health transformation. institute
research institute & knowledge portal
Joaquim Cardoso MSc*
Chief Strategy Officer (CSO), Chief Researcher and Editor
November 21, 2022
MSc* from London Business School — MIT Sloan Masters Program
Executive Summary
What is the context?
- It is absolutely right that the NHS, which accounts for an increasing share of public spending, is expected to make efficiencies.
- And no one should doubt that there is waste within the NHS, as there is in other health care systems and industries.
- But history suggests that governments are chronically predisposed to setting unrealistically ambitious efficiency targets for the NHS.
What can happen to health services during funding squeezes?
- Increase income
- Reduce spending
- Increase productivity and efficiency
- Changes to financial management
What can we learn from the two rounds of £20 billion funding squeezes the NHS has faced since 2010?
- First, although health services have a surprisingly long menu of options for delivering efficiency savings ( see Table 1), they often rely on reducing central management costs; controlling public sector pay; and reducing payments to secondary care providers.
- Second, plans change — which makes it difficult to assess whether the Nicholson or Stevens challenges were ultimately achieved.
- Third, and most importantly — efficiency plans come with a cost.
The Pritchard challenge
- Convention suggests that funding squeezes are named after the chief executive of NHS England. So what does the incumbent Amanda Pritchard face? A bigger challenge with fewer tools perhaps?
- There are some new efficiency opportunities, such as more advanced digital technology and a greater focus on collaboration and sharing NHS resources (eg, through shared staff banks), but their impact remains largely untested
- And unlike its predecessors, the Pritchard challenge will take place with a concurrent challenges of economic depression and Covid-19.
- It will come after two periods of funding squeezes, where the NHS will argue that there is little fat left to cut — belts can’t be tightened much further when they hit bone.
- And things that would have been relied upon in the past — such as pay freezes — will surely be harder (but reportedly not beyond the pale) to deliver when some NHS nurses are preparing for strike action.
ORIGINAL PUBLICATION (The King´s Fund)

The Pritchard challenge: the next NHS efficiency drive
The King´s Fund
Siva Anandaciva
16 November 2022
Open a newspaper today and you will see stories about inflation, recession and cuts to public spending.
So you don’t have to be Nostradamus to predict the NHS is heading for another funding squeeze after the Autumn Statement, even if it is potentially spared from the full force of cuts other public services might face.
The NHS has been here before, so what can we learn from previous rounds of severe belt-tightening?
The Nicholson challenge
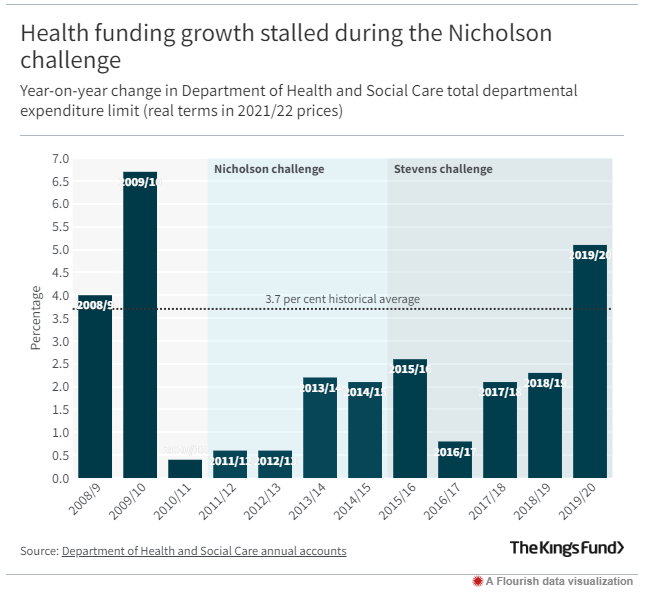
In 2010, just after the global financial crisis, the coalition government pledged to increase NHS spending in real terms over the coming years. But these increases would be far below the historical rises the NHS received ( see Figure 1),…
… so the NHS would need to deliver £15–20 billion of efficiency savings if it was going to balance its books, meet rising demand and maintain the quality of services between 2011/12 and 2014/5.
This then was the ‘Nicholson challenge’ — set by then NHS England Chief Executive Sir David Nicholson — to do more with less on an unprecedented scale.
… the NHS would need to deliver £15–20 billion of efficiency savings if it was going to balance its books, meet rising demand and maintain the quality of services between 2011/12 and 2014/5.
