver disease mortality; in particular, the EU and European governments should prioritise the harmonisation of all forms of public health interventions across Europe with a particular emphasis on vulnerable groups, such as children, people who inject drugs, immigrants, and the less affluent
Originally published at https://www.thelancet.com












