Older adults, like these nursing-home residents in Spain, are more vulnerable to infection and can respond poorly to vaccines. Credit: David Ramos/Getty
COVID-19 poses the greatest threat to older people, but vaccines often don’t work well in this group. Scientists hope drugs that rejuvenate the immune system will help.
Nature; NEWS FEATURE
Cassandra Willyard
14 October 2020
Unlike fine wine, the human body does not improve with age.
Hearing fades, skin sags, joints give out. Even the body’s immune system loses some of its vigour.
This phenomenon, known as immunosenescence, might explain why older age groups are so hard-hit by COVID-19.
And there is another troubling implication: vaccines, which incite the immune system to fight off invaders, often perform poorly in older people.
The best strategy for quelling the pandemic might fail in exactly the group that needs it most.
Scientists have known for decades that ageing immune systems can leave the body prone to infection and weaken their response to vaccines.
In June, the US Food and Drug Administration announced that a COVID-19 vaccine would have to protect at least half the vaccinated individuals to be considered effective, but protection in older adults might not even meet that bar.
“No vaccine is going to be as effective in the elderly as it is in young people,” says Matt Kaeberlein, a gerontologist at the University of Washington in Seattle. “That’s an almost certainty.”
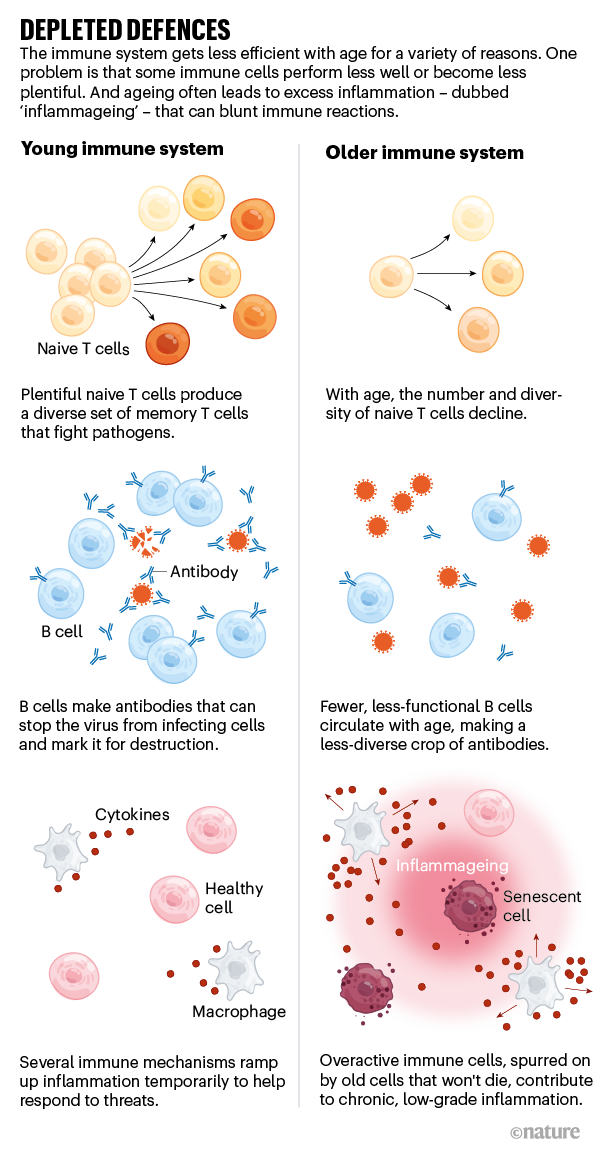
The human immune system is mind-bendingly complex, and ageing affects nearly every component.
Some types of immune cell become depleted: for example, older adults have fewer naive T cells that respond to new invaders, and fewer B cells, which produce antibodies that latch on to invading pathogens and target them for destruction. Older people also tend to experience chronic, low-grade inflammation, a phenomenon known as inflammageing (see ‘Depleted defences’). Although some inflammation is a key part of a healthy immune response, this constant buzz of internal activation makes the immune system less responsive to external insults. “This overarching, chronic inflammatory state is what’s driving much of the immune dysfunction that we see,” says Kaeberlein. The upshot is a poorer reaction to infections and a dulled response to vaccines, which work by priming the immune system to fight off a pathogen without actually causing disease.
With about 50 COVID-19 vaccine candidates currently being tested in humans, researchers say it’s not yet clear how they will fare in older adults.
In its phase I study of 40 people aged 56 and over, Moderna in Cambridge, Massachusetts, reported that its candidate mRNA-1273 elicited similar antibody levels as those elicited in a younger age group. The Chinese biotech Sinovac in Beijing, which trialled its CoronaVac candidate in a phase I/II study that included 421 adults between 60 and 89 years of age, announced in a press release on 9 September that it seems to work as well in older adults as it does in younger ones. However, a phase I study by international pharma company Pfizer and BioNTech in Mainz, Germany, showed that their vaccine BNT162b2 provokes an immune response that is about half as strong in older adults as it is in younger ones. The older adults still produced more antibodies in response to the vaccine than people of a similar age who had had COVID-19, but it’s not known how these levels translate into protection from the virus.
