health and tech institute
research and strategy institute
for continuous health transformation
Joaquim Cardoso MSc.
Founder and Chief Researcher & Advisor
February 17, 2023
EXECUTIVE SUMMARY
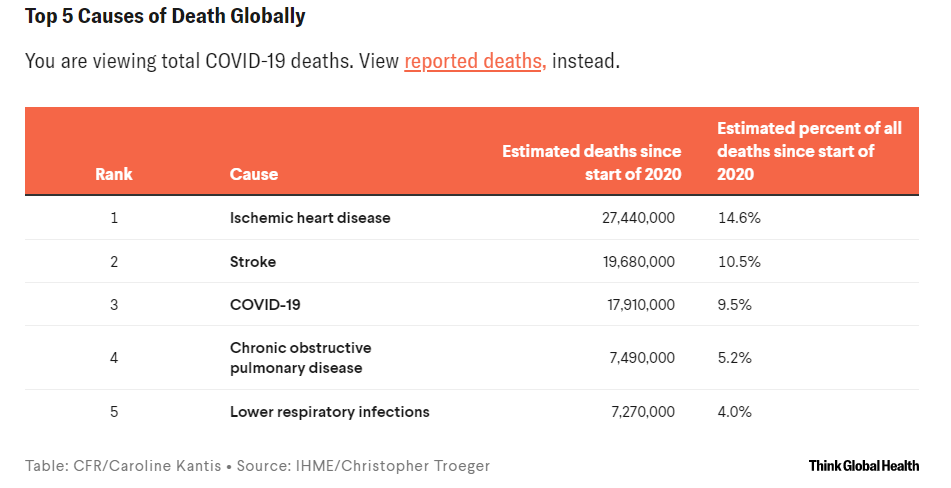
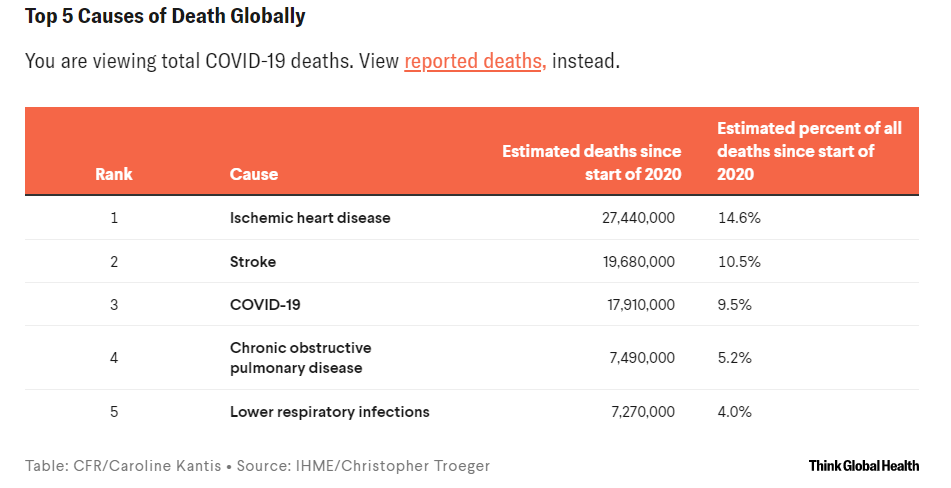
According to official statistics, COVID-19 was the fifth leading cause of death globally, responsible for nearly one in twenty deaths.
However, the real number of deaths is likely underestimated, with estimates suggesting the total number of deaths could be nearly 18 million worldwide, making it the third leading cause of death.
- More people in the United States died of COVID-19 than in any other country (1.1 million).
- According to official statistics, COVID-19 was the leading cause of death in Brazil, Mexico, and Peru.
- But after factoring in COVID-19 deaths that went uncounted, it became the leading cause of death in Italy and France.
- COVID-19 was the second leading cause of death in the region of the Americas and the third leading cause of death in the European region.
- COVID-19 disproportionately affects people over 70 years old and accounts for more deaths in countries with older populations and a greater prevalence of chronic health conditions.
