Frederick Health is leveraging integrated genomic data within patient records to enhance precision medicine and clinical decision-making.
Site Editor:
Joaquim Cardoso MSc.
Health Institute — for continuous health transformation
October 4, 2022
Health IT Analytics
October 04, 2022
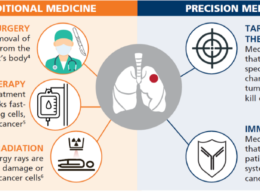
Genomics and precision medicine are exciting prospects for healthcare organizations looking to personalize care to improve disease prevention and clinical outcomes for their patients.
However, implementation and utilization remain a challenge for providers.
Research suggests that ever-evolving risk factors significantly impact the burden of chronic and acute diseases.
These factors must be effectively minimized to support long-term population health.
To mitigate these risks, researchers suggest incorporating data-driven health management strategies, such as precision medicine, into clinical decision-making.
Research suggests that ever-evolving risk factors significantly impact the burden of chronic and acute diseases.
To mitigate these risks, researchers suggest incorporating data-driven health management strategies, such as precision medicine, into clinical decision-making.
In combination with evidence-based medicine, including precision medicine as an approach to clinical decision-making has the potential to advance personalized care and improve outcomes.
Still, hurdles such as bias and evaluation of ethically actionable risk factors can stand in the way.
In combination with evidence-based medicine, including precision medicine as an approach to clinical decision-making has the potential to advance personalized care and improve outcomes.
Still, hurdles such as bias and evaluation of ethically actionable risk factors can stand in the way.
Much of the challenge, though, centers around gathering and integrating patient genomic data so that it is actionable to providers.
This is the focus of a new precision medicine initiative at Frederick Health, where genomic data is being integrated into EHRs to support clinical decision-making and improve outcomes.
To dive deeper into these efforts, HealthITAnalytics sat down with Jackie Rice, chief information officer; Kristin Conley, DO, chief medical information officer and internal medicine physician; and Patricia Rice, clinical director, Precision Medicine & Genetics at Frederick Health.
Much of the challenge, though, centers around gathering and integrating patient genomic data so that it is actionable to providers.
This is the focus of a new precision medicine initiative at Frederick Health, where genomic data is being integrated into EHRs to support clinical decision-making and improve outcomes.

TECHNOLOGY CAN HELP BREAK DOWN GENOMIC DATA SILOS
Frederick Health is not a newcomer to precision medicine.
The health system’s Precision Medicine & Genetics program has existed for a few years. Its associated clinic leverages genomics to provide care for hereditary diseases, oncology, and precision nutrition.
Despite this, providers often struggled to find and access genomic data in a timely manner.
“When I was tasked to develop this program, I knew upfront that we would need a way to put this data front and center for our providers to be able to access because we knew that in the long run, we would want to have this information available for use in everyday practice,” the clinical director explained.
“So, we’re working toward that goal, and in order to do that, we really felt it necessary to integrate it into the EMR as discrete data for ordering and receiving results and so that it is front and center to our provider[s] so that they will begin using it every day and saving time as well.”
Using MEDITECH’s Expanse Genomics, providers can order genetic testing and view results in a specific tab that they navigate to within the patient’s record.
However, this is often not sufficient for use in primary care and behavioral health, the CIO noted.
To expand this technology and get the genomic data right in front of these providers, Frederick Health is currently working on adding attention-grabbing widgets to the EHR that indicate when a patient has had genetic testing related to different clinical concerns or specialties, such as oncology or pharmacogenetics.
By doing so, the health system aims to ensure that providers can easily access and take action using relevant patient genomic data to improve care and outcomes.
Previously, providers would have to sift through long PDFs or dozens of pages to find the information they needed, which cuts into the already limited amount of time they have with each patient.
Previously, providers would have to sift through long PDFs or dozens of pages to find the information they needed, which cuts into the already limited amount of time they have with each patient.
But, as with any new system that a health system implements, provider buy-in and support are crucial.
At Frederick Health, this initiative is being undertaken as a multidisciplinary effort and is steered by a committee that includes providers from disciplines across the health system.
This representation allows providers from each discipline to have at least one person advocating for them.
“I think the buy-in and the advocating among providers starts with an anecdote, a patient example, a good outcome, a bad outcome that was prevented by that genetic testing,” Conley stated.
“So that process starts, I think, [on] a very small scale.”
From there, the team focuses on further provider education to raise awareness of the initiative’s benefits, such as time and cost savings.

