This is an excerpt of the publication below, with the title above, focusing on the topic in question.
Philips
June, 2022
The Future Health Index is commissioned by Philips
Edited by
Joaquim Cardoso MSc.
Health Transformation . Institute
Research Institute for Continuous Health Transformation
June 13, 2022
Emerging from the pandemic, healthcare leaders reassess their needs

1.A much-needed refocus on staff
The pandemic has exacerbated the difficulties faced by healthcare leaders before the crisis.
Today, healthcare leaders face a human capital crisis: the ‘great resignation’ has serious consequences for the industry, leading to the closure of facilities, in some cases.
This is an issue that must be addressed in order to fix other challenges.
2.Evolving the approach to care delivery
The pandemic has led healthcare leaders to act with agility, build resilience and adopt smarter ways of working to help future-proof care.
It has also pushed them to rethink how care is delivered.
In many cases, healthcare leaders have continued to use care practices that were adopted more widely during the pandemic, including virtual care.
“In the hospital sector, the COVID situation hit us hard… future investments fell behind a bit… we are now clearly looking to the future again.” — Operation Room Department Head, Urban hospital, Germany
1.Healthcare leaders refocus on staff satisfaction and retention
2.Expanding care beyond hospital walls gains momentum
3.Tackling health inequalities within the community
4.Embarking on a fast track to sustainability

1.Healthcare leaders refocus on staff satisfaction and retention
Tackling the human capital crisis is top of mind
Employee retention is a serious issue in healthcare systems across the world: global demand for healthcare workers is predicted to rise to 80 million staff by 2030[1].
With supply of healthcare workers expected to reach just 65 million over the same period, this leaves a significant[2] 15 million shortfall.
Driven by aging populations and economic and population growth, this demand is anticipated to be highest in middle-income countries.
Employee retention is a serious issue in healthcare systems across the world: global demand for healthcare workers is predicted to rise to 80 million staff by 2030[1].
With supply of healthcare workers expected to reach just 65 million over the same period, this leaves a significant[2] 15 million shortfall.
Coupled with this is the departure of staff: more than half of all healthcare workers worldwide are experiencing burnout that, if not addressed, could cause many to leave their fields[3].
The consequences of poor staff retention are severe and include high costs associated with replacing staff, which affect patient care and staff morale.

This may explain why staff satisfaction and retention are, together, top of healthcare leaders’ priority lists, both today and three years from now (30% today, 28% in three years).
However, the underlying reasons behind this vary from country to country.
In the United States, for example, it is driven by the ‘great resignation’ and competing salaries from other sectors.
In India, it is the ever-increasing demand for more healthcare professionals that is the driver, …
… while in China the priority is focused around the specific need for doctors and nurses.
Investing in technology can help alleviate the burdens faced by healthcare professionals
The Future Health Index 2020[4] report found that younger healthcare professionals who work in smart facilities are more likely than their peers in both digital and analog facilities to be satisfied in their work.
By placing such an emphasis on technology in their facilities, leaders are likely to be simultaneously improving staff experience and satisfaction.
… younger healthcare professionals who work in smart facilities are more likely than their peers in both digital and analog facilities to be satisfied in their work.
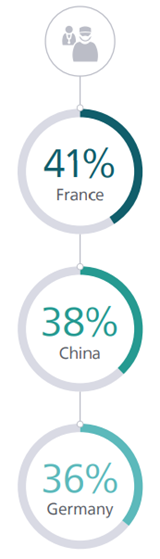
Three countries stand out as prioritizing staff satisfaction and retention the most three years from now
“A job that takes two people to complete is being given to only one person to do. It must be hard for our staff.”
Department Head of Neurology, Urban hospital, China
Three countries stand out as prioritizing staff satisfaction and retention the most three years from now

