NEJM Catalyst Innovations in Care Delivery 2022
Lisa Patel, MD, MESc, Kathryn C. Conlon, MPH, PhD, Cecilia Sorensen, MD, Samia McEachin, Kari Nadeau, MD, PhD, Khyati Kakkad, MD, and Kenneth W. Kizer, MD, MPH
June 15, 2022
Site version edited by:
Joaquim Cardoso MSc
Health Transformation Institute (HTI)
Strategy Advisory Consulting
Climate Change Unit
July 13, 2022
Summary
- Earth’s warming climate is causing heat waves to become more frequent, longer lasting, and hotter, while occurring in locations unaccustomed to such weather events.
- Extreme heat events (EHEs), such as those in the western United States, India, Pakistan, Central Europe, and other locations in recent years, are one of the deadliest consequences of climate change.
- EHEs cause excess morbidity and mortality directly from heat illness, aggravation of comorbid conditions, and exacerbation of the damaging health effects of social factors as well as indirectly from corollary events such as wildfires and air pollution.
- Climate change–related EHEs are projected to worsen for at least the next 3 decades, necessitating that health systems be prepared to meet a growing burden of heat-related illnesses and become more heat resilient, as well as to reduce health care–related climate impacts.
In this article, the authors discuss the health effects of EHEs and provide illustrative examples of what health systems can do to promote climate readiness and heat resiliency.
Structure of the publication:
- Introduction
- The Health Hazards of a Warming Planet
- Heat-Resilient Health Systems
- Ahmedabad and New York City Heat Safety Plans
- Climate Risk and Community Vulnerability Assessments
- Essential Clinical Care and Services Delivery Planning
- Infrastructure Protection and Resilience Planning
- Align Health Care Operations Around Carbon-Neutrality Goals
- Looking Ahead
Looking Ahead
- As the climate crisis worsens, heat waves and EHEs will take an increasing toll on human health.
- Encouragingly, heat is increasingly being recognized as a killer that needs more attention and more coordinated responses.
These efforts are taking various forms.
- For example, Seville, Spain, announced in 2021 that it plans, this year, to begin naming and ranking heat waves (as with hurricanes) in an effort to better raise awareness about the dangers of extreme heat.59
- California is considering legislation to name heat waves on the basis of a ranking system that would mobilize resources to protect community health according to a heat wave’s ranking.60
As warning and activation systems improve and expand, health systems will have to consider their role and place in preparation for EHEs and treatment and prevention of their associated illnesses.
Mapping vulnerable populations, ensuring that these populations receive appropriate counseling and warning, and forming close partnerships and communication with organizations that can assist vulnerable populations during heat waves is perhaps one of the most essential undertakings of a health care system.
- As the recent Pacific Northwest experience with heat waves demonstrates, hospital preparedness for the influx of patients that result from an EHE is important, …
- … but health systems also have to invest in building community resilience to keep community members out of the hospital as much as possible.
Although this article focuses on heat waves, the climate crisis portends diverse and severe effects that will dictate that health systems create adaptable response plans tailored to local circumstances of geography, weather and climate, vulnerable populations, and compound events.
- The threats posed by climate change within each region will be unique, unpredictable, and varied, as demonstrated by the polar vortex that plunged Texas into freezing arctic temperatures or the combined heat and wildfire threats in California.
- Hazard vulnerability assessments that better integrate climate risks can help health systems make the difficult decisions on what investments are needed to improve climate change resiliency.
Finally, while a certain amount of harm has been locked in as a result of historical and ongoing carbon emissions, hospital systems have the opportunity now to prevent heat waves from growing substantially worse by being a part of climate solutions.
Protecting our patients and communities from the harms of heat waves will take a multifaceted approach that should include preparedness but also mitigation for the overarching cause: climate change.
Selected images

The United Nations Intergovernmental Panel on Climate Change (IPCC) reported in 2021 that human activity had increased Earth’s temperature by 1.1°C since 1900, and warned that it will unalterably reach 1.5°C above 1900 levels in less than 20 years, causing devastating impacts on human health. Without the rapid reduction of greenhouse gas emissions, global warming will rise more than 1.5°C and have catastrophic consequences for humanity.
The myriad manifestations of the evolving climate crisis are graphically demonstrated by the increased occurrence of extreme weather events such as heat waves, wildfires, floods, droughts, tornadoes, and tropical cyclones.,These events adversely impact health by directly causing injuries and illnesses and by disrupting the operation of health care facilities, among other ways; these health effects disproportionately impact vulnerable populations due to poverty, housing or food insecurity, age, racism, and other social factors that negatively affect health.
The Health Hazards of a Warming Planet
Among the growing array of extreme weather events caused by climate change, extreme heat events (EHEs) — extended periods of unusually hot temperatures — are of particular concern because of their protean deadly consequences. Heat waves generally and EHEs specifically have occurred more frequently and increasingly in locations unaccustomed to such events. EHEs cause excess morbidity and mortality directly from heat illness, aggravation of comorbid conditions, and exacerbation of untoward health effects of socioeconomic and cultural circumstances, as well as indirectly from often associated events such as wildfires, drought, and air pollution. More than one-third of heat-related deaths during the past 30 years (37%; range, 20.5%-76.3%) are directly attributed to climate change. The IPCC predicts that with 1.5°C of planetary warming, historically twice-per-century heat events could happen every 6 years, or nearly 10 times more often.
