This is a republication of the paper “Radiology 2040”, with the title above.
the health transformation
institute for continuous health transformation
& digital health
Joaquim Cardoso MSc
Founder and Chief Researcher & Editor
December 23, 2022
Executive Summary
Overview
- The next 2 decades will bring astonishing changes to health care that are yet to be imagined.
- With the expected growth of AI, radiologists will need to offer added value beyond image interpretation.
- We have been tremendously innovative over time, and we must remain at the leading edge of innovation in both diagnostic imaging and image-guided therapy (eg, interventional radiology and radiotheranostics) to ensure that our technical advances and expertise continue to provide value in the years ahead.
- We are confident that with flexibility and agility, we will sustain our relevance to the full continuum of clinical care.
- However, we must continue to embrace changes that are best for patients, and decisions made with patients at their center will always serve us well.
- Radiologists will carry on shaping our own destiny just as we have for the past 100 years, since the first innovations of our specialty were set to print in Radiology.
BOX: What to Know to Ensure Radiology Is Thriving in 2040
- 1.Radiologists must add value to the health care continuum, especially given the rise of non–image-based precision diagnostics and minimally invasive interventional techniques
- 2. Radiologists whose activities are limited to image interpretation will not only become a commodity but, eventually, may become obsolete
- 3. The ability to offer therapy is essential for strengthening our clinical impact. We will need to cultivate interventional radiology and radiotheranostics extensively
- 4. Our workflows will be driven by disease focus rather than patient location
- 5. Radiologists need to maintain a strong presence within their institutions and continue to be recognized as key partners in patient care and research
- 6. Radiologists must recognize that artificial intelligence (AI) will enable us to function at a higher level, just as did the advent of digital imaging and electronic image display
- 7. Radiologists must remain the keepers of AI algorithms and oversee their use unequivocally
- 8. Non–image-based precision diagnostics (ie, “liquid biopsies”) will continue to rise, and radiology’s place in the value equation will need to evolve commensurately. Radiology will be responsible for phenotyping with imaging markers that are prognostic and predictive of treatment response on a large scale
- 9. Subspecialized training will remain extremely important, as radiologists’ clinical relevance can only be assured by radiologists being as knowledgeable as our subspecialized referring physicians
- 10. The carbon footprint of medical imaging will be at the forefront among environmental sustainability efforts
- 11. We must remain vigilant to do our part in bringing the power of medical imaging to the most underserved populations across the globe
- 12. Imaging technologies will become increasingly multiscale, multimodal, and multiomic
- 13. Due to advances in imaging, devices, techniques, and robotics, the array of minimally invasive interventions will continue to grow
- 14. Radiotheranostic growth will expand clinicians’ ability to first “see with precision” and then “treat with targeting.” Radiology and nuclear medicine will take leading roles in cancer diagnosis and treatment
ORIGINAL PUBLICATION

Radiology 2040
Radiology
James A. Brink, MD , Hedvig Hricak, MD, PhD
Dec 19 2022
Nothing is permanent except change
Heraclitus, around 500 BCE
Introduction
Historically, radiology has been a specialty of innovation.
Radiology has embraced new technologies and recognized their potential well before their clinical value has been widely accepted. We have been fearless in change and adaptation.
Radiology has embraced new technologies and recognized their potential well before their clinical value has been widely accepted. We have been fearless in change and adaptation.
Over the past 4 decades alone, we have repeatedly expanded and reshaped our field to accommodate revolutionary technological advances.
- We adopted cross-sectional anatomic imaging with CT and MRI, which required adaptation to much greater levels of detail in image interpretation.
- We introduced various forms of functional and molecular imaging, which required us to incorporate biology into our knowledge and image interpretation.
- We facilitated tremendous growth in applications of interventional radiology, incorporating clinics and clinicians with admitting privileges into many of our departments.
- Finally, most recently, we introduced marked advances in radiotheranostics, which combines targeted molecular imaging with radionuclide therapies.
