the health strategist
institute for strategic health transformation
& digital technology
Joaquim Cardoso MSc.
Chief Research and Strategy Officer (CRSO),
Chief Editor and Senior Advisor
October 23, 2023
One page summary
What is the message?
Costa Rica’s remarkable success in managing the COVID-19 pandemic serves as a global exemplar of effective public health and crisis preparedness.
Its experience underscores the importance of a strong healthcare infrastructure and a robust public health system in managing a pandemic, offering valuable lessons for countries like the United States.

What are the key points?
Costa Rica’s Pandemic Success:
Despite fewer resources and more challenges, Costa Rica outperformed richer nations, including the United States, in controlling COVID-19. As of March 2023,
- Costa Rica’s death rate per 100,000 people was 182,
- significantly lower than the U.S. rate of 341.
Robust Healthcare Infrastructure:
Costa Rica began investing in public healthcare in the 1970s, focusing on primary healthcare, accessible hospitals, and public health programs. Primary care clinics, including the EBAIS model, were established in every community, ensuring a solid foundation for responding to pandemics.
Pandemic Preparedness:
Costa Rica’s commitment to public health and its proactive approach allowed the country to update its pandemic response plan in 2018, well before COVID-19’s arrival. This preparedness enabled Costa Rica to quickly set up testing, treatment, and healthcare infrastructure to manage the pandemic.
Investment in Health Workforce:
The Costa Rican Social Security Institution (Caja) invested heavily in healthcare workers, providing overtime pay, hiring additional personnel, and ensuring sufficient personal protective equipment.
Equitable Testing and Treatment:
All COVID-19 tests and treatments were accessible and free to all citizens, ensuring widespread testing and medical care.
Economic Relief:
The Bono Proteger program provided temporary subsidies to those affected by the crisis, offering economic support to mitigate the pandemic’s impact.
Vaccination Campaign:
Costa Rica’s community health workers played a crucial role in equitable vaccine distribution, resulting in 90% of the population receiving at least one COVID-19 vaccine dose.
Public Trust:
High levels of public trust in the healthcare system, fostered through effective communication, further solidified Costa Ricans’ confidence in the pandemic response.
Statistics and Examples
- Lower Death Rates: Costa Rica’s proactive approach led to a substantially lower COVID-19 death rate, with 182 deaths per 100,000 people, in contrast to the U.S.’s rate of 341 deaths per 100,000.
- Robust Infrastructure: By 2023, Costa Rica had 29 hospitals, 105 Health Area clinics, and over a thousand EBAIS clinics, allowing the rapid response to the pandemic.
- Economic Support: The Bono Proteger program provided temporary subsidies to approximately 700,000 people affected by the pandemic.
- Vaccination Success: Costa Rica’s community health workers ensured widespread and equitable vaccine distribution, with 90% of the population receiving at least one vaccine dose.
- Public Trust: Public trust in the healthcare system in Costa Rica remained high throughout the pandemic, supported by transparent communication.
Conclusion
Costa Rica’s success in managing the COVID-19 pandemic underscores the significance of a strong healthcare infrastructure, public health preparedness, and public trust in government.
Lessons from Costa Rica’s experience are essential for countries like the United States, emphasizing the need for investment in healthcare and pandemic preparedness to effectively manage future crises.
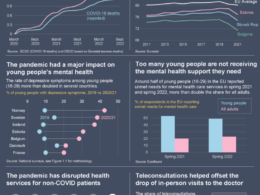
Infographic
DEEP DIVE