Most COVID-19 vaccine trials include at least some older adults.
But a recent analysis of 18 such trials found that the risk of exclusion is high. More than half had age cut-offs and many were at risk of excluding older participants for other reasons, including underlying conditions.
If COVID-19 vaccines perform less well in older adults, researchers might be able to find ways to tweak the shot itself to elicit a stronger response. Some influenza vaccines, for instance, include immune-boosting ingredients or higher doses of the viral antigen. But some scientists say there is a better option. They are developing and testing drugs that could improve how older adults respond to vaccines and might also help them fight viruses more effectively in the first place. Rather than working with the limitations of the ageing immune system, they are planning to rejuvenate it.
Forever young
Many researchers have grown old trying to pinpoint ways to reverse the ageing process. In the past decade, however, they have made serious progress in identifying particular molecular targets that might help in this quest.
One promising class of anti-ageing drug acts on pathways involved in cell growth.
These drugs inhibit a protein known as mTOR. In the laboratory, inhibiting mTOR lengthens lifespan in animals from fruit flies to mice. “mTOR is one of probably multiple biologic mechanisms that contribute to why we age and why our organ systems start to decline,” says Joan Mannick, co-founder and chief medical officer of resTORbio, a biotech company based in Boston, Massachusetts, that aims to develop anti-ageing therapies.
In a study published in 2018 and carried out when Mannick was at the Novartis Research Institutes in Cambridge, Massachusetts, she and her colleagues tried damping down mTOR in elderly adults to see if this could improve immune function and lower infection rates.
The 264 participants received a low-dose mTOR inhibitor or a placebo for six weeks. Those who received the drug had fewer infections in the year after the study and an improved response to the flu vaccine. On the basis of her work on mTOR inhibition, Mannick, by then at resTORbio, launched a phase III trial in 2019 to see if a similar mTOR inhibitor called RTB101 could stave off respiratory illnesses in older adults.
That trial failed to show the desired effect, perhaps because infections were monitored by self-report of symptoms rather than requiring a lab test to confirm infection, as in the earlier trial.
That created “a lot more noise”, says Ilaria Bellantuono, co-director of the Healthy Lifespan Institute at the University of Sheffield, UK, who was not involved in the trial. “A much bigger group would have been required to see a difference.”
Still, the data from this and an earlier trial suggested that participants who received the mTOR inhibitor had fewer severe infections from circulating coronaviruses and recovered faster from them than the placebo group.
The trials pre-date the emergence of SARS-CoV-2, but they suggest that RTB101 could lessen the severity of infection. resTORbio is now testing that idea in 550 nursing-home residents aged 65 and over.
RTB101 is similar to an already approved mTOR inhibitor, the immune-suppressing drug rapamycin.
At least four other groups are testing rapamycin in small numbers of infected individuals as a possible COVID-19 therapy; one group is trialling the drug exclusively in adults aged 60 or older.
The type 2 diabetes drug metformin also dampens down mTOR’s activity, albeit indirectly.
Some studies suggest that people who take metformin are less likely to be hospitalized or die if they contract COVID-19. A small retrospective study in China found that the mortality among hospitalized individuals with COVID-19 taking metformin was 2.9% compared with 12.3% in people who didn’t take the drug. Researchers at the University of Minnesota in Minneapolis analysed data on hospitalized individuals with COVID-19 who had an average age of 75, some of whom were already taking metformin for obesity or diabetes. They found a significant reduction in mortality among women taking metformin, but not among men.
Carolyn Bramante, an obesity researcher who led the University of Minnesota study, points out that diseases such as diabetes and obesity lead to some of the same immune deficits as occur in older age.
She and her colleagues plan to launch a trial of 1,500 people aged 30 and over to determine whether metformin could help stave off SARS-CoV-2 infection or prevent the worst outcomes in people already infected.
Meanwhile, Jenna Bartley, who studies ageing at the University of Connecticut in Storrs, is assessing whether metformin can boost responses to flu vaccine in a small trial of older adults.
The idea, based on her work in mice, is that metformin can improve the energy metabolism of the T cells of the immune system, making them better at detecting new threats. Bartley has finished collecting data, but because her lab was shut down owing to COVID-19, she won’t have the results analysed for a few more weeks.
If metformin works against COVID-19, researchers will still have to tease out why. Kaeberlein points out that no one is quite sure how metformin works because it has so many targets. “It’s about the dirtiest of dirty drugs out there,” he says. It was originally used as an anti-influenza drug; Bramante says it helps tamp down inflammation. Aside from the mechanistic unknowns, the advantage is that metformin has been used for decades and is generally safe. Children can take it, as can pregnant women. “Metformin is a medication that you actually could give prophylactically for 12 months without having to do any follow-up,” Bramante says, “and it costs less than US$4 a month.”