Underpinned by a national efficiency programme called Quality, Innovation, Productivity and Prevention (QIPP), and informed by modelling by McKinsey, the NHS planned to make these savings from national programmes (eg, public sector pay freezes and slashing management costs); frontline NHS providers (eg, by reducing the prices paid for delivering care); and local NHS commissioners or budget-holders (eg, shifting care out of hospitals, centralising services).

The Stevens challenge
The NHS was hoping for some respite after the most prolonged funding squeeze in its history. But it had another challenge coming.
In 2014, the new NHS England Chief Executive Simon Stevens published the Five Year Forward View, which forecast a further £30 billion NHS funding gap by 2020/21.
In 2014, the new NHS England Chief Executive Simon Stevens published the Five Year Forward View, which forecast a further £30 billion NHS funding gap by 2020/21.
The government responded in the 2015 Spending Review by topping up NHS budgets (but not wider health spending) by a further £8 billion in real terms by 2020/21 — which left a remaining efficiency requirement (the ‘Stevens challenge’) of £22 billion.
Some of these savings (roughly £7 billion) would be delivered nationally, including a further public sector pay freeze, renegotiating community pharmacy contracts and reducing administration budgets.
And the lion’s share of the remaining £15 billion would be delivered by ‘ conventional provider productivity ‘, ie, reducing prices paid to NHS secondary care providers.

Lessons from the past
So, what can we learn from the two rounds of £20 billion funding squeezes the NHS has faced since 2010?
First, although health services have a surprisingly long menu of options for delivering efficiency savings ( see Table 1), they often rely on reducing central management costs; controlling public sector pay; and reducing payments to secondary care providers.
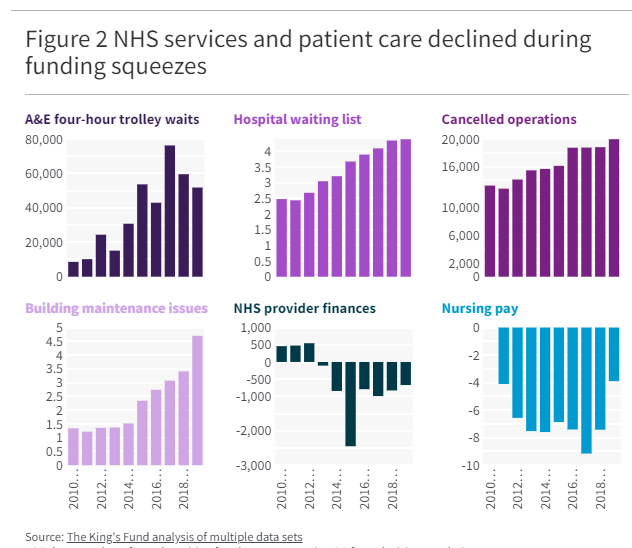
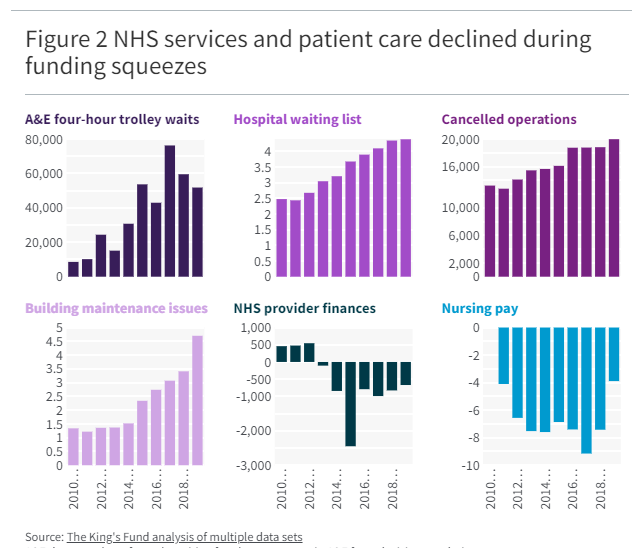
This may be understandable given how much NHS spending is tied to staffing costs and provider budgets, and where manager numbers are always in the target sights of ministers. But it is also a surprisingly crude set of tools: paying frontline providers less for the care they deliver is an incentive, but no guarantee, of greater efficiency. If anything, it only seemed to be a guarantee that financial distress would grow in these organisations ( see Figure 2).