Illustrative of recent EHEs, the U.S. Pacific Northwest experienced a heat dome (when the atmosphere traps hot ocean air) in the summer of 2021, during which temperatures peaked at 46.7°C (116°F) — an unprecedented event in recorded history. This EHE was linked with a 69-fold increase in ED visits in Washington State for heat stroke, heat exhaustion, exacerbation of chronic medical conditions (e.g., cardiovascular conditions, respiratory disease, or diabetes), and one case of third-degree burns from walking on hot asphalt.,If the mean planetary temperature increases beyond 2°C, which is expected at the current pace of carbon emissions, then the Pacific Northwest can expect this type of 1-in-1,000-year event to occur every 5–10 years.
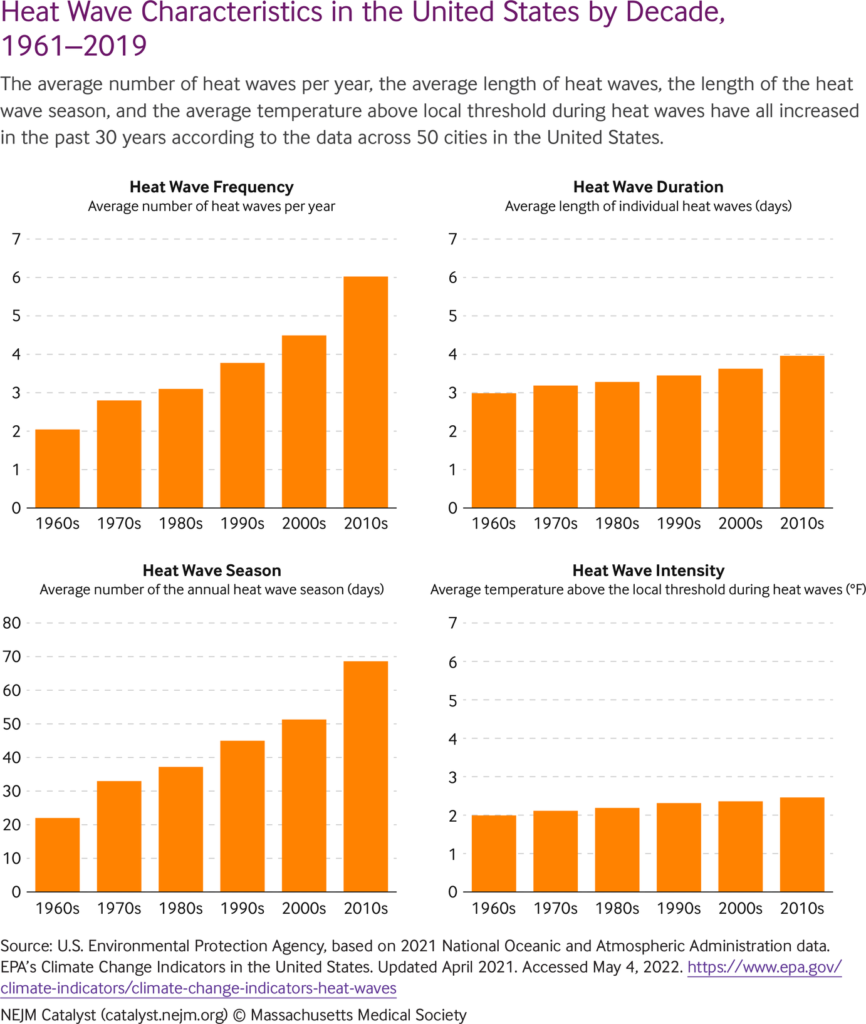
Heat events of increased frequency, intensity, and duration can be expected throughout the United States () and the world.
Globally, this has resulted in a 53.7% increase in heat-related mortality among individuals older than 65 years of age in the past 20 years, with those working in the agriculture industry being most at risk. Climate change-caused nighttime warming is particularly dangerous to health because it does not allow the body time to recover from a hot day.
If the mean planetary temperature increases beyond 2°C, which is expected at the current pace of carbon emissions, then the Pacific Northwest can expect this type of 1-in-1,000-year event to occur every 5–10 years.
On a global scale, compared with data from between 1983 and 2016, a warming planet has meant 3.1 billion more person-days of extreme heat in 2020 for people older than 65 years of age and 626 billion more person-days of exposure for children younger than 1 year of age. This is especially problematic for an increasingly urbanized world because of the urban heat island effect — the phenomenon where roads and buildings in urban areas absorb and re-emit heat, resulting in warmer temperatures than surrounding nonurban areas by upward of 10°C. The urban heat island effect has accelerated heat risks for individuals living in low-income urban neighborhoods, tripling the number of individuals worldwide exposed to extreme heat as a result of their living in denser populations with less access to mitigating factors such as urban vegetation.