Over the past 4 decades alone, we have repeatedly expanded and reshaped our field to accommodate revolutionary technological advances.
Today, we are in some ways the victims of our own success, as the demand for imaging, especially in oncology, keeps increasing.
We now face large volumes of examinations, exponential increases in the number of images generated by each examination, and the demand for 24/7 coverage.
In an era of widespread physician burnout, our specialty is among the most affected.
The present is not sustainable, and yet again, radiology is at a crossroads.
The next several decades are sure to bring seismic organizational and operational changes that will affect all medical specialties, including radiology.
- Artificial intelligence (AI) is emerging as an extremely powerful force in medicine and particularly in radiology-one that could help streamline our workflow and reduce our workload while also posing challenges to our relevance.
- Moreover, the pace of technological change is constantly accelerating.
- Many operational and technological developments that will affect radiology are being driven by external forces beyond our control.
Imaging will still play a critical role in diagnosis and minimally invasive intervention.
But, as radiologists, our focus must be laser-sharp on ways in which we can add value to the health care continuum, especially given the rise of non-image-based precision diagnostics and minimally invasive interventional techniques certain to occur in other specialties.
Radiologists whose activities are limited to image interpretation will not only become a commodity but, eventually, may become obsolete.
It is time to actively search out and demonstrate new means through which we can contribute beyond image interpretation.
If we approach this challenge in the right way, then the specialty will continue to prosper. But the specialty will have to change considerably.
Radiologists whose activities are limited to image interpretation will not only become a commodity but, eventually, may become obsolete.
At the most basic level, radiologists’ ability to remain clinically relevant will depend on our becoming and staying part of the clinical team.
The ability to offer therapy will also be essential for strengthening our clinical impact. Thus, we will need to cultivate interventional radiology and radiotheranostics extensively.
Furthermore, it will be critical for us to partner with other disciplines-in medicine, data science, engineering, and other areas-to perform clinically relevant research and carve out paths of innovation and expertise unique to our specialty.
Furthermore, it will be critical for us to partner with other disciplines-in medicine, data science, engineering, and other areas-to perform clinically relevant research and carve out paths of innovation and expertise unique to our specialty.
This editorial describes a variety of anticipated changes in the science and practice of radiology ( Table), some of which will appear almost inevitably and some of which the imaging community will only be able to achieve through vision and intense determination.
BOX: What to Know to Ensure Radiology Is Thriving in 2040
- 1.Radiologists must add value to the health care continuum, especially given the rise of non–image-based precision diagnostics and minimally invasive interventional techniques
- 2. Radiologists whose activities are limited to image interpretation will not only become a commodity but, eventually, may become obsolete
- 3. The ability to offer therapy is essential for strengthening our clinical impact. We will need to cultivate interventional radiology and radiotheranostics extensively
- 4. Our workflows will be driven by disease focus rather than patient location
- 5. Radiologists need to maintain a strong presence within their institutions and continue to be recognized as key partners in patient care and research
- 6. Radiologists must recognize that artificial intelligence (AI) will enable us to function at a higher level, just as did the advent of digital imaging and electronic image display
- 7. Radiologists must remain the keepers of AI algorithms and oversee their use unequivocally
- 8. Non–image-based precision diagnostics (ie, “liquid biopsies”) will continue to rise, and radiology’s place in the value equation will need to evolve commensurately. Radiology will be responsible for phenotyping with imaging markers that are prognostic and predictive of treatment response on a large scale
- 9. Subspecialized training will remain extremely important, as radiologists’ clinical relevance can only be assured by radiologists being as knowledgeable as our subspecialized referring physicians
- 10. The carbon footprint of medical imaging will be at the forefront among environmental sustainability efforts
- 11. We must remain vigilant to do our part in bringing the power of medical imaging to the most underserved populations across the globe
- 12. Imaging technologies will become increasingly multiscale, multimodal, and multiomic
- 13. Due to advances in imaging, devices, techniques, and robotics, the array of minimally invasive interventions will continue to grow
- 14. Radiotheranostic growth will expand clinicians’ ability to first “see with precision” and then “treat with targeting.” Radiology and nuclear medicine will take leading roles in cancer diagnosis and treatment
Radiology Workflow and Teleradiology
Increasingly, computation and data analytics will support imaging and other diagnostics, as well as connectedness and telehealth ( 1).