BUT DATA INTEGRATION IS KEY
Integrating genomic data into patient records in a way that’s actionable and useful to providers without causing additional burdens is also key to the success of an initiative like this.
But the process can be complex and laborious.
“Integrating discrete data from a genetic lab is very, very complicated,” the CIO explained.
“That’s why everybody’s not doing that. So, we wouldn’t have been able to do that without partnering with our [her vendor and MEDITECH].
We partnered with them and with the lab, and we have the interfacing. Not all the labs are ready to give us discrete data, so we have to evaluate what labs are we going to use, what kind of data do they have there, and how to map that in.”
Integrating genomic data into patient records in a way that’s actionable and useful to providers without causing additional burdens is also key to the success of an initiative like this.
But the process can be complex and laborious.
Using a third-party system has helped with this process, she noted.
Leveraging the system has meant that Frederick Health had support with figuring out how to map their genomic data into the patient record.
Further, in the future, other health systems may be able to use a similar strategy to leverage their data.
As part of the data integration process, health system leaders must consider what alerts are relevant for their providers.
Alerts that are relevant for a pharmacist may not be relevant for a cardiologist, which is why the widgets are customized, the CIO noted.
Thus, Frederick Health is experimenting with what alarms and alerts go to which specialty groups, she continued.
Providers in specialties with little knowledge of genomics and genetic testing receive only the alerts relevant to them within the EHR widget.
They also have access to a navigator who helps them determine what to do with that information, alongside the initiative-specific education they’re already receiving.
Providers in specialties with little knowledge of genomics and genetic testing receive only the alerts relevant to them within the EHR widget.
They also have access to a navigator who helps them determine what to do with that information, alongside the initiative-specific education they’re already receiving.
Further, patient education and counseling, in addition to buy-in and cooperation from payers and other stakeholders, are also key to the success and growth of any data integration process, especially one being used to bolster precision medicine.
The initiative is also doing significant work in pharmacogenomics.
“We have a PharmD that is seeing our patients who has the ability to order a pharmacogenomics test, and then that data comes back into the EMR, and it’s readily accessible to our providers when they’re prescribing,” the clinical director explained.
“So, our providers will receive alerts when they enter a medication that says [whether the patient is] a rapid metabolizer or a normal metabolizer of a medication.”
This is vital for patient safety and population health because genetics plays a critical role in drug response and potential interactions, she explained.
“Approximately five genes process about 75 percent of our medications,” Conley added.
“So, if we can map those genes out for patients and identify certain medications that would really be affected by metabolizing that drug, then I think we’re definitely in a better shape to dictate or help drive what treatment course we lay out for our patients.”
“Approximately five genes process about 75 percent of our medications,” Conley added.
Currently, Frederick Health is looking at antidepressant and psychotropic medications in this context.

MOVING FORWARD
The genomic data arm of Frederick Health’s precision medicine efforts had only been live for about 13 weeks at the time of the interview.
Consequently, the health system has yet to see results, and key performance indicators for an initiative in such a relatively new field can be hard to nail down.
However, the health system is confident that that initiative will succeed and is offering participation in the program to its employees first.
The health system is also working with MEDITECH to create new dashboards to support its precision medicine and genomics efforts and is looking into potential collaborations to further boost these efforts.
While Frederick currently has limited results related to this initiative, they hope to share them in the future.
Originally published at https://healthitanalytics.com
Names mentioned
Jackie Rice, chief information officer;
Kristin Conley, DO, chief medical information officer and internal medicine physician; and
Patricia Rice, clinical director, Precision Medicine & Genetics at
Frederick Health.