Periods of extreme heat will also tax power grids, causing power blackouts and adversely impacting health and health systems in three main ways. First, power blackouts shut off mechanical air conditioning in homes, workplaces, and other settings, exposing many more people to heat. One study of three U.S. cities estimates that power outages during a heat wave would expose 68% to 100% of those urban populations to an elevated risk for heat exhaustion and heat stroke. Second, patients with various chronic medical conditions who are treated at home with the aid of electrically powered equipment (e.g., oxygen concentrators, ventilators, or motorized vehicles) may be harmed because their equipment becomes inoperable, and they will likely seek care at the nearest hospital. Experiential data from wildfires in the western United States in recent years and from the polar vortex in Texas in 2021 indicate that significant numbers of home-care patients will seek care at hospitals when the power goes out.
Third, hospitals also risk losing power in situations when the power grid is overtaxed, disrupting care and exposing highly vulnerable persons to elevated temperatures. Because hospitals are typically sealed buildings, loss of power can result in a rapid rise in interior temperatures during a heat wave. For example, the University of South Alabama Medical Center lost power during a 2010 heat wave, causing its cooling systems to fail and indoor temperatures to soar. Similarly, Plumas Hospital in Quincy, California, had to close after it lost power during a heat wave, forcing it to transfer its patients. Newer hospitals have increased their emergency power capabilities to include mechanical cooling, and hospitals certified by the U.S. Centers for Medicare & Medicaid Services (CMS) are required to have backup generators to maintain safe temperatures. However, many health care facilities (e.g., nursing homes) remain at risk of losing air-conditioning capability when power is disrupted.,
Heat-Resilient Health Systems
Health system preparedness for the growing threat of heat waves and EHEs should be rooted in the concept of resilience, which is defined by the IPCC as, “the capacity of social, economic, and environmental systems to cope with a hazardous event or trend or disturbance, responding or reorganizing in ways that maintain their essential function, identity, and structure, while also maintaining the capacity for adaptation, learning, and transformation.” Given the inevitability of rising global temperatures for at least the next 2 decades, and probably longer, hospitals and health systems need to act now to become more heat resilient. When hospitals conduct their required hazard vulnerability analyses, as mandated by the Joint Commission, they should pay particular attention to assessing climate-specific risks such as EHEs, updating system-wide emergency plans and infrastructure, developing triage and treatment protocols, and ensuring clinical staff and first responders are appropriately trained and prepared. This also requires an assessment of the surrounding community to identify populations most vulnerable to heat and its possible consequences, such as loss of electrical power.
Building from key components of the U.S. Climate Resilience Toolkit, we discuss strategies and methods for health systems to better prepare for EHEs, to consider climate risks and community vulnerability assessments, to plan for essential clinical care services and care delivery needs, and to facilitate infrastructure protection and resilience planning ().
Actions taken in the cities of Ahmedabad and New York represent examples of leaders responding to the growing threat of heat waves and how to design climate resilience into health systems.
Ahmedabad and New York City Heat Safety Plans
Ahmedabad, with approximately 8.25 million residents, is the fifth-most populous city in India; it experienced severe heat waves in 2010 and 2016, recording temperatures of 50°C (122°F). Researchers predict that large regions of South Asia will exceed the survivability threshold of 35°C by the end of the century. (The survivability threshold is the upper limit at which humans can survive heat-humidity impacts under sustained exposure, after which the body loses its ability to cool itself.) New York City, with approximately 8.8 million residents, is the most populous city in the United States; it, too, has experienced repeated heat waves in recent years and can expect the number to increase from an average of two per year to seven per year by 2050.
Health system preparedness for the growing threat of heat waves and EHEs should be rooted in the concept of resilience.
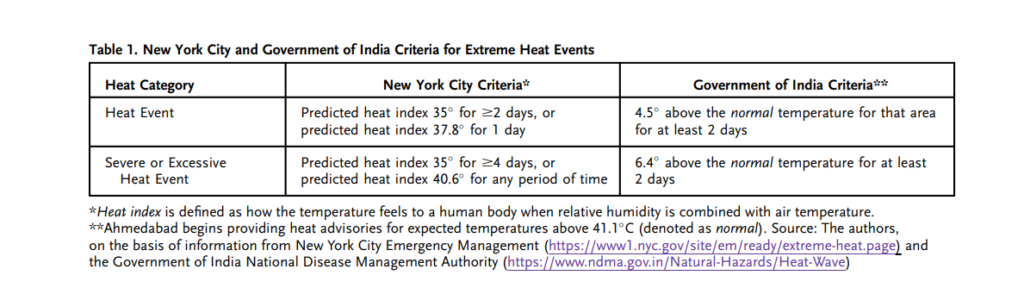
Understanding that preparation will be critical, Ahmedabad and New York City have developed heat action plans to coordinate local government response with other relevant government agencies, health care facilities, and community organizations. These plans become activated when formal thresholds (i.e., those identified by federal or city agencies) of excessive heat are met or exceeded ( Table 1).
