health transformation institute
the most comprehensive knowledge portal for health transformation
Joaquim Cardoso MSc*
Founder, CEO and CSO
November 24, 2022
MSc* from London Business School — MIT Sloan Masters Program
Executive Summary:
What is the scope of the paper?
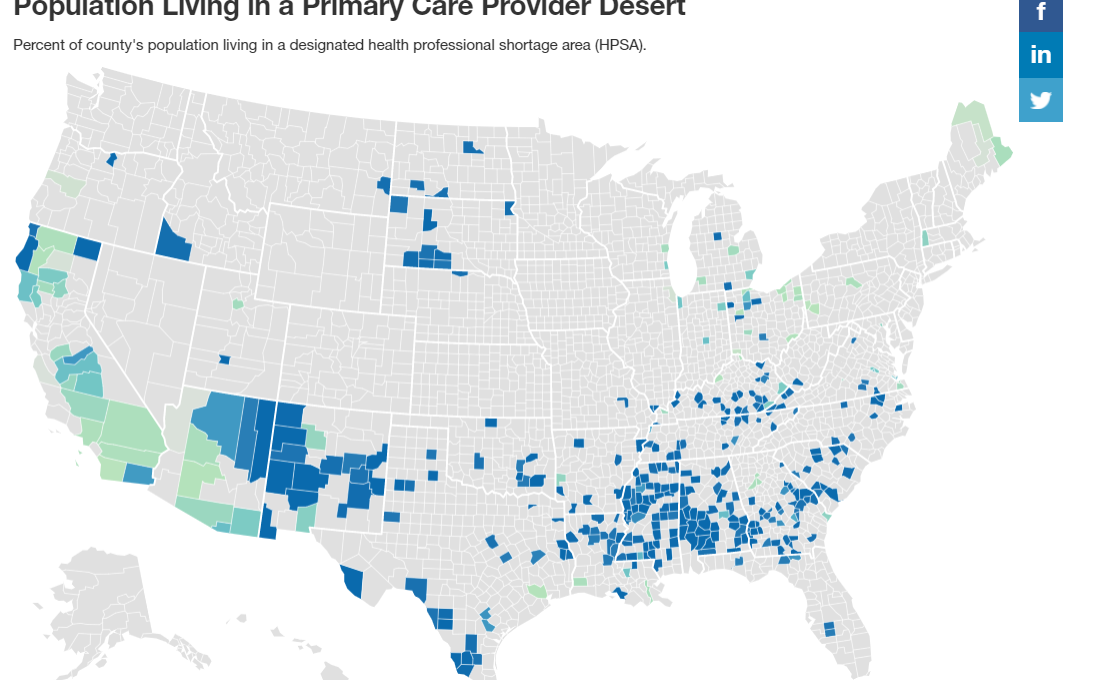
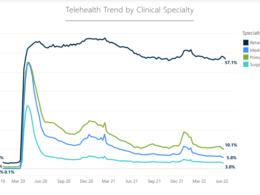
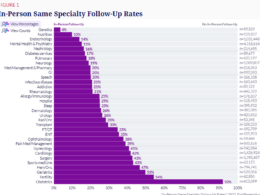
- Telemedicine use has accelerated across the US and has the potential to expand health care access to vulnerable populations and areas with limited health care services (health care deserts)
- Reliable internet access remains challenging within many communities, and whether telemedicine will mitigate or widen health disparities is unclear.
- To assess internet service availability and population demographics in health care deserts, the authors analyzed 2015 to 2019 American Community Survey data, linking them to national, state, and county-level metrics of health care access.
What are the findings?