Current workflows are largely driven by patient location. Worklists are organized according to whether patients are inpatients, outpatients, or admitted to the emergency department.
But we will see the distinction between these three patient locations blurred as more and more medical care is delivered at home.
Home hospital programs are on the rise.
If inpatient care can be delivered at home, it is likely that we will see more urgent and acute care being delivered at home as well.
Thus, our workflows will need to be driven by disease focus rather than patient location.
Current workflows are largely driven by patient location. Worklists are organized according to whether patients are inpatients, outpatients, or admitted to the emergency department.
But we will see the distinction between these three patient locations blurred as more and more medical care is delivered at home.
Thus, our workflows will need to be driven by disease focus rather than patient location.
Just as other medical care will be delivered at home, imaging technologies will increasingly be brought to the patient for self-examination.
AI-powered autonomous or semiautonomous US using low-cost transducers driven by smartphone technology will enable patients to perform simple US data acquisition on their own, with images being reconstructed automatically ( 2).
In the future, other examinations may be performed locally, including with portable equipment for radiography, CT (motionless), and MRI (low field strength) ( 3, 4).
AI-powered autonomous or semiautonomous US using low-cost transducers driven by smartphone technology will enable patients to perform simple US data acquisition on their own, with images being reconstructed automatically ( 2).
In the future, other examinations may be performed locally, including with portable equipment for radiography, CT (motionless), and MRI (low field strength) ( 3, 4).
Home reading and teleradiology will continue to rise due to the growing demand for worker flexibility and the need for continuous coverage as well as outreach beyond urban centers.
However, radiologists of the future will need to think hard about how to balance remote and on-site readings for the benefit of patients, education, and cross-fertilization of knowledge.
It will be important for radiologists to maintain a strong presence within their health care institutions so that they continue to be recognized as key partners in patient care and research.
However, radiologists of the future will need to think hard about how to balance remote and on-site readings for the benefit of patients, education, and cross-fertilization of knowledge.
Artificial Intelligence
AI will not replace radiology, but it will profoundly affect our relevance and our workflow.
The greatest risk to our specialty is that other medical specialties, and potentially patients themselves, may leverage AI for independent image interpretation.
AI will not replace radiology, but it will profoundly affect our relevance and our workflow.
The greatest risk to our specialty is that other medical specialties, and potentially patients themselves, may leverage AI for independent image interpretation.
Given that referring physicians have clinical information at their fingertips, they will be able to put imaging findings in a clinically relevant context to a much greater degree than traditional radiologists.
Given that referring physicians have clinical information at their fingertips, they will be able to put imaging findings in a clinically relevant context to a much greater degree than traditional radiologists.
The globalization of consultative work combined with AI automation will increasingly threaten many white-collar disciplines.
These include medicine and law ( 5). Our pathology colleagues have seen evolution in practice.
For example, the Papanicolaou test no longer requires human interpretation routinely ( 6).
The globalization of consultative work combined with AI automation will increasingly threaten many white-collar disciplines. Our pathology colleagues have seen evolution in practice.
For example, the Papanicolaou test no longer requires human interpretation routinely ( 6).
Machine-based interpretations, potentially in distant locations, have become the norm.
The only exceptions are in unusual conditions that prevent automatic reading and require human intervention.
Certain radiology examinations will undergo a similar evolution. AI algorithms will provide comprehensive and autonomous interpretation.
Machine-based interpretations, potentially in distant locations, have become the norm. The only exceptions are in unusual conditions that prevent automatic reading and require human intervention.