Note that thresholds to activate heat safety actions/responses (e.g., heat advisories) are often not derived from location-specific epidemiologic data, with New York City and Ahmedabad being the exception rather than the rule. (Ahmedabad is based on Knowlton et al., and New York City is based on Benmarhnia et al.) Epidemiologic analyses have identified that the thresholds of health impact are highly variable across the world and within countries, regions, and states, and often do not align with the formal threshold definitions. The thresholds at which health is adversely impacted by heat depend on a region’s individual and population-level acclimatization to heat and variations in daytime and nighttime temperature. Defining these thresholds is central to developing heat safety plans because they determine when the plan is activated ( Table 1). Regional variations in heat-related hospitalizations provide critical information that can be used in developing place- and institution-specific heat response plans by anticipating patient volume on the basis of location-specific epidemiologic and meteorologic data.
Although the bulk of these plans focus on the public health response, hospital systems need to discuss and plan for their role in considering the preparedness of the surrounding community, health care professionals, and health care infrastructure. Lead times to a heat wave may vary from 72 to 24 hours. This time is needed to activate additional staff and resources at health systems to prepare for patient surges, especially patients needing emergency and critical care services.
Climate Risk and Community Vulnerability Assessments
Health systems could build more rigorous community-based collaborations to develop extreme heat response plans that incorporate traditional information about heat vulnerability (i.e., heat vulnerability maps) with community-derived knowledge about attitudes and practices among the populations most at risk in health care service areas. Understanding the characteristics of vulnerability also allows health systems to better target community benefit funding toward community resilience projects to mitigate the effects of extreme heat.
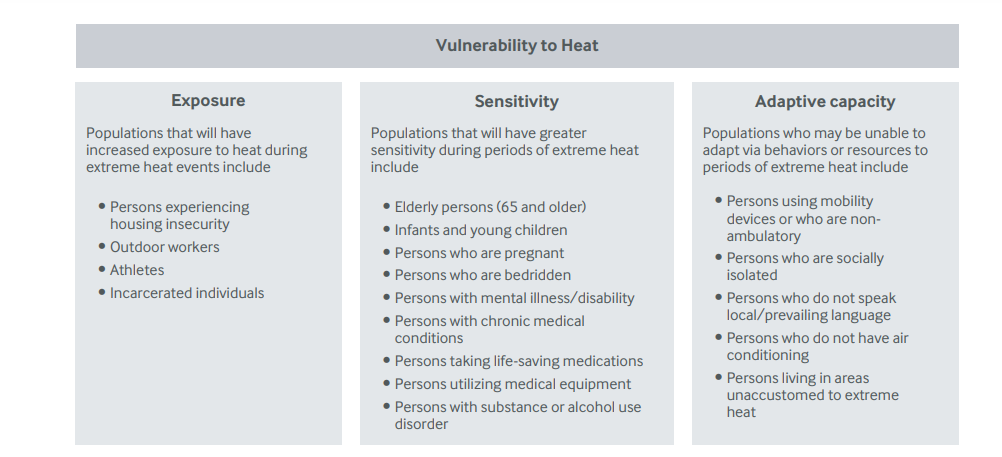
Those who are most at risk from extreme heat are often considered heat vulnerable. Whether a person is vulnerable to heat depends on multiple factors that contribute to exposure, sensitivity, and adaptive capacity-().
Social determinants of health such as race, income, employment, and language are factors that may be linked to the health risks of extreme heat. Elderly individuals, persons of any age who have chronic medical conditions, people who live alone, and those without access to air conditioning are at higher risk for adverse health effects of heat exposure. Infants and young children are more physiologically sensitive to extreme heat, owing to immature thermoregulation that increases their risk for mortality or to the inability to move independently to cool down (e.g., being confined in an overheated car). Pregnant individuals are at higher risk for premature birth, stillbirth, and lower infant birthweight. Outdoor workers and athletes are at risk for higher and longer exposures, often because of the nature of their physical activity and the time of day it takes place. Individuals who lack access to secure and stable housing are at higher risk for adverse outcomes as well.
In the United States, communities that experienced historical redlining, the intentionally discriminatory lending practice common in the early 20th century, record higher ambient temperatures today than do their nonredlined counterparts. Lack of tree canopies and limited investment in energy-efficient building infrastructure contribute to substantial temperature differences across urban areas. Under-resourced communities and neighborhoods with lower income and with higher concentrations of communities of color are often disproportionately hotter, placing individuals living in these communities at higher risk. In India, countries in Africa, and other lower-income countries, vulnerability to heat is also associated with a lack of access to safe drinking water or air conditioning and with living in densely populated urban dwellings or rural areas, among other factors.
Understanding that preparation will be critical, Ahmedabad and New York City have developed heat action plans to coordinate local government response with other relevant government agencies, health care facilities, and community organizations.
Despite gains in reducing heat vulnerability through the implementation of warning systems and increased awareness of heat threats, many communities remain challenged in identifying who is most at risk for heat-health hazards and where they are located. A common strategy utilized by public health practitioners and researchers that may be helpful in these situations is to map heat vulnerability. These maps can be created through a variety of methods,,but all typically include indicators of environmental and sociodemographic characteristics that are associated with adverse health outcomes during EHEs. The U.S. Centers for Disease Control and Prevention (CDC) Environmental Public Health Tracking Network provides an online tool that, depending on data availability, can map county-level measures of heat vulnerability and preparedness such as the number of hospital beds per 100,000. States such as Massachusetts, North Carolina, and Minnesota, among others, and cities such as New York City and Denver have developed community-specific heat vulnerability visualization tools. Such tools display the spatial distribution of population-level characteristics that are associated with heat vulnerability, providing users with a sense of where communities may be most at risk during a heat wave. For example, New York City’s hazard mitigation site includes a heat vulnerability map that shows the highest vulnerability in places that have little green space, which are most often communities of color.