Soothing balm
mTOR is a classic anti-ageing target, but it’s far from the only one.
In fact, many anti-ageing pathways seem to be linked, says James Kirkland, who studies cellular ageing and disease at the Mayo Clinic in Rochester, Minnesota. “That is, if you target one, you tend to affect all the rest,” he says. Many of the immune changes that come with ageing lead to the same result: inflammation. So researchers are looking at drugs that will calm this symptom.
Arne Akbar, an immunologist at University College London, has shown that the anti-inflammatory drug losmapimod, which is being developed as a therapy for muscular dystrophy, might help boost immunity.
In a 2018 study, the researchers injected chickenpox virus into the skin of elderly adults. Although these people had already been exposed to chickenpox, their immune response was lacklustre, hampered by excess inflammation. When the team gave the study participants losmapimod, it ratcheted down inflammation by about 70% and improved their immune responses.
In June, the company currently developing losmapimod — Fulcrum Therapeutics in Cambridge, Massachusetts — launched a 400-person phase III study to investigate whether the drug could prevent death and respiratory failure in older people hospitalized with COVID-19.
Another class of drug, called senolytics, helps to purge the body of cells that have stopped dividing but won’t die.
These senescent cells are typically cleared by the immune system, but as the body ages, they begin to accumulate, ramping up inflammation. In August, Kirkland and a team at the Mayo Clinic launched a 70-person trial to test whether a senolytic called fisetin, which is found in strawberries and sold as a health supplement, can curb progression of COVID-19 in adults aged 60 or older. They also plan to test whether fisetin can prevent COVID-19 infection in nursing-home residents.
“Senescence is really a key factor in ageing,” says Eric Verdin, president and chief executive of the Buck Institute for Research on Aging in Novato, California, who is not involved in the fisetin research.
No senolytics have currently been approved for clinical treatment, however. “This is one area that has been much less studied,” he says.
Kaeberlein says it’s likely that most companies will pursue anti-ageing drugs as therapies before they test them as prophylactics.
“It’s much easier to get a therapy approved in people who are already sick,” he says. He thinks that mTOR inhibitors hold the most promise. “If I had the power to go back to the beginning of this whole COVID pandemic and try one thing, I’d pick mTOR inhibitors — rapamycin specifically,” he says. According to his back-of-the-envelope calculations, if rapamycin works in the same way in people as it does in mice, it could reduce COVID-19 mortality by 90%.
Kirkland says he can envisage giving one of these anti-ageing drugs as a primer before vaccination.
“We have to figure out ways to target fundamental ageing mechanisms at around the time that we’re vaccinating people,” he says, “but we have to find ways of doing this that are safe and effective.”
Added ingredients
If tweaking the immune system proves too challenging, there might be ways to juice up the vaccine itself.
For flu, there are two vaccines aimed specifically at people over 65, which help worn immune systems to stage a response. One, Fluzone High-Dose, contains four times the standard amount of flu virus antigens, and the other, Fluad, relies on an immune-boosting molecule called an adjuvant.
A team led by vaccinologist Ofer Levy at Boston Children’s Hospital in Massachusetts is working on a COVID-19 vaccine specifically for older adults, using an in-vitro screening system to identify the best adjuvants.
“Vaccines were typically developed as one-size-fits-all,” he says. But a lot of features — age, sex, and even the season — affect vaccine responses, Levy says. The best combinations of adjuvant and vaccine they find will be tested in mice and then in humans.
But, in general, developing medications to improve immune function seems like a much smarter strategy than creating vaccines specifically for elderly people, says Claire Chougnet, an immunologist at Cincinnati Children’s Hospital Medical Center in Ohio, who is studying inflammation in aged mice.
Vaccine development is costly and time-intensive. “In the case of an emerging virus, when you want a quick response, that makes things even more complicated if you have to do two types of vaccine,” she says. Plus, individual vaccines target specific pathogens, but an immune-boosting medication could be used with any vaccine. “That could work for flu, that could work for COVID-19. That would work for COVID-25,” she says. The approach is “extremely versatile”.
Verdin agrees that supporting the older immune system should be a priority. “I think the net result of all this will be renewed interest in understanding the defect in the immune response in the elderly.” That has implications not only for the coronavirus, but also for a host of other diseases, including other viral infections and even cancer. “COVID-19 has brought to the front something that a lot of people have ignored.”
Originally published at https://www.nature.com.
PDF version:
chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/viewer.html?pdfurl=https%3A%2F%2Fmedia.nature.com%2Foriginal%2Fmagazine-assets%2Fd41586-020-02856-7%2Fd41586-020-02856-7.pdf&chunk=true