Certain radiology examinations will undergo a similar evolution. AI algorithms will provide comprehensive and autonomous interpretation.
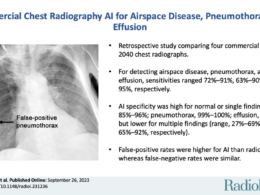
At present, most AI algorithms are narrowly focused, targeting a specific imaging feature or function.
Over the next several years, algorithm development will broaden substantially to include a comprehensive evaluation of all possible features that may be present in certain imaging examinations.
Over the next several years, algorithm development will broaden substantially to include a comprehensive evaluation of all possible features that may be present in certain imaging examinations.
Algorithm development will become increasingly federated, with the training of distributed algorithms on local data rather than moving data beyond secure firewalls.
This will increase the diversity of training data and minimize training bias, thereby promoting health equity and algorithm robustness.
Once an algorithm is trained, its quality will be maintained with continuous learning.
Temporal degradation owing to changes in local data environments will be minimal ( 7, 8).
Radiologists must remain the keepers of such algorithms and oversee their use unequivocally.
Algorithm development will become increasingly federated, with the training of distributed algorithms on local data rather than moving data beyond secure firewalls. This will increase the diversity of training data and minimize training bias, thereby promoting health equity and algorithm robustness.
Radiologists must remain the keepers of such algorithms and oversee their use unequivocally.
Just as AI will permeate all facets of daily living, it will affect all aspects of radiology practice.
These will range from examination triage and planning to lesion detection, characterization, and measurement ( 9).
AI will also enable greater assessment of disease likelihood and potential treatment outcomes by seamless integration of imaging findings with other clinical indicators. Radiologists’ role in this continuum is not assured.
We must see to it that we are adding value at every step.
AI will also enable greater assessment of disease likelihood and potential treatment outcomes by seamless integration of imaging findings with other clinical indicators. Radiologists’ role in this continuum is not assured.
We must see to it that we are adding value at every step.
The “lifelong learning” of AI algorithms, including their ability to adapt to improved or new technologies (eg, novel MRI pulse sequences, novel radiotracers) will influence the training of the next generation of radiologists.
The integration of AI into training will continuously evolve.
Radiologists will, at least in the short- and mid-term, still be required to supervise and, if necessary, overrule AI, thereby providing feedback and improving model performance.
Radiologists will, at least in the short- and mid-term, still be required to supervise and, if necessary, overrule AI, thereby providing feedback and improving model performance.
While training supported by AI will surely be a great learning opportunity, especially when visualization tools such as gradient-weighted class activation mapping, or Grad-CAM, are applied, we need to ensure that trainees acquire sufficient knowledge and do not unquestioningly trust the results produced by an algorithm ( 10).
For this, trainees need at least a basic understanding of AI algorithm design and training strategies to understand AI algorithms’ performance levels and limitations.
For this, trainees need at least a basic understanding of AI algorithm design and training strategies to understand AI algorithms’ performance levels and limitations.