2.Expanding care beyond hospital walls gains momentum
Extending care is another top priority for leaders
The value of delivering care beyond hospital walls was in evidence during the pandemic[5], with digital tools such as contact tracing apps and telehealth consultations helping to keep communities safe while ensuring continuity of care.
Today, healthcare leaders view extending care delivery as their highest priority after staff satisfaction and retention.
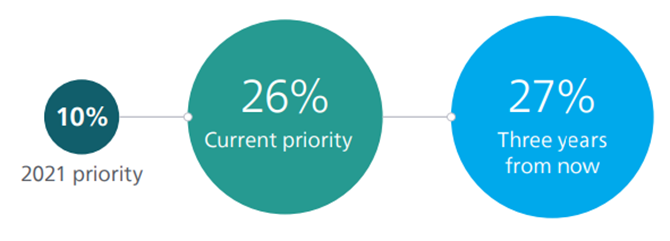
This reflects the Future Health Index 2021 report, which found that 24% of healthcare leaders would prioritize extended care in the following three years.
This reflects the Future Health Index 2021 report, which found that 24% of healthcare leaders would prioritize extended care in the following three years.
Notably, there is also a continuing acceleration in the rise in ambulatory care, one of the fastest-growing segments of the healthcare industry[6].
…there is also a continuing acceleration in the rise in ambulatory care, one of the fastest-growing segments of the healthcare industry
This focus is also closely aligned with the Quadruple Aim as it meets the needs of both patients and staff, while improving outcomes and considerably reducing costs.
“We see an increasing shift in care outside of the big box hospital model and into the home setting.”
Chief Operating Officer, Urban hospital, Australia
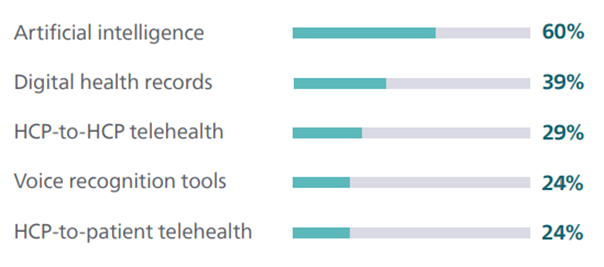
To deliver this care, leaders continue to invest in enabling technologies
These technologies include digital health records, telehealth and artificial intelligence (AI) tools that can enhance efficiency, improve care and connect remote communities.
Such technologies remain a top investment for healthcare leaders, highlighting how leaders are building on advances made during the pandemic when telehealth played a key role.
These technologies include: (1) digital health records, (2) telehealth and (3) artificial intelligence (AI) tools — that can enhance efficiency, improve care and connect remote communities.
The pandemic spurred a huge surge in investment in telehealth.
A 2020 analysis[7] by Frost & Sullivan found that the telehealth market in the US alone was predicted to display seven-fold growth by 2025.
In 2021, 64% of healthcare leaders were investing in it.
Now, with the technology already in place, healthcare leaders are looking to secure the right technology infrastructure to ensure they get maximum value from telehealth.
Now, with the technology already in place, healthcare leaders are looking to secure the right technology infrastructure to ensure they get maximum value from telehealth.
Extending care delivery has grown to be a priority today and three years from now
Digital health records and AI are the leading digital technology investments today

3.Tackling health inequalities within the community
Healthcare leaders are prioritizing social responsibility
Health inequalities are complex and far-reaching, and affect a broad range of communities. Key factors include socioeconomic status, geographic location, race and ethnicity, and gender and sexual identity.
The pandemic highlighted health inequalities across society, leading to a call from the World Health Organization for global action to address such issues[8].
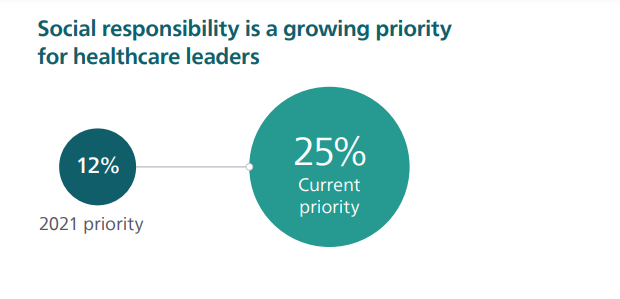
This year’s research found that social responsibility, including addressing health inequalities, has become one of healthcare leaders’ top priorities both now and in the future.
One-quarter (25%) of healthcare leaders say that being a socially responsible healthcare provider is one of their primary responsibilities and, in many cases, are already acting on this sense of responsibility.
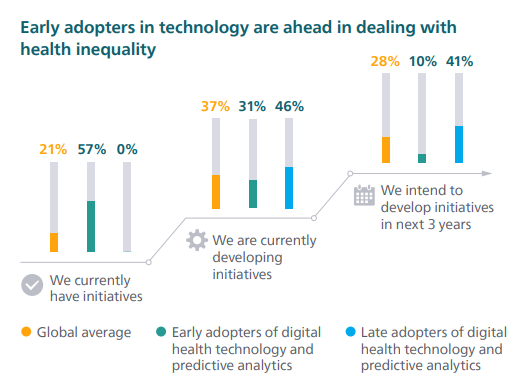
Over half (58%) say they either have initiatives in place to help tackle health inequity or are currently developing such initiatives.
A recent snapshot[9] of the ways US hospitals are working to limit health disparities showed community outreach programs, healthy food access schemes, volunteering, and diversity and inclusion planning.
These activities are mirrored in private sector hospitals around the world
Technology plays a part in tackling such disparities
Over two-thirds (68%) of healthcare leaders say that the use of predictive analytics can have a positive impact on health inequality.
For example, predictive analytics can provide fast and accurate insights around risk scores and collective health issues. These insights help to proactively identify groups of people at risk, particularly among poorer and more vulnerable groups. Hospitals are then able to incorporate this information into planning for community health issues such as disease outbreaks and cancer incidence, improving the healthcare delivered to these underserved groups.
Underlining this link, healthcare leaders who say they are early adopters of technology and predictive analytics are more likely than those who are late adopters to have initiatives to deal with health inequalities in place, highlighting how technology adoption can address health inequality.
With two-thirds of the world’s population lacking access to basic medical imaging technology[10], one initiative that is making a difference by bringing quality care to patients in need is PURE, a non-profit organization dedicated to enhancing ultrasound education and use in the developing world.
Participating physicians in the US and Europe use tele-ultrasound to support emergency medicine residents in Kigali, Rwanda, who in turn share their learning with healthcare professionals in rural areas, boosting the country’s emergency medicine facilities.
Why addressing health inequalities is on the agenda
Health inequalities have been sharply magnified in the past two years. Those from minority communities experienced disproportionate rates of illness and death due to COVID-19.
This is attributed[11] to increased risk of exposure to the virus due to living, working and transportation situations.
They also faced greater risk of experiencing serious illness if infected due to higher rates of underlying health conditions.
The social and economic effects of the pandemic also threaten to reverse progress toward gender equality, with a recent global study reporting increased disruptions in reproductive health services, as well as finding that women have experienced negative social and economic[12] impacts to a greater extent than men.
At a global level, acute issues such as poor supply and limited infrastructure are now under greater scrutiny, with healthcare leaders and governments under increasing pressure to respond.