In addition to mapping, vulnerability information can be collected via health surveys, analysis of mortality records or chronic disease registries, records of ambulance calls, and interviews and focus groups with government officials and health care professionals. This was carried out in Ahmedabad to identify populations at higher risk for poor outcomes, with outdoor workers, slum dwellers, and neonates identified as the populations at highest risk.
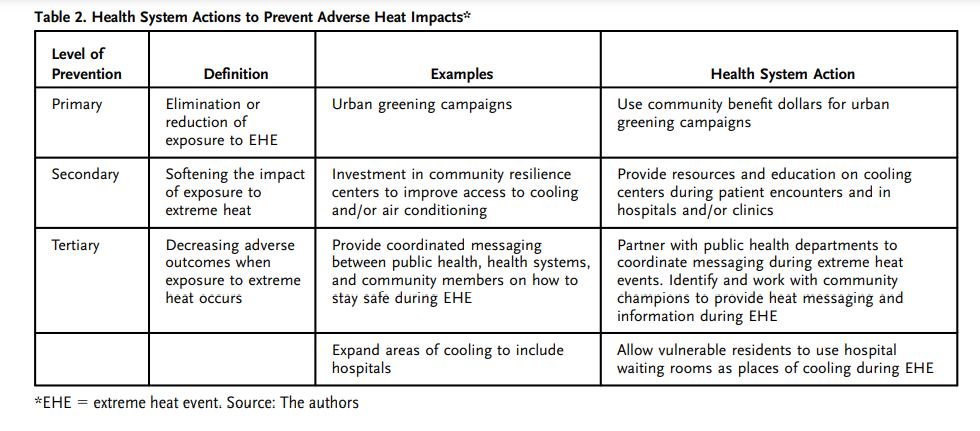
Health systems have an opportunity to leverage heat vulnerability information with community-led heat prevention activities that are socially and culturally appropriate among those who are most at risk during heat events. Tiers of prevention from the adverse impacts of heat can be considered as primary, secondary, and tertiary. Health systems have important roles to play in each level of prevention ( Table 2).
Primary prevention efforts such as urban greening campaigns that increase tree canopies and vegetation-covered surfaces can decrease daytime air temperatures and reduce population exposure to heat. Health systems could consider leveraging their community benefit dollars for such initiatives. Secondary prevention such as improving opportunities for cooling can reduce heat wave mortality for vulnerable populations. Community cooling shelters placed within vulnerable communities and broadly advertised, including in clinics and hospitals, can better prepare populations for extreme heat. Activities that reduce the exacerbation of heat-related morbidity or mortality — tertiary prevention — are a common response to extreme heat threats for hospital systems.
New York City and Ahmedabad are examples of how hospital systems in cities can work with local public health and preparedness experts to coordinate activities during EHEs. In many places, however, these relationships are not formalized or extended to community partners. In Ahmedabad, hospitals assist with raising public awareness by providing emergency service vehicles with displays that detail the dangers of heat exposure and the appropriate protective behaviors. Ahmedabad Municipal Corporation and cities throughout the United States also activate cooling centers during periods of extreme heat; health systems can advertise these centers to their communities by working closely with departments of public health and community organizations. In New York City, to help vulnerable residents find places to avoid heat exposure, the New York City Department of Homeless Services directs hospitals to allow patients to stay in waiting rooms during periods of extreme heat or to call a government assistance line to find a cooling center. Health systems can also consider creating a registry of individuals who are using electrically powered medical and life-supporting equipment at home to check on these patients in the event of an EHE or power outage.
Finally, health systems can build more rigorous community-based collaborations to develop extreme heat response plans that incorporate traditional information about heat vulnerability (i.e., heat vulnerability maps) with community-derived knowledge about attitudes and practices among the most at-risk individuals in the health care service area. For instance, community partnerships may identify heat champions — individuals the community respects to serve as a liaison — to provide heat messaging during events.,Similarly, these partnerships may help health experts determine the most appropriate methods to communicate heat risks to community members who may be most resistant to employing personal protective behaviors. Rather than the traditional top-down approach, health systems can leverage community-based relationships to enact tertiary prevention to save lives during EHEs.
Despite gains in reducing heat vulnerability through the implementation of warning systems and increased awareness of heat threats, many communities remain challenged in identifying who is most at risk for heat-health hazards and where they are located.
Essential Clinical Care and Services Delivery Planning
Train Health Care Providers to Recognize and Manage Heat Illness
During heat waves, EDs see a higher volume of patients, increased length of ED stay, and higher patient acuity, with length of stay being inversely associated with poorer outcomes. Even when health systems have mobilized resources, the surge of patients can overwhelm hospitals. Evidence suggests that even modest rises in temperature can increase ED usage for a broad range of heat-sensitive conditions. Furthermore, heat exposure has been associated with increases in the risk for ED visits for mental health disorders, self-injury/suicide, and intentional injury/homicide. During the Pacific Northwest Heatwave of 2021, there were nearly 1,800 heat-related ED visits across the state of Washington, with about one-fifth resulting in hospital admission, indicating that preparedness needs to extend beyond hospital walls.