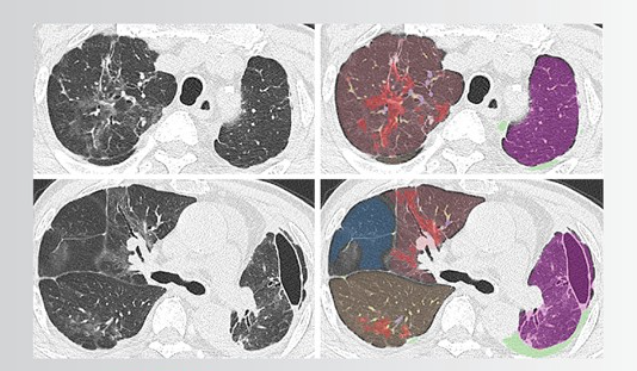
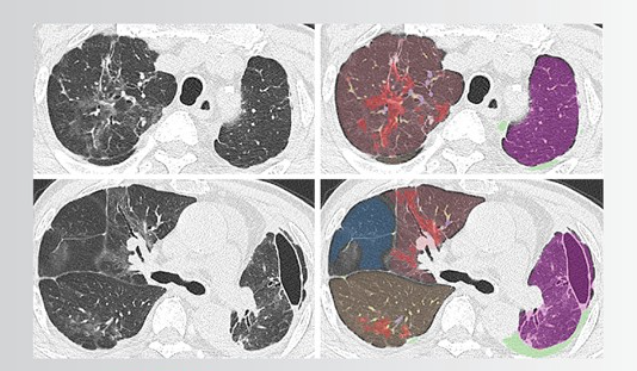
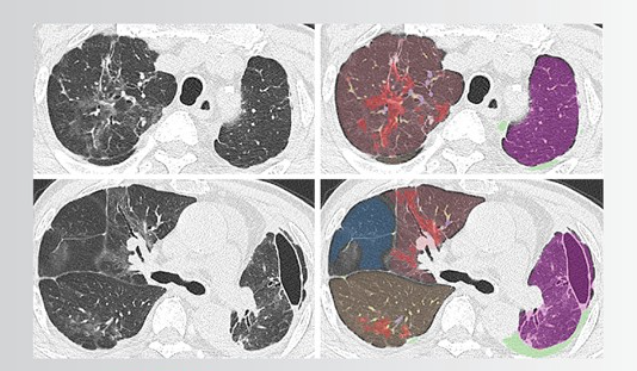
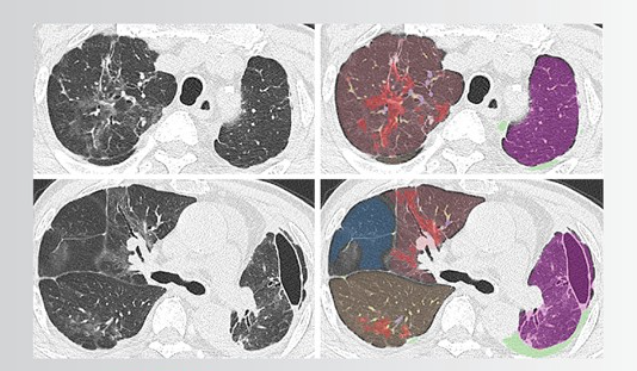
Over time, AI algorithms will enable the integration of radiomic features and metabolic or functional information with genomic and other phenotypic information for disease detection and characterization.
These capabilities will likely exceed what is achievable by humans alone ( 11).
As radiologists, we must welcome the assistance that AI will provide to our practices, recognizing that it will enable us to function at a higher level, just as did the advent of digital imaging and electronic image display.
To truly harness this AI-enhanced, integrated diagnostic approach, cross-training with other specialties such as pathology will be vital for the next generation of radiology trainees.
To truly harness this AI-enhanced, integrated diagnostic approach, cross-training with other specialties such as pathology will be vital for the next generation of radiology trainees.
This may be achieved by electives during residency, short-term fellowships, or at an even earlier point during medical school in the form of integrated MD-PhD programs.
Value-based Care
Non-image-based precision diagnostics (ie, “liquid biopsies”) will continue to rise, and radiology’s place in the value equation will need to evolve commensurately.
We must strive to be the primary purveyors of imaging examinations in every respect, from their most appropriate uses to timely, accurate, and precise reporting of the information they contain.
Imaging centers will evolve beyond diagnostic centers to treatment planning and prediction centers.
Radiology will be responsible for phenotyping with imaging markers that are prognostic and predictive of treatment response on a large scale.
The drive toward subspecialization for maximal value creation will continue.
But AI may enable radiologists to achieve highly subspecialized excellence (as so-called centaur radiologists-a combination of human plus computer) ( 12).
But AI may enable radiologists to achieve highly subspecialized excellence (as so-called centaur radiologists-a combination of human plus computer) ( 12).