- However, countries with strong infectious disease surveillance systems and effective public health measures, such as China, Taiwan, Thailand, and New Zealand, have been able to control the spread of COVID-19 and keep death counts low.
People all over the world are grief-stricken at the loss of friends, family members, and neighbors, and the disruption to their communities and livelihoods.
As individuals and societies, we should work to prevent COVID-19 from being a leading cause of death in the years to come.
INFOGRAPHIC
DEEP DIVE

Just How Do Deaths Due to COVID-19 Stack Up?
Despite a likely undercount in many places, COVID is among the leading causes of death in most countries
Think Global Health
Christopher Troeger
February 15, 2023
At the end of December 2019, the World Health Organization country office in China was notified of several cases of pneumonia of unknown etiology. These were the first cases of COVID-19.
In the three years since, COVID-19 has killed more than 7.3 million people worldwide, including more than one million people in the United States, 800,000 in Russia, 690,000 in Brazil, and 530,000 in India.
These tallies could substantially underestimate COVID-19’s true death toll.
In fact, some estimates suggest the total number of deaths could be more than two times as large as reported globally-nearly eighteen million deaths-and more than ten times greater than reported in some countries.
The scale of loss is staggering, but the huge numbers are difficult to understand without context.
It can be helpful to consider how COVID-19 ranks as a cause of death around the world, and the factors driving those trends.
Looking at official statistics alone, COVID-19 was the fifth leading cause of death globally, accounting for nearly one in twenty deaths worldwide since the beginning of 2020.
After accounting for unreported deaths, the total toll could be as high as the third leading cause of death, responsible for an estimated 17.9 million deaths, or one out of every ten deaths.
About half of people globally live to 70 before they die, so causes of death that tend to kill older adults including ischemic heart disease and stroke predominate the most common causes of death.
COVID-19 is similar in that it kills very few young children or adolescents but becomes sharply more dangerous with age, disproportionately killing people over 70 years old.
An analysis found that different age structures, or the fraction of the population is in different age groups, could explain almost half of the variation in the risk of mortality between countries.
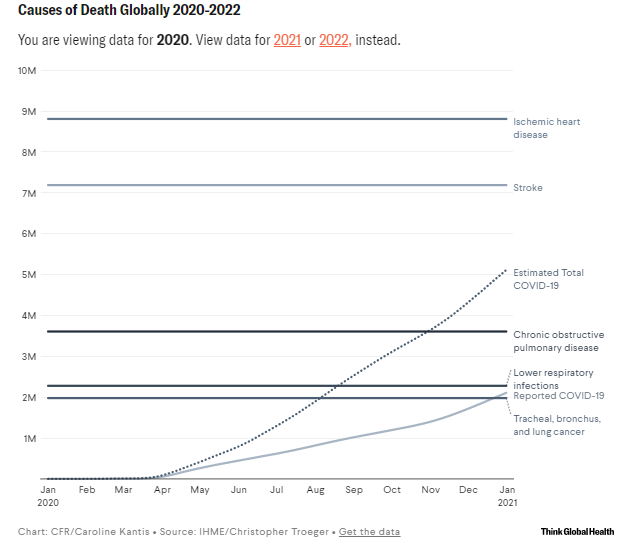
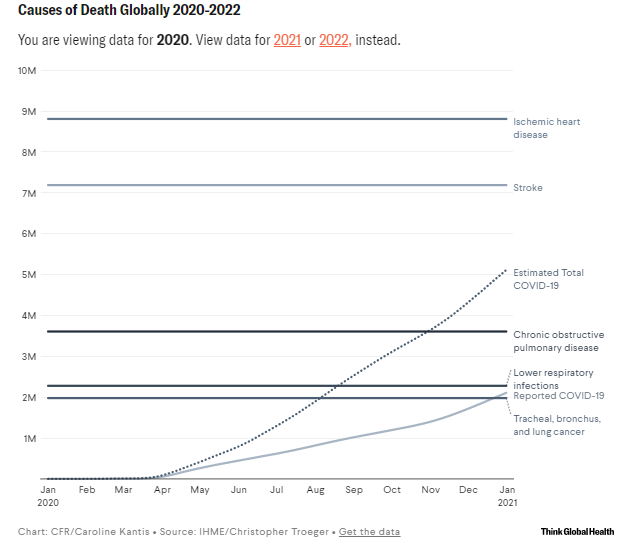
Despite improved treatment and the growing, albeit inequitable, availability of vaccines and therapeutics for COVID-19, 2021 was its deadliest year.