Some recent analyses provide encouraging data suggesting that global heat-related mortality may be decreasing, possibly because of better early warning systems and recognition of heat casualties. However, significant variability in outcomes and data gaps persists, especially among vulnerable populations and in developing regions.
Heatstroke, the most serious heat-related emergency, requires rapid recognition and treatment to prevent permanent morbidity and mortality. The hallmark of heatstroke is the combination of central nervous system dysfunction and elevated core body temperature, defined as more than 40°C. During periods of heat stress, the body begins to sweat in an effort to maintain a stable core temperature. If heat is prolonged, and the body is depleted of electrolytes and hydration through sweating or insufficient rehydration, the core temperature begins to rise, compromising the body’s ability to thermoregulate. The failure of thermoregulation results in a systemic inflammatory reaction with multiorgan failure (renal, cardiac, and hepatic), disseminated intravascular coagulation, and central nervous system dysfunction. Dehydration can decrease end-organ perfusion, furthering injury. Medications that interfere with salt and water balance and circulatory function also increase risk.
EDs have alert systems for other high-risk, time-sensitive conditions to appropriately allocate human and hospital resources in a timely manner to improve patient outcomes. For example, sepsis and cardiac alerts are a component of quality incentive metrics for many EDs and have been shown to improve mortality. Stroke alerts expedite imaging and timely intervention. With these time-sensitive conditions, emergency medical services providers also participate in identifying and initiating treatment by alerting treatment teams to prepare for rapid, aggressive treatment prior to hospital arrival. The time sensitivity of treating heat stroke and the risk of severe complications warrants a similar approach, especially when considering the resource- and personnel-intense nature of therapeutic cooling and that EDs may be faced with many critically ill patients simultaneously during heat waves.
Currently, there is a lack of standardization and deployment of evidence-based protocols for the rapid triage and treatment of heat stroke victims. To address this gap, we undertook a systematic review of the literature pertaining to the recognition and management of heatstroke in prehospital, ED, and ICU populations and developed an evidence-based prehospital and ED-based heat-alert pathway to improve early diagnosis and resource mobilization. This protocol ensures that resources can be readily mobilized and that patient care tasks are clearly delineated, thus enabling the emergency and critical care teams to care for these patients efficiently and effectively without disrupting other critical tasks and operations. Hospitals must implement such protocols as part of their heat preparedness planning.
Rather than the traditional top-down approach, health systems can leverage community-based relationships to enact tertiary prevention to save lives during EHEs.
Develop Forms of Communication During EHEs to Share Resources and Information
During EHEs, the influx of patients, combined with stresses on the electrical grid and health care infrastructure, requires coordinated sharing of information and resources. In New York City, the Greater New York Hospital Association ( GNYHA), a trade association that includes all 55 hospitals located in New York City, is a key player in the health system response structure. GNYHA has been deeply involved in hospital emergency preparedness and response for 2 decades and has a permanent seat at the New York City Emergency Management (NYCEM) Emergency Operations Center (EOC). The city’s EOC is the central location for coordination among senior officials from city, state, and federal agencies, as well as other entities, during response efforts.
During responses, GNYHA shares critical information with its members to inform their readiness and response efforts, and collects information about clinical and operational impacts to inform its actions and those of government response agencies. In support of these functions, several years ago, GNYHA launched Sit Stat, a regional situational awareness and information-sharing platform that is now used by roughly 140 hospitals and more than a dozen city and state agencies across New York.
Sit Stat houses key contact, service line, and capability information for each facility, and it is used to rapidly collect information on operational impacts and needs during emergency events. With input from its Sit Stat Advisory Council, GNYHA has developed numerous hazard-specific event surveys, including an Extreme Temperatures Survey. The surveys ask a limited number of questions that provide actionable information to GNYHA, the hospital community, and the response agencies. The Extreme Temperatures Survey asks the three questions shown in Table 3.
If an EHE is forecast to impact New York City, the following generally happens:
- NYCEM activates the citywide Heat Emergency Plan and begins to convene a daily Heat Emergency Steering Committee Call in which GNYHA participates for the duration of the event. On that daily call, the the National Weather Service shares the forecast, and agency response actions are discussed.
- GNYHA then summarizes this information for hospital members via an Emergency Preparedness Bulletin that is emailed to key personnel within each member hospital and health system, including clinical and operational leaders, ED administrators, directors of facilities and engineering, and emergency managers. These bulletins also outline GNYHA’s planned use of Sit Stat surveys and any other planned actions.