While it is tempting to imagine that this scenario may enable AI-powered generalists to deliver the value typically seen with subspecialists, subspecialized training will remain extremely important, as radiologists’ clinical relevance can only be assured by radiologists being as knowledgeable as our subspecialized referring physicians.
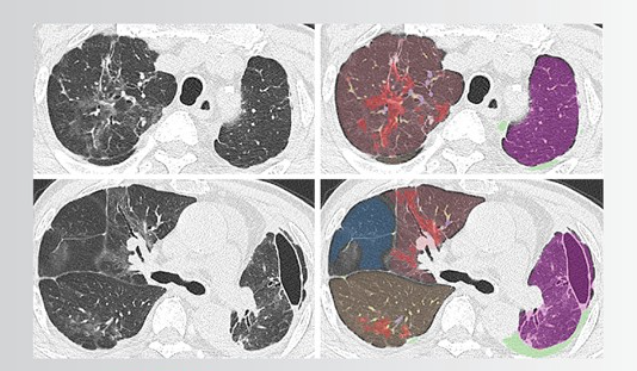
Imaging examinations will give rise to AI-derived three-dimensional data sets of imaging findings.
Radiologists will need to ensure the accuracy of salient findings.
More importantly, radiologists must ensure the integration of these findings with relevant clinical scenarios to produce meaningful and impactful diagnoses.
Imaging interpretations will be converted to lay language instantly and in a variety of media, including static and motion content with automatic, cinematically rendered images ( 13).
Patients and their providers will have instant and full access to their images and interpretations in real time, potentially for the application of individual or personal AI algorithms on features of interest.
Patients and their providers will have instant and full access to their images and interpretations in real time, potentially for the application of individual or personal AI algorithms on features of interest.
Recommended follow-up imaging or other diagnostic testing will be communicated, confirmed, and, if warranted, arranged automatically through robust care coordination systems ( 14).
These changes will further marginalize radiologists and threaten our relevance unless we integrate ourselves in the care continuum and add value beyond machine-generated interpretations and recommendations.
Recommended follow-up imaging or other diagnostic testing will be communicated, confirmed, and, if warranted, arranged automatically through robust care coordination systems ( 14).
These changes will further marginalize radiologists and threaten our relevance unless we integrate ourselves in the care continuum and add value beyond machine-generated interpretations and recommendations.
Environmental, Social, and Governance Concerns
The carbon footprint of medical imaging will be at the forefront of environmental sustainability efforts.
Thus, technical advances that substantially reduce our energy consumption will be embraced uniformly.
These include imaging devices and viewing equipment with reduced power requirements.
Renewable sources for consumables in diagnostic and interventional radiology will become mainstream.
Radiology’s role in ensuring that health care is delivered equitably across all demographic groups of our society is not assured.
Economic pressures will continue to favor the greatest care delivery to those who can most afford it.
We must remain vigilant to do our part in bringing the power of medical imaging to the most underserved populations across the globe ( 9).
Similarly, diversity among our leadership and within our governance structures is not assured.
We must continually strive for parity for women and members of other underrepresented groups, or the axiom “if you’re not at the table, you’re on the menu” will be as apt in 2040 as it is today.