About 3.9 million COVID-19 deaths occurred in 2021, representing about half of all COVID-19 deaths from 2020–2022.
This is probably related to the emergence of the delta variant, which was much more likely to lead to fatal outcomes compared to the ancestral variant, and the omicron variant, which despite being less severe than the ancestral variant is more transmissible.
Despite the relaxing of mitigation measures and the expiration of some public health emergency orders, 2022 had the fewest annual deaths from COVID, about 1.3 million, likely due to widespread population immunity from vaccines, infection, or both.
One massive outlier in political and epidemiological experience during the first three years of the pandemic is China.
The country has made an abrupt shift in policy related to zero-COVID, relaxing its previously strict quarantining and testing guidelines that had, for most of the last three years, brought entire cities to a grinding halt.
There are major uncertainties in how this will manifest in 2023 and beyond, but a long-range forecasting model from IHME is predicting at least a million deaths in China.
There are major uncertainties in how this will manifest in 2023 and beyond, but a long-range forecasting model from IHME is predicting at least a million deaths in China.
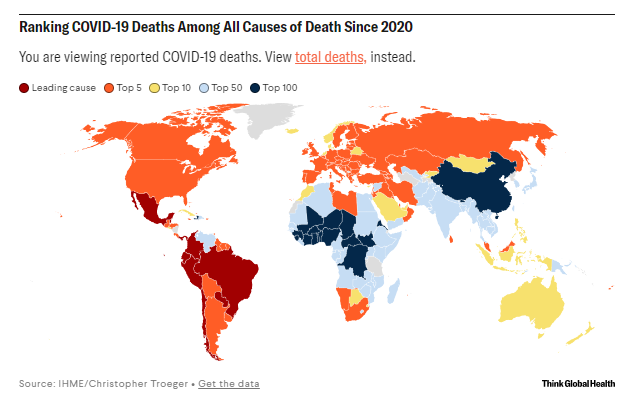
According to official statistics, COVID-19 was the leading cause of death in Brazil, Mexico, and Peru.
But after factoring in COVID-19 deaths that went uncounted, it became the leading cause of death in Italy and France.
COVID-19 was the second leading cause of death in the region of the Americas and the third leading cause of death in the European region.
People over 70, who are at elevated risk of COVID-19 mortality, make up a larger share of the population in higher-income countries.
Countries with older populations also tend to have a greater prevalence of chronic health conditions that increase with age such as obesity, high blood pressure, diabetes, chronic kidney disease, and respiratory illness, which likely contributed to higher rates of COVID-19 mortality.
In contrast, a handful of countries and territories like China, Taiwan, Thailand, and New Zealand acted quickly to control the spread of COVID-19, and kept their death counts low, at least in the first months and years of the pandemic.
This held true when accounting for deaths that could be missing from official statistics.
Countries in East Asia were well prepared for COVID-19 thanks to strong infectious disease surveillance systems they developed in response to recent respiratory disease outbreaks including influenza H1N1 and Severe Acute Respiratory Syndrome (SARS). When COVID-19 arrived, South Korea and Taiwan were quick to test and trace infections and embraced mask-wearing, due in part to a culture of mask use during influenza season.
Australia and New Zealand also acted quickly, enacting strict international and domestic travel restrictions and social distancing mandates, likely helping them sustain low levels of transmission.
COVID-19 has also been among the leading causes of death in many countries in Europe, North America, and Latin America.