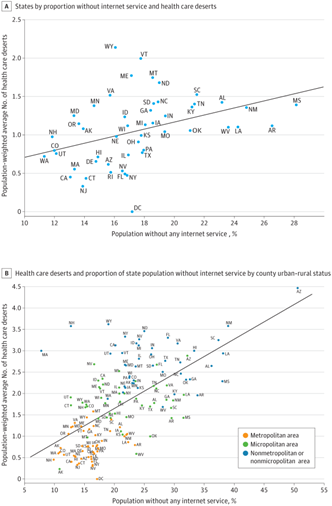
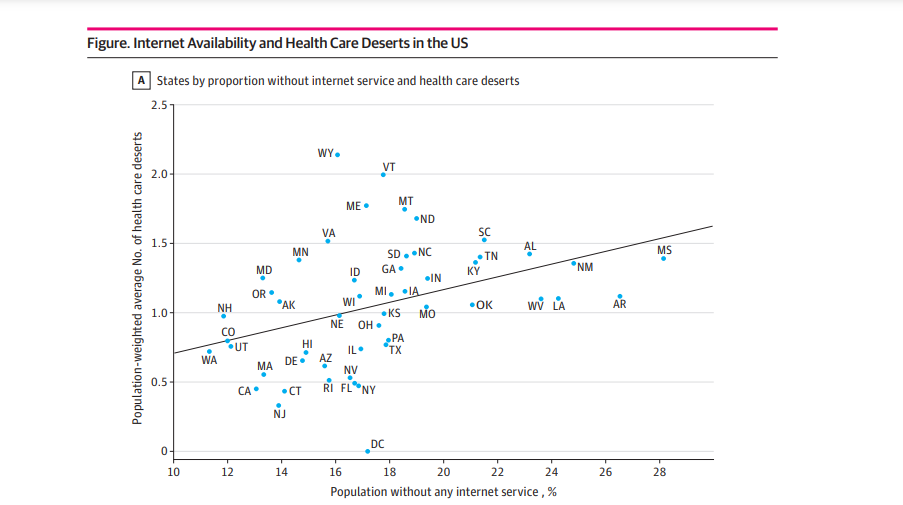
- Among 3140 counties (99.9% of all US counties), health care access and internet service availability were correlated (slope, 4.6 [P = .005]; intercept, 0.3 [P = .36]) (Figure, A).
- Mississippi, Arkansas, Louisiana, New Mexico, West Virginia, and Alabama had the largest percentage of households without internet service (>23%) and the highest fitted population-weighted mean number of health care deserts.
- Washington, New Hampshire, Colorado, Utah, California, and Maryland had the lowest number of households without internet service and the lowest fitted number of health care deserts.
- Rural counties were more likely to have more health deserts and less internet service availability (slope, 8.1 [P < .001]; intercept, 0.0 [P = .91]) (Figure, B).
What are the implications?
- These findings suggest that telemedicine expansion may have low effectiveness in counties where telemedicine is most needed but health care access is already limited.
What are the recommendations?
- Expanding telemedicine without improving internet access and digital literacy, along with mitigating clinician shortages, could contribute to rural-urban health disparities in the US.
- Study limitations include lack of digital literacy data, which could exacerbate urban-rural disparities.
- Public efforts to create community broadband networks and expand low-cost internet service in areas with poor health care access, while providing flexibility for other forms of communication in the short term as infrastructure develops, are critical to equitable access given the uptake and promise of telehealth.
Infographic:
ORIGINAL PUBLICATION (jama)
Geospatial Analysis of Access to Health Care and Internet Services in the US
JAMA Network
Eméfah C. Loccoh, MD1; Amanda Nguyen, PhD2; Gaeun Kim, MS2; Haider J. Warraich, MD1,3
November 23, 2022
Introduction
Telemedicine use has accelerated across the US and has the potential to expand health care access to vulnerable populations and areas with limited health care services (health care deserts).1
Reliable internet access remains challenging within many communities, and whether telemedicine will mitigate or widen health disparities is unclear.
To assess internet service availability and population demographics in health care deserts, we analyzed 2015 to 2019 American Community Survey data, linking them to national, state, and county-level metrics of health care access.
We hypothesized that internet access was poor in areas with limited access to traditional health care resources.
Methods
This cross-sectional study was exempt from review and the informed consent requirement per the Common Rule because the data used were deidentified. We followed the STROBE reporting guideline.
Health care deserts were identified by poor access to domains of pharmacies, hospitals, hospital beds, trauma centers, primary care physicians, and low-cost health centers at the census tract level, with an aggregate score of 0 to 6 (higher scores indicated more deserts across the domains)2 (eMethods in the Supplement).
