BMJ Innovation
Shruti Murthy ,1 Prashanthi Kamath,2 Myron Anthony Godinho ,3 Nachiket Gudi ,4 Anil Jacob,5 Oommen John 6,7
27 February 2022
Abstract
Objective
To identify and summarise the digital health interventions (DHIs) implemented for non-communicable disease (NCD) management for COVID-19.
Design
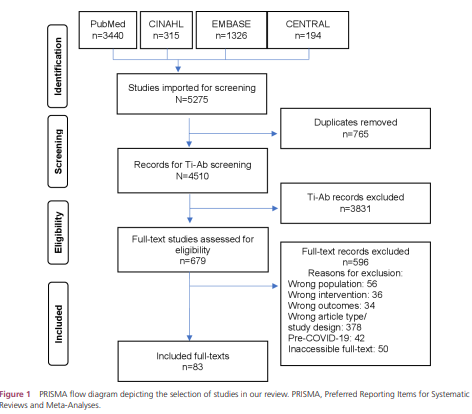
Rapid scoping review. Three reviewers jointly screened titles-abstracts and full texts. One reviewer screened all excluded records. Data were mapped to WHO DHI Classification and narratively summarised.
Data sources
PubMed, CENTRAL, CINAHL, EMBASE.
Eligibility criteria for selecting studies
Peer-reviewed primary research published between 1 November 2019 and 19 September 2021 on DHI for NCD management during the COVID-19 pandemic. Reviews, editorials, letters, commentaries, opinions, conference abstracts and grey literature were excluded.
Results
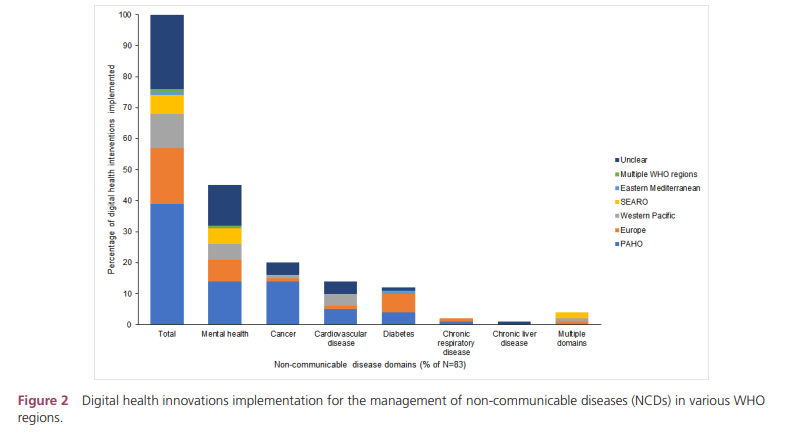
Eighty-three studies drawn from 5275 records were included. A majority of the studies were quantitative in design.
Forty per cent of the DHIs were implemented in the Americas.
Nearly half of these DHIs targeted mental health conditions.
A majority of the interventions were delivered remotely and via telephones. Zoom (26.5%), email (17%) and WhatsApp (7.5%) were the top three platforms for care delivery.
Telemedicine, targeted client interventions, personal health tracking and on-demand information services for clients were the most frequently implemented interventions.
Details regarding associated costs, sustainability, scalability and data governance of the DHI implementations were not described in the majority of the studies.
Conclusion
While DHIs supported NCD management during the COVID-19 pandemic, their implementation has not been equitable across geographies or NCDs.
While offering promise towards supporting the continuum of care during care delivery disruptions, DHIs need to be embedded into healthcare delivery settings towards strengthening health systems rather than standalone parallel efforts to overcome system level challenges.
While offering promise towards supporting the continuum of care during care delivery disruptions, DHIs need to be embedded into healthcare delivery settings towards strengthening health systems rather than standalone parallel efforts to overcome system level challenges.
Summary box
What is already known?
- The COVID-19 pandemic disrupted healthcare services, those with non-communicable diseases (NCDs) were disproportionately affected due to restrictive measures imposed to prevent SARS-CoV-2 transmission.