Generally, GNYHA will deploy the Extreme Temperatures Survey at 9:00 a.m., with responses requested by 11:00 a.m., which allows GNYHA staff to report out hospital sector impacts during the 11:00 a.m. NYCEM Heat Emergency Steering Committee Call. The survey efficiently shows which hospitals are managing well on their own and which may be experiencing problems, enabling GNYHA and response agencies to focus their efforts accordingly. Such challenges may include increased patient volume in EDs or increased numbers of community members, including homeless individuals, seeking respite from the heat at hospitals. During periods of extreme heat, New York City hospitals are formally asked by the city’s Department of Homeless Services to accommodate individuals experiencing homelessness within dedicated waiting areas even if they do not require medical attention. Hospitals in New York City have established internal capabilities to meet this expectation but may sometimes be overwhelmed during a particular event and need additional support. In those instances, the hospitals can call a government line for help finding an appropriate cooling center for those individuals.
While the coordination of hospitals will vary in each region, hospitals can request that their appropriate associations play a role in facilitating communication, providing education, and building heat-specific surveys during EHEs to better coordinate support and resources.
Develop Buddy Systems with Regional Hospitals in Case of Power Outages
As mentioned previously, periods of extreme heat can lead to widespread power outages, potentially impacting health care facilities and their cooling systems. In accordance with standards and regulations, all hospitals have systems in place to maintain temperatures in patient care areas when a reduction or loss of power occurs. However, needs may arise related to a patient or community member surge or infrastructure and system impacts.
New York City hospitals, often in coordination with GNYHA, will contact response partners for assistance. The visibility of facility-level impact information facilitates support from GNYHA and response agencies. Hospitals additionally have agreements in place with other hospitals should a partial or full evacuation become necessary. While these agreements have historically centered on coastal storm scenarios, they provide a critical foundation for other hazards that may require patient evacuation, such as prolonged power outages.
Although hospitals are well positioned to weather short-duration power loss or reduction, extended outages are challenging and may require transfers of patients or wholesale evacuation. Hospitals are required to have emergency preparedness plans to address patient evacuation, with send-receive agreements outlined in the New York State Department of Health Facility Evacuation Planning Application. If additional resources are required, New York City and the region have plans and systems in place to support patient evacuation. In the event of a large-scale multifacility evacuation, GNYHA may also deploy predeveloped Sit Stat surveys to help facilitate regional coordination and bed matching across hospitals and health systems.
While coordination of hospitals will vary in each region, hospitals can request that their appropriate associations play a role in facilitating communication, providing education, and building heat-specific surveys during EHEs to better coordinate support and resources.
While New York City did not experience the extreme heat waves seen in other parts of the United States during the summer of 2021, it was nonetheless an eventful summer, with five heat events triggering activation of the city’s heat event response plan. Table 4 shows the dates of each heat event and the number of Sit Stat surveys that were activated for each.
Train Health Care Providers for Systems Preparedness
Emergency medical personnel, home health workers, and other first responders make up the front line responsible for recognizing, triaging, and managing heat-affected patients. However, an entire health system response — involving health care system administrators, clinicians, and other caregivers, as well as public health professionals — is necessary to protect community health. Recent studies have demonstrated that some emergency personnel are unprepared to recognize and manage the health complications of heat exposure. Certainly, ensuring that emergency medical care personnel are appropriately trained and practiced in recognizing and treating heat illness is foundational to decreasing morbidity and mortality. To this end, the Global Consortium on Climate and Health Education ( GCCHE) was launched in 2017, with now more than 260 schools across the globe having pledged to train their health professional students in climate and health. The GCCHE creates a set of highly vetted core competencies for health professionals, which include the ability to rapidly recognize and treat climate-related health emergencies such as the spectrum of heat illnesses ranging from heat exhaustion to heat stroke.
Notwithstanding this progress, more widespread educational efforts are needed, especially among existing health professionals. Leading health organizations, including the Association of American Medical Colleges ( AAMC) and the Accreditation Council for Graduate Medical Education ( ACGME), have the opportunity to accelerate health professional preparedness by mandating curricular requirements around climate change and health. In June 2021, the American Board of Pediatrics ( ABP) published a board maintenance of certification module, titled “The Impact of Climate Change on Pediatric Health Care.” By launching this module, the ABP is officially recognizing climate change as a foundational health issue affecting the clinical care of patients in ways that require dedicated education. More similar efforts are needed globally to bring all health care providers to a basic understanding of the health impacts of climate change.
Infrastructure Protection and Resilience Planning
Elements of infrastructure protection and resilience planning for heat waves include consideration of how communications, energy, water, and waste management capabilities could become vulnerable and which specific improvements would enhance their resilience to extreme heat, especially with regard to patient care. Hospitals should also consider how they can decrease their contribution to heat island effects, reduce their energy demands, and keep the inside of the hospital cooler by investing in green and cool rooftops. The U.S. Environmental Protection Agency (EPA) recommends green, or vegetative, rooftops, which can be 30–40°F lower than those of conventional roofs and offer a 0.7% reduction in building energy use. Other types of reflective rooftops (e.g., white China mosaic cool roofs) also offer cooling benefits. After successfully reducing heat stress using cool rooftops at its Shardaben Hospital in Ahmedabad, the Ahmedabad Municipal Corporation extended the initiative to all hospitals as part of its heat safety plan.
Elements of infrastructure protection and resilience planning for heat waves include consideration for how communications, energy, water, and waste management capabilities could become vulnerable and which specific improvements would enhance their resilience to extreme heat, especially with regard to patient care.