Data sources were dataQ and GoodRx databases for 60 249 pharmacies; Health Resources & Services Administration (HRSA) for primary care health professional shortage areas; and Homeland Infrastructure Foundation-Level Data, the Indian Health Service, and HRSA for 7513 hospitals, 2020 trauma centers, and 11 643 community health centers.
State populations were grouped by metropolitan status as defined by the US Census Bureau: metropolitan (urban area with a population of ≥50 000), micropolitan (urban area with a population of ≥10 000), and nonmetropolitan or nonmicropolitan (rural area with a population of <10 000).
The proportion of populations with any internet access and the expected number of health care deserts, representing the population-weighted mean number of health care deserts in a region, were calculated and mapped for each metropolitan status in each state. Population race and ethnicity were obtained from data sources.
All analyses were performed using Python 3.10 (Python). Two-sided P < .05 indicated significance.
Results
Among 3140 counties (99.9% of all US counties), health care access and internet service availability were correlated (slope, 4.6 [P = .005]; intercept, 0.3 [P = .36]) (Figure, A).
Mississippi, Arkansas, Louisiana, New Mexico, West Virginia, and Alabama had the largest percentage of households without internet service (>23%) and the highest fitted population-weighted mean number of health care deserts.
Washington, New Hampshire, Colorado, Utah, California, and Maryland had the lowest number of households without internet service and the lowest fitted number of health care deserts.
Rural counties were more likely to have more health deserts and less internet service availability (slope, 8.1 [P < .001]; intercept, 0.0 [P = .91]) (Figure, B).
Rural counties were more likely to have more health deserts and less internet service availability
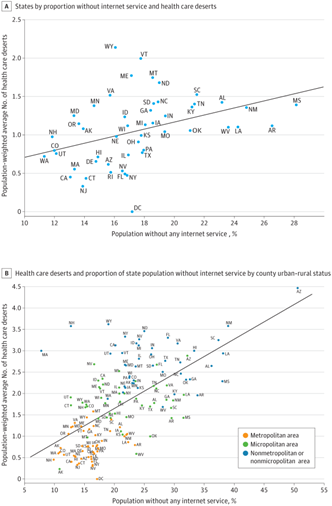
Counties with above-median numbers of health care deserts and proportions of population without internet access were more likely to be rural (78% vs 26%; P < .001), have lower income ($47 333 vs $66 139; P < .001), and be sparsely populated (20 586 vs 325 206; P < .001) compared with counties with below-median numbers (Table).
The correlation between expected number of health care deserts and county-level characteristics was the rural population percentage (Pearson r2 = 0.67).
Discussion
These findings suggest that telemedicine expansion may have low effectiveness in counties where telemedicine is most needed but health care access is already limited.
Expanding telemedicine without improving internet access and digital literacy, along with mitigating clinician shortages, could contribute to rural-urban health disparities in the US.3
Study limitations include lack of digital literacy data, which could exacerbate urban-rural disparities.
Although not meant to show causal association, this study found significant co-occurrence of poor internet and health care access across 6 domains.
Although not meant to show causal association, this study found significant co-occurrence of poor internet and health care access across 6 domains.
Public efforts to create community broadband networks and expand low-cost internet service in areas with poor health care access, while providing flexibility for other forms of communication in the short term as infrastructure develops, are critical to equitable access given the uptake and promise of telehealth.
Public efforts to create community broadband networks and expand low-cost internet service in areas with poor health care access, while providing flexibility for other forms of communication in the short term as infrastructure develops, are critical to equitable access given the uptake and promise of telehealth.
Citation
Loccoh EC, Nguyen A, Kim G, Warraich HJ. Geospatial Analysis of Access to Health Care and Internet Services in the US. JAMA Netw Open. 2022;5(11):e2243792. doi:10.1001/jamanetworkopen.2022.43792
Image credit:
https://hitconsultant.net/2021/09/10/healthcare-deserts-goodrx-report/
References
See the original publication