Evolution of Imaging Technologies
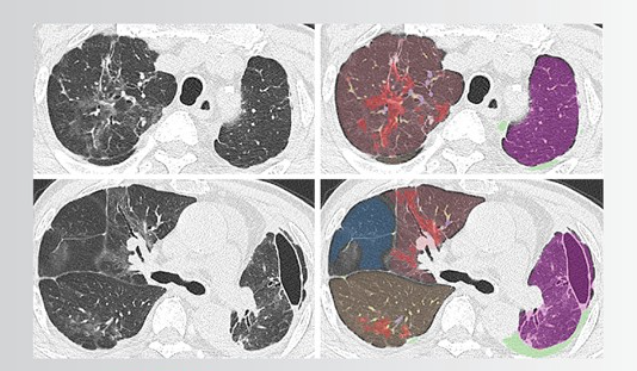
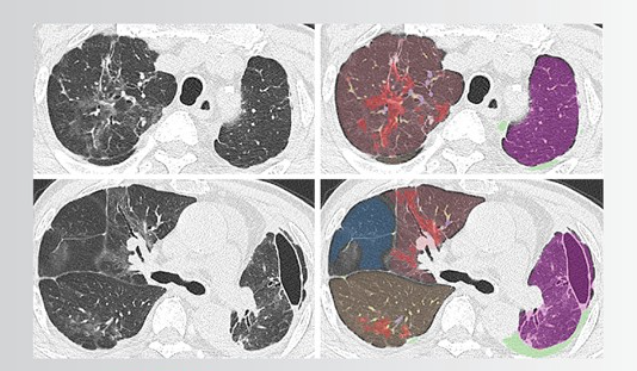
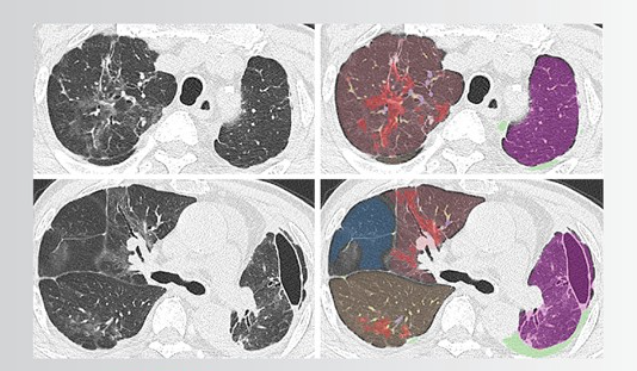
Imaging technologies will become increasingly multiscale, multimodal, and multiomic.
They will incorporate relevant metabolic, proteomic, and genomic information.
Imaging technologies will become increasingly multiscale, multimodal, and multiomic.
They will incorporate relevant metabolic, proteomic, and genomic information.
“Smart” contrast agents will increase exponentially, leveraging in vivo biochemistry, immunohistochemistry, reporter genes (genes that produce receptors that bind imaging probes), and nanoparticles.
Bioengineering will advance rapidly, showing explosive potential to alter the practice of medicine, with an outsized impact on medical imaging.
Phenotypic data generated by the physical interaction of an external energy source with biologic tissue will enter multiomic databases that cross multiple levels of biologic regulation, potentially bypassing the need for image formation (ie, fingerprinting).
Images will be reconstructed in select cases where human understanding is best achieved by visual means, such as for surgical or interventional radiology treatment planning.
Therapy: An Expanding Role of Radiology
1.Precision Imaging and Image-guided Intervention
Due to advances in imaging, devices, techniques, and robotics, the array of minimally invasive interventions will continue to grow ( 1).
Percutaneous endoscopic imaging will enable interventional radiologists to perform minimally invasive interventions in domains previously reserved for other specialties.
When combined with multispectral optical imaging, in vivo virtual histologic examination may be possible for certain pathologic conditions, potentially obviating the need for a needle biopsy ( 15).
Interventional procedures will become increasingly automated, powered by AI.
This will enable less-trained personnel to carry out some less complicated image-guided procedures, potentially at home and other locations beyond the purview of standard health care facilities ( 16).
AI-powered robotics may follow for more complex procedures.
2.Radiotheranostics
Molecular imaging will continue to expand through basic science research and clinical practice via the rapid rise in theranostics.
Theranostics combines diagnostic imaging with targeted therapy to noninvasively determine tumor phenotype and evaluate functional and molecular responses to therapy.
Radiotheranostics will continue to expand exponentially, combining molecular imaging-currently with PET and SPECT-with radionuclide therapy, leveraging small drugs, peptides, and antibodies to carry therapeutic radionuclides (alpha-, beta-, or auger-emitters).