First, although health services have a surprisingly long menu of options for delivering efficiency savings ( see Table 1), they often rely on reducing central management costs; controlling public sector pay; and reducing payments to secondary care providers.
Table 1 What can happen to health services during funding squeezes?
- Increase income
- Reduce spending
- Increase productivity and efficiency
- Changes to financial management
Increase income
- Increase government funding
- Increase private patient work
- Sell surplus land and assets
Reduce spending
- Reduce range of services offered on the NHS, eg, fewer cycles of IVF
- Restrict access to treatment, eg, higher referral criteria
- Reduce quality of services, eg, longer waiting times for care
- Reduce staffing pay costs, eg, redundancies, lower or frozen pay, reduce spending on agency and locum staff, lower staff education and training budgets
- Delay capital investment in buildings, equipment and technology
- Limit additional service spending, eg, fewer weekend and evening operating sessions
- Cap on management consultancy contracts
- Renegotiate prices on pharmaceutical products
Increase productivity and efficiency
- Improve procurement to reduce variation in prices paid for goods and services
- Reduce waste of unused inputs, eg, clinical supplies
- Reduce costly harm and errors in care, eg, safer prescribing initiatives
- Stop providing treatments and medicines that deliver little clinical value
- Reduce unwarranted variation in how clinical services are designed and delivered
- Redesign how care is delivered and clinical innovation, eg, day-case surgery
- Share back-office staff
Changes to financial management
- Incur financial deficits by overspending annual budgets
- Take out government or commercial loans to cover costs
- Delay payments to suppliers
- Remove ‘prudence’ from handling of bad debts and deferred income
- Divert capital investment budgets to support day-to-day spending
- Requesting additional sign-off on expenditure, eg, ministerial approval of salaries for very senior NHS managers
Notes: Some actions are time-limited (eg delaying payments to suppliers) and may benefit the annual financial position of individual organisations but not the NHS as a whole (eg financial deficits in providers have to be balanced elsewhere in the system). Other elements may result in lower spending even if they are not conscious attempts to save money (eg longer waits for care).
Second, plans change — which makes it difficult to assess whether the Nicholson or Stevens challenges were ultimately achieved.
Changes to inflation (NHS funding deals are often set out in cash terms) and top-ups to spending plans muddy the waters over just how much the NHS has saved and how much it needs to save over any given period (Figure 1). All of which emphasises the inefficient boom-and-bust approach to NHS funding that leaves the service on shifting sands when developing its savings plans.
Second, plans change — which makes it difficult to assess whether the Nicholson or Stevens challenges were ultimately achieved.
Third, and most importantly — efficiency plans come with a cost.
On one measure at least, the NHS met the Nicholson and Stevens challenges because it continued to balance its books. But a broader look at NHS services and patient care shows buildings and equipment were run-down to unsafe levels; pay was held down and staffing shortages ballooned; financial deficits became endemic and hard-fought progress in reducing waits for care was rapidly unwound ( see Figure 2). All of which left the health service in a fragile state just as Covid-19 entered the picture.
Third, and most importantly — efficiency plans come with a cost.
The Pritchard challenge
Convention suggests that funding squeezes are named after the chief executive of NHS England.
So what does the incumbent Amanda Pritchard face? A bigger challenge with fewer tools perhaps?
There are some new efficiency opportunities, such as more advanced digital technology and a greater focus on collaboration and sharing NHS resources (eg, through shared staff banks), but their impact remains largely untested.
And unlike its predecessors, the Pritchard challenge will take place with a concurrent challenges of economic depression and Covid-19.
It will come after two periods of funding squeezes, where the NHS will argue that there is little fat left to cut — belts can’t be tightened much further when they hit bone.
And things that would have been relied upon in the past — such as pay freezes — will surely be harder (but reportedly not beyond the pale) to deliver when some NHS nurses are preparing for strike action.
It is absolutely right that the NHS, which accounts for an increasing share of public spending, is expected to make efficiencies.
And no one should doubt that there is waste within the NHS, as there is in other health care systems and industries.
But history suggests that governments are chronically predisposed to setting unrealistically ambitious efficiency targets for the NHS.
Little wonder then that Amanda Pritchard has reportedly described the NHS’s financial position as ‘a [bleeping] nightmare’. An assessment her predecessors would surely have shared.
Originally published at https://www.kingsfund.org.uk on November 16, 2022.
Names mentioned
In 2014 NHS England Chief Executive Simon Stevens
incumbent Amanda Pritchard