- Recent research has highlighted the role of digital health interventions (DHIs) for public health responses against COVID-19 and clinical care for COVID-19 and remote management in the context of pandemic.
- Reviews found that telemedicine was the most frequently employed intervention during COVID-19.
What are the new findings?
- Nearly half of the DHIs were implemented for the management of mental health/neurological disorders.
- Commonly available telecommunications tools (eg, telephones, internet-based short messaging tools and video calling platforms) were the most frequently used digital health innovations for NCD management during the COVID-19 pandemic.
- This review mapped the DHIs for NCD management and their need (ie, health system challenges during the COVID-19 pandemic) using WHO DHI v1.0 classification.
- Targeted client communication and personal health tracking were most popular for NCD management towards addressing gaps in utilisation, access and availability posed by the disruptions to routine health services delivery.
How this study might affect research, practice or policy?
- Need for focus on equitable distribution of DHIs for NCD management.
- Need for implementation research to explore sustainability of DHIs for NCD management.
- Need for transparent research reporting of financial, data governance and ethical aspects of DHI.
Need for focus on equitable distribution of DHIs for NCD management.
Need for implementation research to explore sustainability of DHIs for NCD management.
ORIGINAL PUBLICATION (excerpts of the full version)
Digital health innovations for non-communicable disease management during the COVID-19 pandemic: a rapid scoping review
BMJ Innovation
Shruti Murthy ,1 Prashanthi Kamath,2 Myron Anthony Godinho ,3 Nachiket Gudi ,4 Anil Jacob,5 Oommen John 6,7
27 February 2022
Introduction
COVID-19 has significantly impacted health systems globally. Containing the rapid spread of the SARS-CoV-2 has placed unprecedented demands on the health systems. 1
This sudden surge in demand coupled with pre-existing resource constraints and fragile healthcare delivery systems has disrupted routine healthcare services at all levels of the healthcare system. 1 2
Nearly every country experienced disruption in general healthcare services, with services in low/middle-income countries (LMICs) being affected the most. 3
In particular, this abrupt disruption of health services has significantly affected individuals living with non-communicable diseases (NCDs). 4 5
Health systems either ceased or scaled down services due to reasons such as: fear of contracting SARS-CoV-2 infections, repurposing of the health workforce for public health response and COVID-19 care, the conversion of NCD centres to isolation zones, closure(s) of health facilities for non-emergency conditions and enforcement of physical distancing norms such as lockdowns and travel restrictions. 6 7
The WHO’s rapid assessment survey in May 2020 found disruptions in 50% of NCD rehabilitative services in 163 countries during the pandemic. 1
Services for management of hypertension (53%), diabetes and its complications (49%), asthma (48%), cancer (42%) and cardiovascular diseases (CVDs) (31%) were affected.
Additionally, people living with NCDs are at risk of worsening of their NCDs. 8 9
This was attributable to disruptions in essential NCD support and treatment services, a lack of access to appropriate management for conditions during the pandemic and a drastic decline in the utilisation of, for instance, chemotherapy services and urgent referrals. 1 10–12
Furthermore, these disruptions are likely to adversely impact the achievement of multiple NCD-related targets of the 2030 Sustainable Development Goals. 9 13–15
Thus, it is crucial to ensure the continuity of care for people living with NCDs amidst this pandemic, keeping in mind the interlinkages between NCDs and COVID-19.
Thus, it is crucial to ensure the continuity of care for people living with NCDs amidst this pandemic, keeping in mind the interlinkages between NCDs and COVID-19.