As hospitals consider other interventions to keep patients safe from extreme heat, vulnerability assessments also can help identify specific at-risk populations. For example, as part of the Ahmedabad Heat Action Plan, infants in the postnatal ward were identified as a highly vulnerable population during periods of extreme heat because of their location on the top floor of the Shardaben Hospital. Like a majority of hospitals in India, Shardaben Hospital is not air conditioned. After higher NICU admissions during the warmer months were observed (N=24), the maternity ward was moved to a lower floor and observed just four admissions in 2011. The reduced NICU admissions could have been the result of either the intervention or that temperatures were on average lower in 2011 compared with the heat waves in 2010. To account for this, the authors used a study model to show at the best fit temperature (42°C), moving the maternity ward to a lower floor was associated with a predicted 64% reduction in heat-related admissions to the NICU (95% confidence interval, 3%-89%).
Align Health Care Operations Around Carbon-Neutrality Goals
Although not explicitly a part of traditional resilience and preparedness planning, a discussion on climate change preparation would be incomplete without addressing the root cause: carbon emissions. Health care globally accounts for approximately 5% of carbon emissions. The health sector has the opportunity to lead on this issue to protect the health of the communities it serves and to encourage other sectors to do the same.
The National Academy of Medicine recently launched a call to decarbonize the health care sector, and the National Health Service in England is working with the World Health Organization on a plan to promote decarbonization of the health care sector around the world. Health care leaders must learn from these efforts in moving the mission and operations of their institutions toward becoming part of the solution.
Looking Ahead
As the climate crisis worsens, heat waves and EHEs will take an increasing toll on human health. Encouragingly, heat is increasingly being recognized as a killer that needs more attention and more coordinated responses. These efforts are taking various forms. For example, Seville, Spain, announced in 2021 that it plans, this year, to begin naming and ranking heat waves (as with hurricanes) in an effort to better raise awareness about the dangers of extreme heat. California is considering legislation to name heat waves on the basis of a ranking system that would mobilize resources to protect community health according to a heat wave’s ranking. As warning and activation systems improve and expand, health systems will have to consider their role and place in preparation for EHEs and treatment and prevention of their associated illnesses.
Mapping vulnerable populations, ensuring that these populations receive appropriate counseling and warning, and forming close partnerships and communication with organizations that can assist vulnerable populations during heat waves is perhaps one of the most essential undertakings of a health care system. As the recent Pacific Northwest experience with heat waves demonstrates, hospital preparedness for the influx of patients that result from an EHE is important, but health systems also have to invest in building community resilience to keep community members out of the hospital as much as possible.
Although this article focuses on heat waves, the climate crisis portends diverse and severe effects that will dictate that health systems create adaptable response plans tailored to local circumstances of geography, weather and climate, vulnerable populations, and compound events. The threats posed by climate change within each region will be unique, unpredictable, and varied, as demonstrated by the polar vortex that plunged Texas into freezing arctic temperatures or the combined heat and wildfire threats in California. Hazard vulnerability assessments that better integrate climate risks can help health systems make the difficult decisions on what investments are needed to improve climate change resiliency.
Finally, while a certain amount of harm has been locked in as a result of historical and ongoing carbon emissions, hospital systems have the opportunity now to prevent heat waves from growing substantially worse by being a part of climate solutions. Protecting our patients and communities from the harms of heat waves will take a multifaceted approach that should include preparedness but also mitigation for the overarching cause: climate change.
ABOUT THE AUTHORS
- Lisa Patel, MD, MEScClinical Assistant Professor of Pediatrics, Stanford Medicine, Stanford, California, USA; Deputy Executive Director, Medical Society Consortium on Climate and Health, George Mason University, Fairfax, Virginia, USA
- Kathryn C. Conlon, MPH, PhDAssistant Professor, Jointly Appointed in the Department of Public Health Sciences, UC Davis School of Medicine, and Department of Medicine and Epidemiology, School of Veterinary Medicine, University of California, Davis, California, USA
- Cecilia Sorensen, MDDirector, Global Consortium on Climate and Health Education, Columbia University, New York, New York, USA; Associate Professor, Emergency Medicine and Environmental Health Sciences, Columbia University Medical Center, New York, New York, USA
- Samia McEachinAssistant Director, Emergency Management Systems, Greater New York Hospital Association, New York, New York, USA
- Kari Nadeau, MD, PhDDirector, Sean N. Parker Center for Allergy and Asthma Research, Stanford University, Stanford, California, USA; Senior Director of Clinical Research, Division of Hospital Medicine, Stanford University, Stanford, California, USA
- Khyati Kakkad, MDProfessor and Division Head, Pediatrics Department, AMC MET Medical College, LG, Ahmedabad, Gujarat, India
- Kenneth W. Kizer, MD, MPHAdjunct Professor and Director, Climate Change Communications and Strategy, Sean N. Parker Center for Allergy and Asthma Research, Stanford University School of Medicine, Stanford, California, USA; Distinguished Professor Emeritus, Department of Emergency Medicine, UC Davis School of Medicine, Sacramento, California, USA
Originally published at https://catalyst.nejm.org on June 15, 2022.