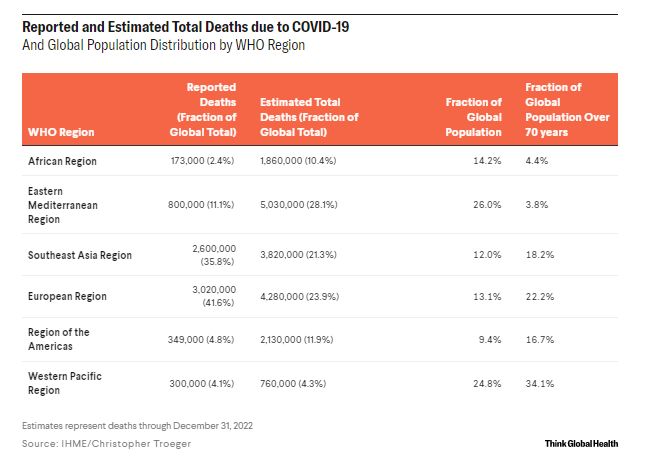
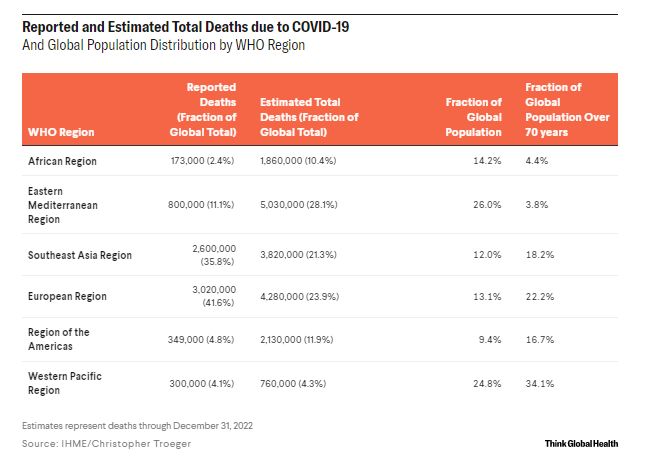
The Americas and Europe accounted for about 75 percent of reported COVID-19 deaths globally, even though they represent only about a quarter of the world’s population.
However, their share of estimated total COVID-19 deaths was about 45 percent, reflecting substantial burden of unreported mortality in the African region (five times more than reported), South East Asia region (about three times more than reported), and the Eastern Mediterranean region (about three times more than reported).
Importantly, the age pyramid, or the percentage of people who fall into each age group, differs across WHO regions.
Of the 483 million people worldwide over 70 years old, about one-third live in the Western Pacific region and another quarter live in the European region.
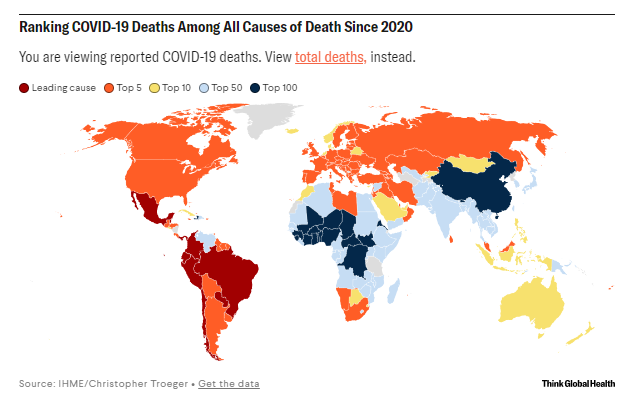
Based on reported data alone, COVID-19 has not been a leading cause of death in much of the African, South-East Asian, or Western Pacific Regions.
However, when considering underreporting and correcting for total COVID-19 deaths, COVID-19 is among the leading causes of death in many countries of sub-Saharan Africa and South Asia.
Countries in these regions tend to have a higher overall burden of infectious diseases compared to countries in Europe or North America.
One analysis suggests that undercounting of COVID-19 deaths contributes to these patterns. Although it is an issue worldwide, the fraction of missed COVID-19 deaths could be highest in South Asia and sub-Saharan Africa.