Costa Rica Managed to Limit COVID’s Spread. Here’s What the U.S. Should Know Before the Next Pandemic
The Commonwealth Fund
Munira Gunja
October 23, 2023
Costa Rica’s handling of the COVID-19 pandemic has been lauded as a global success story. As of March 2023, the Central American nation had an average of 182 deaths for every 100,000 people, substantially below the U.S. rate of 341 deaths per 100,000.
Costa Rica achieved this despite being a middle-income country with far fewer resources than richer nations like the United States, two difficult-to-control land borders, a critically important tourism industry, and a relatively high fiscal deficit that left little room to address the pandemic´s effects. The crucial difference was that Costa Rica’s government and vaunted public health care system started to prepare for the pandemic well ahead of the country’s first diagnosed COVID-19 case, allowing the nation to take decisive action once the virus appeared.
A Strong Health Care Infrastructure
Costa Rica began investing heavily in the public provision of health care in the 1970s, particularly emphasizing primary health care. This involved not only building robust and accessible hospitals but also investing in public health and primary health care programs, such as the Rural Health Program and Hospital sin Paredes (Hospital Without Walls) for at-home care.
By the 1990s, the Ministry of Health committed to building a high-quality primary care clinic for every community, even the most rural and remote. Responsibility for primary care was transferred to the Costa Rican Social Security Institution — known as the Caja — under a new model based on primary care teams (EBAIS). Each team comprises a doctor, nursing assistant, data specialist, and trained community health worker who makes house calls. In addition to providing curative and preventive health care, the EBAIS clinics and primary care network are responsible for collecting and analyzing epidemiologic data for new cases of HIV, influenza, malaria, dengue, and other diseases.
Partly because of this commitment to public health, Costa Rica had already updated its pandemic preparedness and response plan in 2018 in anticipation of possible swine and avian flu outbreaks. So by the time the country faced its first COVID-19 case, it had 29 hospitals, 105 Health Area clinics, and more than a thousand EBAIS clinics. With this infrastructure in place, the Caja was able to spring into action and limit the spread of the virus by:
- Investing in public health workers. The Caja invested hundreds of millions of dollars in its health care workforce — paying overtime, hiring additional personnel, and ensuring that all employees had adequate personal protective equipment.
- Conducting widespread testing and making treatments available. All COVID-19 tests and treatments were made accessible and offered free to all Costa Ricans.
- Providing economic relief. The Bono Proteger program was established to provide temporary subsidies to about 700,000 people affected by the crisis.
- Distributing vaccines equitably. Community health workers, already based in clinics throughout the country, visited and vaccinated all households in their jurisdictions. Today, 90 percent of the population has had at least one COVID-19 vaccine dose.
- Strengthening public trust. Costa Ricans have historically held the public health care system in high regard, reporting higher satisfaction with health services compared to the rest of Latin America. This high level of trust only deepened during the pandemic, as the president and the pandemic response team held daily public news conferences to deliver the most up-to-date information.
Will Things Be Different in the Next Pandemic?
With the United States far behind its neighbor to the south on several health measures, it will be challenging to replicate this success when the next pandemic strikes. While the Costa Rican government invested in a universal health system in which all citizens and permanent residents receive primary and preventive care, more than 8 percent of the population in the U.S. is uninsured. Lack of coverage, in addition to underinvestment in primary care, has resulted in a lower average life expectancy and higher rates of avoidable deaths in the U.S.

Inadequate preparations in the U.S. contributed to the lack of reliable information that was available to patients as well as physicians in the early days of the outbreak. In Costa Rica, community-based clinics were prepared to collect important epidemiological data at the local level, allowing the government to identify weaknesses, needs, and threats from the get-go and act accordingly. Mobilizing around these data was also comparatively easier in Costa Rica, where the pandemic was less politicized. In the United States, trust in the government was already low and plummeted further during the outbreak’s first year. Moreover, studies show that, at least in the early days, the federal government failed to follow evidence-based guidance for pandemic mitigation.
Costa Rica’s response to COVID-19 resulted in fewer deaths and higher vaccination rates. The U.S., on the other hand, continues to have one of the lowest COVID vaccination rates among industrialized nations. Costa Rica is seeing the benefits of its investment, with an overall healthier population compared to the U.S., where life expectancy is actually falling. Absent much greater investment in primary and preventive care and efforts to rebuild public trust in government, the United States will struggle in future outbreaks to duplicate Costa Rica’s achievements.
International Insights would like to thank Ambassador Roman Macaya and Dr. Madeline Pesec, MD, ScM for their review of, and contributions to, this article.
Originally published at https://www.linkedin.com/pulse