Radiotheranostic growth will expand clinicians’ ability to first “see with precision” and then “treat with targeting.”
While oncologic radiotheranostics already includes numerous contemporary applications, it has enormous untapped potential for treating a huge range of cancers, given its capacity to be adapted to different targets and maximize tumor killing while minimizing side effects ( 17).
While oncologic radiotheranostics already includes numerous contemporary applications, it has enormous untapped potential for treating a huge range of cancers, given its capacity to be adapted to different targets and maximize tumor killing while minimizing side effects
Real-time feedback from imaging allows clinicians to improve patient selection for therapy, provide earlier and more precise treatment response assessment, and expedite drug development.
Whereas patients are typically selected for cancer therapies based on clinical (and secondarily histopathologic or molecular) parameters, pairing radiation therapy with a companion diagnostic (eg, technetium 99m, fluorine 18, or gallium 68) allows clinicians to visualize in vivo the expression of the therapeutic target, confirm the presence of the therapeutic agent, and visualize tumor burden.
In the field of oncology, drug development currently fails about 90% of the time.
Radionuclide therapies, however, provide insights regarding the biodistribution of both intended targets and radioligands that allow researchers to quickly halt, adapt, or accelerate their experiments.
In the field of oncology, drug development currently fails about 90% of the time.
Radionuclide therapies, however, provide insights regarding the biodistribution of both intended targets and radioligands that allow researchers to quickly halt, adapt, or accelerate their experiments.
This increases the success rates of these therapies over those of conventional cancer therapies.
The development and implementation of radiotheranostics will clearly represent a tremendous opportunity for radiology and nuclear medicine to take leading roles in cancer diagnosis and treatment.
Furthermore, while radionuclide probes for the selective and targeted diagnosis and treatment of specific cells hold immense promise for cancer, they also will have potential for application to other patient-specific diseases, including inflammatory and autoimmune conditions.
Realizing the full potential of radiotheranostics for advancing clinical care will require more extensive cross-training of radiologists, and likely other clinicians, in nuclear medicine ( 18).
Realizing the full potential of radiotheranostics for advancing clinical care will require more extensive cross-training of radiologists, and likely other clinicians, in nuclear medicine
Conclusion
The next 2 decades will bring astonishing changes to health care that are yet to be imagined.
With the expected growth of AI, radiologists will need to offer added value beyond image interpretation.
We have been tremendously innovative over time, and we must remain at the leading edge of innovation in both diagnostic imaging and image-guided therapy (eg, interventional radiology and radiotheranostics) to ensure that our technical advances and expertise continue to provide value in the years ahead.
We have been tremendously innovative over time, and we must remain at the leading edge of innovation in both diagnostic imaging and image-guided therapy (eg, interventional radiology and radiotheranostics) to ensure that our technical advances and expertise continue to provide value in the years ahead.
We are confident that with flexibility and agility, we will sustain our relevance to the full continuum of clinical care.
However, we must continue to embrace changes that are best for patients, and decisions made with patients at their center will always serve us well.
Radiologists will carry on shaping our own destiny just as we have for the past 100 years, since the first innovations of our specialty were set to print in Radiology.
Radiologists will carry on shaping our own destiny just as we have for the past 100 years, since the first innovations of our specialty were set to print in Radiology.
References
See the original publication
Originally published at https://pubs.rsna.org.
About the authors & affiliations
James A. Brink, MD
Hedvig Hricak, MD, PhD
From the Department of Radiology, Massachusetts General Hospital, Brigham and Women’s Hospital, Boston, Mass (J.A.B.);
and Department of Radiology,
Memorial Sloan Kettering Cancer Center, 1275 York Ave, Ste H-704, New York, NY 10065 (H.H.).
Acknowledgments
The authors thank Jason Lewis, PhD; Marius Mayerhoefer, MD, PhD; and Ralph Weissleder, MD, PhD, for their valuable input and Ada Muellner, MS, for editing the manuscript.