Health Policy Watch
Kerry Cullinan
09/09/2021
Image Credits: NCD Alliance, WHO/A. Loke.
Health services in low and middle-income countries have yet to adapt to their growing burden of non-communicable diseases (NCDs) and still prioritise infectious diseases, according to a new launched on Thursday by the NCD Alliance.
Treatment “silos” for HIV and tuberculosis need to be transformed into integrated universal healthcare services to better serve people in LMICs, many of whom are living with both infectious diseases and NCDs, according to the report.
“COVID-19 has brought about a greater recognition that the long-held distinctions between infectious and non-communicable diseases are not as clear cut as once thought — those with chronic conditions have a significantly higher risk of hospitalisation or death from the virus,” according to the NCD Alliance.
… those with chronic conditions have a significantly higher risk of hospitalisation or death from the virus,”…
The vast majority of people who have become seriously ill or died from COVID-19 had an underlying condition, particularly hypertension, cardiovascular disease and diabetes, it notes.
The vast majority of people who have become seriously ill or died from COVID-19 had an underlying condition
Integrated care ‘is the future’
“We urgently need a reset of healthcare delivery in poorer countries that actually reflects the needs of those who need it most,” said Katie Dain, CEO of the NCD Alliance.
“Integrated care is the future of healthcare. The reality today is that ever more people are living with multiple chronic conditions. This needs to be better recognised in health systems.
The reality today is that ever more people are living with multiple chronic conditions.
Dain added that infectious diseases and NCDs were entwined:
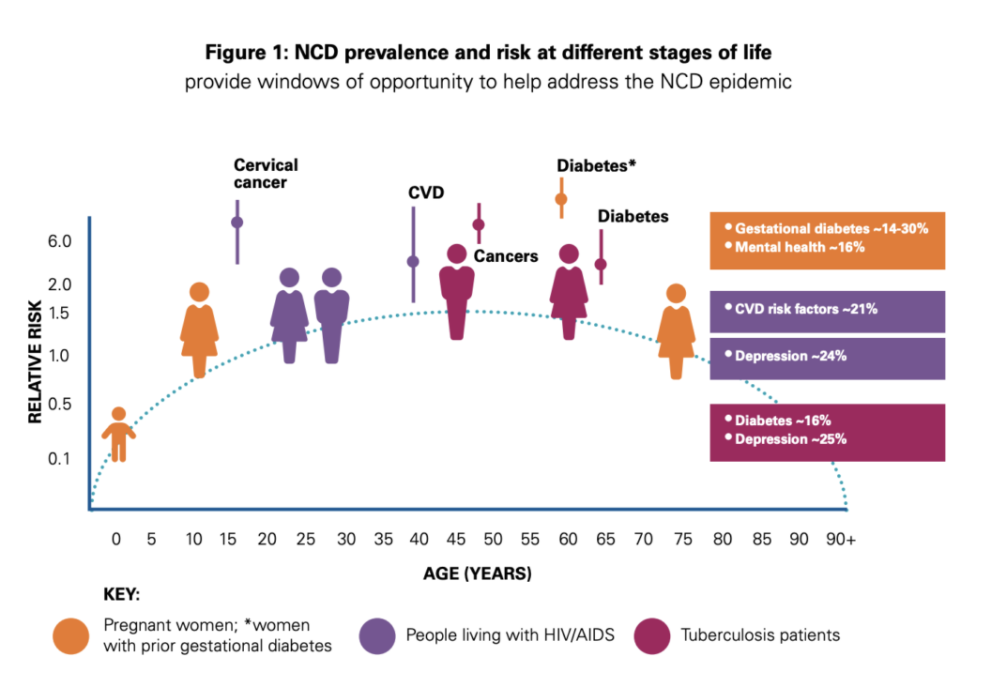
- “People living with HIV have a significantly higher risk of cardiovascular disease and some cancers.
- People living with TB are much more susceptible to diabetes and vice-versa.
“Hypertensive disorders and gestational diabetes affect many pregnancies, risking potential lifelong health impacts for both mother and child if not effectively treated.”
“LMICs are experiencing a rapid transition from population disease profiles shaped by communicable diseases and conditions impacting mothers and their children, to those dominated by NCDs and injuries.
Today, 85% of people dying from NCDs between ages 30 and 70 are in LMICs,” according to the NCD Alliance.
One in three diseases among the poorest billion people in the world are NCDs, according to the Lancet NCDI Poverty Commission.
- Cardiovascular diseases account for most NCD deaths (17.9 million people annually),
- followed by cancers (9.3 million),
- respiratory diseases (4.1 million),
- and diabetes (1.5 million).
These four groups of diseases account for over 80 percent of all NCD deaths before the age of 70.
“Health centres that reflect this changing epidemiology are the future,” said Dain. “But this will also mean that we have to change the way we do business.
“Health centres that reflect this changing epidemiology are the future,” said Dain. “But this will also mean that we have to change the way we do business.
The COVID-19 pandemic has been catastrophic for people living with NCDs and it is clear we need a health infrastructure in LMICs that is fit for purpose if we are to build back better.”
HIV, TB funding influences health system
The report’s lead author, Dr Gill Schierhout from the George Institute for Global Health, said that many LMIC health systems were still influenced by funding for HIV, TB, malaria and maternal health.
“The shape of this [funding] has critical impacts on the health care available — or not available — for the growing number of people who are living with NCDs in LMICs,” said Schierhout.
The report was based on an online survey that was sent to health workers in LMIC.
Survey respondents identified that there were particular challenges posed by
- staffing siloes, and
- organisational ambivalence around the integration effort.
In addition, specialist managers of global health initiatives are sometimes “well versed in disease-focused areas, but not as well versed in whole-of-person care or primary health care.
… specialist managers of global health initiatives are sometimes “well versed in disease-focused areas, but not as well versed in whole-of-person care or primary health care.
Therefore, programmes often struggle to gain the necessary management support”, according to the report.
However, the report documents a number of integration successes.
- In Zambia, for example, a cervical cancer screening has been integrated into an HIV care programme.
It modelled that, for every 46 HIV-positive women screened, a woman’s life was saved who otherwise would likely have died of undetected cervical cancer.
More than a decade ago Ministers of Health resolved at the first UN High-Level Meeting on NCDs to “encourage the development, integration and implementation of vertical programmes, including disease-specific programmes, in the context of integrated primary health care”.
“However, progress in this area has been patchy at best,” noted the NCD Alliance.
Originally published at https://healthpolicy-watch.news.
Names cited:
Katie Dain, CEO of the NCD Alliance;
Dr Gill Schierhout, from the George Institute for Global Health
TAGS: NCDs, Integrated Care, Primary Care;