This unprecedented situation has demanded novel solutions, adaptations or innovations in care delivery mechanisms to minimise in-person contact at the health facilities and promote remote care. 9 16
Reviews and WHO documents consistently highlight the need for innovations to respond to the (increasing) NCD burden during, and following, the COVID-19 era. 1 17
This pandemic has spotlight digital technologies as a vital tool to innovatively support the response efforts to COVID-19. 18 19
Additionally, our previous work has highlighted the importance of, and opportunities for, digital technological solutions to ensure a continuum of care for people with NCDs. 20 21
Many reviews on digital health interventions (DHI) for NCD management have focused on a subset of NCDs (eg, the use of telemedicine for mental health or neurological disorders 22 23), a specific time period within the pandemic (eg, technologies implemented in the first COVID-19 wave 17) or a subset of DHIs (eg, use of smartphones to ensure continuity of care during this pandemic 24).
There is a need to build on these efforts and broaden the horizon of our understanding of technological innovations for NCD management during health emergencies such as COVID-19 pandemic.
This pandemic has spotlight digital technologies as a vital tool to innovatively support the response efforts to COVID-19
In such a situation, we assessed that a scoping review was an appropriate and important first step to (1) comprehensively review, and map from, the breadth of available literature the DHI implemented during this pandemic for the management of various NCDs, (2) map the range and functionalities of the DHI and (3) to identify the gaps to inform future research efforts. 25–28
The rapid nature of the review will provide a timely and relevant response to the call for the ‘Innovations in Non-communicable diseases’ supplement by BMJ Innovations.
This call highlighted the need and importance of understanding innovations for this pandemic. 29
We thus designed a rapid scoping review with an objective to identify, map and summarise, in a timely manner, the global DHI for people with NCDs during the COVID-19 pandemic.
This call highlighted the need and importance of understanding innovations for this pandemic.
Methodology
See the original publication
Discussion
This rapid scoping review identifies and summarises the attributes of digital health innovations implemented for the management of NCDs during the COVID-19 pandemic.
The most frequently targeted NCDs related to mental health, neurological or neurodevelopmental conditions.
Telemedicine was the most frequently implemented intervention. Telemedicine or telehealth has been widely used during this present COVID-19 pandemic for its long-lasting ‘remote’ care continuity solutions for NCDs such as cancer, 42 mental health 43 and spiritual support for critical or end-of-life situations. 44 A scoping review on technologies for any health condition in the first COVID-19 wave similarly found telemedicine as the most frequently implemented technology (85%). 17
The demand for innovations was amplified multifold during this pandemic, especially because of the mobility restrictions imposed by the governments to contain the spread of SARS-CoV-2.
This in turn adversely affected the continuity of care for people living with NCDs.
Using the WHO DHI classification helped us identify the key elements that are likely to impact the large-scale DHI implementation including financial aspects, sustainability and broader data governance requirements for overcoming regulatory restrictions across geographies.
The WHO DHI classification v 1.0 is vital to categorise technologies implemented to support needs of the health system and is especially useful for evidence synthesis approaches among others. 36
Despite some challenges in broader application and/or adoption by particular stakeholders involved in clinical care, 45 mapping the DHIs to their corresponding health system challenges promotes an understanding of the deployments and their needs. 36
This endeavour can provide a shared language to inform planners, decision makers and researchers about the ‘functionalities of digital health implementations’ for NCD management, 25 especially for rapid implementation in health emergencies such as the COVID-19 pandemic.
We found that targeted client communications, personal health tracking and on-demand health information services for clients were the three most frequently used client interventions.
This is expected since our review focused on management of special groups of people, in particular, those diagnosed with NCDs.
The latter two interventions reflect the need for continuation of monitoring and supportive services-a critical component of continuum of NCD care during the COVID-19 pandemic.
The pandemic has also resulted in significant lifestyle changes for people living with NCDs, especially among those with diabetes and with risk factors of cardiovascular diseases. 12
Interventions for self-management will be important to mitigate the worsening of existing conditions due to, for instance, limited opportunities for outdoor physical activities due to the closure of parks and gymnasiums. 12
We found that commonly used communication tools were the most frequently used interventions for health services delivery during the pandemic for the management of NCDs.