Why are COVID-19 deaths lower in some regions and locations?
Research suggests that a variety of contextual and population-health factors could explain some of the variation including the age patterns (about 50 percent), country wealth (measured as gross domestic product per capita, about 3 percent), and average body mass index (about 1 percent).
This leaves a substantial amount of variation unexplained.
Other factors that contribute include decisive and effective government responses, international coordination in response and diagnostic testing, income inequality, and lower rates of chronic diseases including obesity and diabetes.
Public trust in government and other people is associated with greater impact of policies meant to reduce mobility and in COVID-19 vaccine uptake. Further, trust in institutions like scientists and health authorities is associated with behaviors like mask wearing, handwashing, and belief in the importance of community action to respond to the pandemic.
More people in the United States died of COVID-19 than in any other country
More people in the United States died of COVID-19 than in any other country (1.1 million).
Although this is in part due to the large U.S. population, the country also has a high death rate due to COVID-19.
Incredibly, 114,000 more Americans died of COVID-19 in 2021 compared to 2020, despite the federal government purchasing over a billion doses of mRNA vaccine, enough to cover its population several times over.
More people in the United States died of COVID-19 than died of seasonal influenza in the last ten years (2010–2020) and COVID-19 is the deadliest disease in U.S. history, surpassing the 1918 influenza pandemic which killed an estimated 675,000 Americans.
When the causes of death are ranked in this article, it assumes that estimates for non-COVID-19 causes would remain the same in the absence of COVID-19. This may not be true.
During the pandemic, researchers have noticed decreases in injuries and road traffic deaths due to lower mobility; decreases in routine health-care utilization, potentially affecting mortality due to chronic but treatable diseases; decreases in other respiratory diseases like pneumonia; and other changes in disease burden.
Another consideration could be that in locations with complete or near complete vital registration systems, like the United States, deaths originally determined as a non-COVID-19 cause were in fact caused by COVID-19, potentially changing the ranking of causes of death presented in this post.

The future of COVID-19 is impossible to predict.
Trends in China could dominate the narrative for 2023.
It will likely be among the leading infectious causes of death globally, probably equaling tuberculosis and HIV which each cause about a million deaths per year.
Although it could continue to be a leading cause of death in 2023 and beyond, there are things that can help mitigate its spread.
Governments should use the opportunity to strengthen surveillance systems including the availability of COVID-19 tests, data analytic capacity, and reporting completeness and timeliness.
Investing in community-level public health infrastructure and rebuilding public trust is needed in many places worldwide.
It remains urgent to expand the availability and uptake of vaccines, particularly bivalent formulations designed around the ancestral and omicron variants, and in highly efficacious antiviral therapies in all settings and ensure that all people have the opportunity to receive them, no matter where they live.
People all over the world are grief-stricken at the loss of friends, family members, and neighbors, and the disruption to their communities and livelihoods.
As individuals and societies, we should work to prevent COVID-19 from being a leading cause of death in the years to come.
As individuals and societies, we should work to prevent COVID-19 from being a leading cause of death in the years to come.

ACKNOWLEDGEMENTS: The author would like to thank Katherine Leach-Kemon for her support on the article and to thank Catherine Bisignano, Katie Welgan, Emma Castro, Erin Frame, Rebecca Sirull, and Professors Robert Reiner and Emmanuela Gakidou for their feedback and fact-checking.
EDITOR’S NOTE: The author is employed by the University of Washington’s Institute for Health Metrics and Evaluation (IHME), which produced the COVID-19 forecasts described in this article. IHME collaborates with the Council on Foreign Relations on Think Global Health. All statements and views expressed in this article are solely those of the individual author and are not necessarily shared by their institution.
Christopher Troeger is a doctoral student at the University of Washington and a pre-doctoral research assistant at the University of Washington’s Institute for Health Metrics and Evaluation (IHME).
Originally published at https://www.thinkglobalhealth.org.