4.Embarking on a fast track to sustainability
Healthcare leaders are prioritizing environmental sustainability
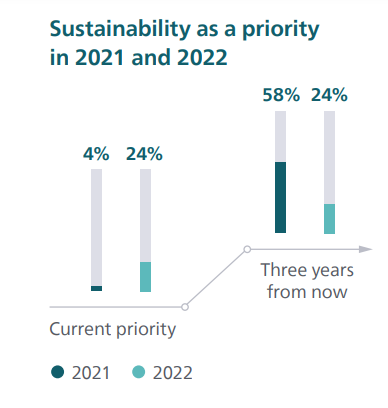
The Future Health Index 2021 report found that just 4% of healthcare leaders saw implementing sustainability practices as a priority, although many (58%) agreed it would become a priority by 2024.
Today, the picture is very different.
This year’s findings suggest that healthcare leaders have fast-tracked their sustainability plans. Almost one-quarter (24%) are prioritizing sustainability, and the same number plan to do so three years from now.
This shift may be explained by both the public commitment of 50 countries to develop climate-resilient and low-carbon health systems as part of the COP26 Health Programme[13] in late 2021, and a resetting of expectations as leaders embark upon implementing their sustainability plans.
Healthcare leaders in urban facilities are more likely than their peers in rural facilities to prioritize sustainability (26% vs 19%), demonstrating the role of patients and healthcare workers in driving sustainability.
In urban areas where there is a wider choice of facilities, healthcare leaders are more likely to feel pressure to meet patient demands for sustainable practices in order to attract and keep patients[14].
Equally, sustainability is increasingly playing a key part in recruiting talent in areas where there is significant competition.
However, while leaders in rural facilities are currently behind those in urban facilities in prioritizing sustainability, they are set to surpass them in terms of the issue three years from now (29% vs 25%).
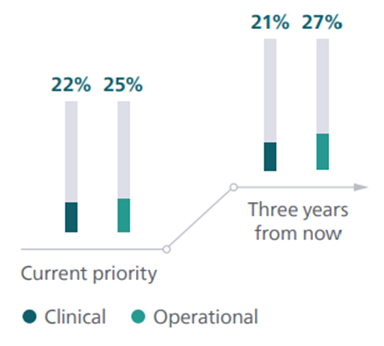
There are also differences in attitudes towards sustainability between operational and clinical healthcare leaders
Clinical leaders are less likely to prioritize sustainability than their operational colleagues today and this difference is even greater in the future.
However, they can also have an impact on emissions reductions, for example by prescribing medications that are manufactured with a lower carbon footprint or advocating for equipment that has zero landfill at the end of its life.
For hospitals and healthcare facilities to achieve their sustainability goals, both clinical and operational leaders must play an equal part in carbon reduction.
Operational leaders taking the lead in addressing sustainability
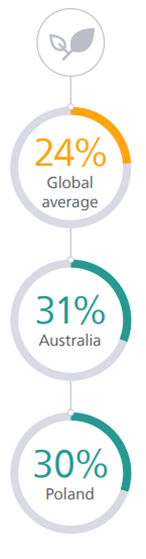
Healthcare leaders in Australia and Poland are ahead of most other countries in prioritizing sustainability
The role of sustainability in healthcare
With the healthcare industry being one of the most carbon-intensive industries, leaders have long faced calls to adopt more sustainable practices.
The supply chain is one of the most important areas on which to focus.
Other common initiatives include increased use of renewable energy, expanding the circularity of products and materials, efficient construction practices, and replacing harmful chemicals with safer alternatives.
Organizations such as Health Care Without Harm[15] are leading the growing demand for sustainability with a range of initiatives, including tools for facilities to control their waste management and education programs on the health impacts of climate change.
References
See the original publication
Originally published at https://www.philips.com