As found in our review, repurposing of the available communication channels (eg, Zoom, WhatsApp, telephones) to ensure continuum of care during the COVID-19 pandemic. 17
We additionally found emails to be a popular medium for health services delivery and continuum of care.
Innovative practices need not be always inventive in nature; advances that are initiated and evaluated rigorously in other jurisdictions add to the evidence base of effective public health programmes in order to be scaled-up and implemented more widely.
Rapid deployment of novel health innovations during public health crises has been described previously. 46 47
Our review noted that telemedicine was the most commonly used digital health innovation for NCD management during the pandemic.
This is no surprise as telemedicine offers multiple advantages, particularly relevant in this COVID-19 pandemic, that Dorsey et al refer to as its 5 Cs:
- ‘accessible care,
- increased convenience,
- enhanced comfort,
- greater confidentiality,
- educed risk of contagion’. 48
However, some of the challenges they and the telemedicine literature highlight hold relevance to our findings broadly.
These have to do with technological barriers, digital literacy, financial and security aspects. 17 42 48–52
We found an inequitable regional distribution in DHI implementation with most implementations in the Americas, especially the USA.
This is similarly reported in other studies and possibly reflects the technological advancement of the countries and the regional SARS-CoV-2 burden. 1 17
Furthermore, studies in our review either required segments of the population facing technological barriers to continue with in-person visits, or provided technological support (ie, donated or funded).
Additionally, financial and security challenges exist particularly when DHIs collect, manage, store or transmit client health information; a majority of the DHIs in our review incorporated one or more of these functions.
However, the majority of the DHIs in our review did not adequately address or report these design aspects.
However, some of the challenges they and the telemedicine literature highlight hold relevance to our findings broadly. These have to do with technological barriers, digital literacy, financial and security aspects.
The absence or presence of (access to) reliable technology, finances, digital literacy and motivation, thus determine inclusion and uptake for many DHIs. 53
Needless to say, a complete shift to telemedicine without addressing the above challenges will only worsen existing inequities in access and disease outcomes. 17 42 50 51 53
Digital technologies are increasingly being recognised as critical innovations to strengthen health services delivery systems. 54–56
Thus, it becomes imperative to address the above aspects for scalability and continued uptake, considering the widespread use and integration of telemedicine in routine NCD care. 49
COVID-19 restrictions made digital solutions necessary in many social sectors, and this society-wide transition is poised to significantly change the ways in which whole societies engage in, and enact health. 57
Despite years of consistent efforts for the mainstreaming of DHIs, the health service delivery disruptions during this pandemic forced the health systems to pivot towards digital innovations for NCD-focused care delivery. 58
The absence or presence of (access to) reliable technology, finances, digital literacy and motivation, thus determine inclusion and uptake for many DHIs.
Despite years of consistent efforts for the mainstreaming of DHIs, the health service delivery disruptions during this pandemic forced the health systems to pivot towards digital innovations for NCD-focused care delivery
This review highlights the considerable capacity for health systems to undertake this shift.
However, sustaining these interventions beyond mere pilot projects has been a long-standing challenge for digital health implementors. 59
This review highlights the considerable capacity for health systems to undertake this shift.
However, sustaining these interventions beyond mere pilot projects has been a long-standing challenge for digital health implementors.
Regular monitoring and evaluation of digital health innovations is the first step towards ensuring effective and safe DHI implementation, and several toolkits are available for this purpose. 60
In the long term, embedding DHIs within healthcare delivery systems is a promising approach for their sustainabilty, 61 and DHIs can effectively support integrated care models for NCDs. 62
Regular monitoring and evaluation of digital health innovations is the first step towards ensuring effective and safe DHI implementation, and several toolkits are available for this purpose.
In the long term, embedding DHIs within healthcare delivery systems is a promising approach for their sustainabilty, and DHIs can effectively support integrated care models for NCDs
The WHO’s framework on Integrated People-Centred Health Services outlines an approach to institutionalising DHIs within digitally augmented, comprehensive care through supportive policies, sustainable financing, a suitably trained workforce and reliable infrastructure. 63
It is also important that the DHI interoperates seamlessly with other DHIs within the broader digital health ecosystem, highlighting the importance of coding languages and interoperability standards. 64
It is also important that the DHI interoperates seamlessly with other DHIs within the broader digital health ecosystem, highlighting the importance of coding languages and interoperability standards
Finally, we bring attention to the use of the term ‘health innovations’, defined by the WHO as one that ‘aims to develop and deliver new or enhanced health policies, systems, products, technologies, services and delivery methods to improve people’s health’. 65
Innovations are multifaceted in nature and are continuously being prototyped, piloted and deployed at scale or adapted to cater across services for a long time in tune with the healthcare sector challenges.
A consensus across the literature is that to be an innovation would mean for it to be ‘patient-centric’ and to bring in ‘something new or significantly different from other solutions in the field’. 65–72
Many studies in our review loosely referred to the need and/or use of innovations, and were limited by an inadequate description of ‘innovation’.
On the other end, elaborate accounts brought clarity regarding the need, design (eg, using service design methods) and implementation of novel solutions.
We thus support the call to researchers to explicitly define the need and design of their innovations in order to prevent a dilution of its meaning. 70
Finally, we bring attention to the use of the term ‘health innovations’, defined by the WHO as one that ‘aims to develop and deliver new or enhanced health policies, systems, products, technologies, services and delivery methods to improve people’s health’.
This is the first rapid scoping review identifying global digital health literature for NCD management during the COVID-19 pandemic, and mapping it to WHO DHI Classification, to the best of our knowledge.
While expediting the review, we incorporated measures for quality assurance for the review. Search strategies, screening protocol and data abstraction template were developed based on standard scoping and rapid review guidelines and literature review, 17 30–33 73 74 pilot-testing, multiple discussions within a team experienced in content and methods. To minimise selection bias, we standardised procedures, trained and calibrated the team, and had one reviewer screen all excluded records. Mapping of studies to WHO DHI classification was performed by review members experienced in digital health and the WHO DHI classification tool (MG and NG). 51 We used a comprehensive search strategy to minimise the risk of missing potential inclusions. However, we acknowledge that potentially relevant studies may have been missed because of the rapid nature of the review (eg, author contact for additional information, screen reference lists of included studies, seek grey literature/non-English language studies/ conference abstracts).

Conclusion
This review outlines the considerable progress made in digital health service delivery for NCDs during the COVID-19 pandemic, while noting the potential challenges to scale-up and wide spread adoption of DHI for NCD management.
Health systems, despite their constraints, have made considerable efforts to continue service provision despite systemic disruptions.
We have highlighted the important role of commonly available telecommunication tools for NCD management during the COVID-19 pandemic.
Broadly, DHIs offer a promising and sustainable approach to NCD management.
However, the distribution of DHI implementation for NCD management has not been equitable geographically or across NCDs, with certain regions (such as the Americas) and NCDs (eg, mental health conditions) documenting far more innovations than others.
As the pandemic wears on, it is important that the diffusion of such innovations for NCD management reach those in LMICs where the need for them is greatest.
This presents a noble and worthwhile agenda for more research and implementation of DHIs for NCDs as the health systems gear towards building back better beyond the COVID-19 pandemic.
Originally published at https://innovations.bmj.com on April 26, 2022.
About the authors & affiliations
Shruti Murthy ,1
Prashanthi Kamath, 2
Myron Anthony Godinho ,3
Nachiket Gudi ,4
Anil Jacob ,5
Oommen John 6,7
1 The George Institute for Global Health India, Hyderabad, India
2 The George Institute for Global Health India, New Delhi, India
3 WHO Collaborating Centre for eHealth, School of Population Health, UNSW Sydney, Sydney, New South Wales, Australia
4 Independent Researcher, Bengaluru, India
5 George Institute Services, New Delhi, India
6 George Institute for Global Health, UNSW, New Delhi, India
7 Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, India













