Site editor:
Joaquim Cardoso MSc
The Health Institute — for continuous health transformation
October 3, 2022
Forbes
William Haseltime
October 3, 2022
Executive Summary (by the site editor)
Overview:
- New research published in Science Translational Medicine suggests an mRNA vaccine that targets both the SARS-CoV-2 spike protein (S) as well as the nucleocapsid protein (N) may offer stronger and broader protection than current, spike-only vaccines.
- This research opens the possibility that one vaccine may protect against current and future variants.
Rationale for Inclusion of Nucleocapsid Protein
- One of the most difficult challenges of the Covid-19 pandemic is accounting for the rise of new variants. Successive waves of infection and hospitalization are driven by the emergence and spread of fitter strains.
- These quickly push out prior strains as they rise to dominance.
- And, because Omicron sublineages can be as different from one another as the Alpha variant was from Delta, prior infection with one Omicron virus does not necessarily mean you will be protected against any of its relatives.
How current mRNA vaccines work?
- Current mRNA vaccines work by exposing our bodies to the SARS-CoV-2 spike protein, which the virus depends on to bind and eventually enter our cells. Antibodies that block the spike protein can block infection.
- The issue is that the spike protein is prone to mutation — its structure can change a lot without sacrificing functionality.
- By extension, vaccines based only on the spike protein risk losing efficacy when confronted with new variants.
What are the implications?
- This work by Hajnik et al. has laid the groundwork for the development of more broadly neutralizing Covid-19 vaccines, ones that can remain effective even in the face of continued viral variation.
- Research like this sets us on the path for the generation of a truly universal SARS-CoV-2 vaccine.
- Successes like these reemphasize the importance of continued funding and research on coronaviruses; the more we know about a virus, the easier it is to produce targeted and lasting interventions.
- This is true for vaccines and prophylactic drugs alike.

New research published in Science Translational Medicine suggests an mRNA vaccine that targets both the SARS-CoV-2 spike protein (S) as well as the nucleocapsid protein (N) may offer stronger and broader protection than current, spike-only vaccines.
This research opens the possibility that one vaccine may protect against current and future variants.
Rationale for Inclusion of Nucleocapsid Protein
One of the most difficult challenges of the Covid-19 pandemic is accounting for the rise of new variants.
Successive waves of infection and hospitalization are driven by the emergence and spread of fitter strains.
These quickly push out prior strains as they rise to dominance.
The Omicron family of viruses has asserted itself as king of the hill in 2022.
In large part, this is because the lineage has proven especially adept at evading vaccine induced immunity.
And, because Omicron sublineages can be as different from one another as the Alpha variant was from Delta, prior infection with one Omicron virus does not necessarily mean you will be protected against any of its relatives.
Current mRNA vaccines work by exposing our bodies to the SARS-CoV-2 spike protein, which the virus depends on to bind and eventually enter our cells. Antibodies that block the spike protein can block infection.
The issue is that the spike protein is prone to mutation — its structure can change a lot without sacrificing functionality.
By extension, vaccines based only on the spike protein risk losing efficacy when confronted with new variants.
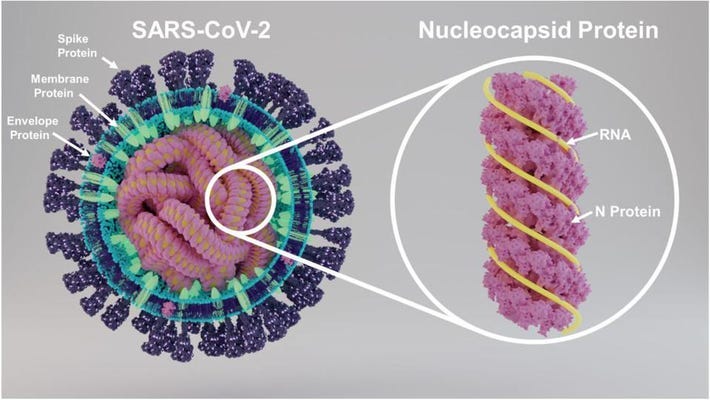
The nucleocapsid protein is a structural protein with an integral role in viral assembly and the packaging of genetic material (Figure 1).
It is 90% conserved between SARS-CoV-1 and SARS-CoV-2, compared to 76% for the spike protein.
These two features combined make it a very promising target for vaccine design.
Added to this is the fact the nucleocapsid protein has been shown to elicit a powerful T cell response.
Where B cells produce antibodies that can bind to viral particles before they enter cells, T cells are in charge of destroying host cells already infected with the virus; the stronger the T cell response, the better the body can contain the spread of the virus and clear the infection.
Analyses of people infected with SARS-CoV-1 have indicated that N-specific T cell immunity can be very long lasting, with some individuals retaining memory T cells up to 17 years after initial infection.
These same T cells managed to recognize the SARS-CoV-2 nucleocapsid protein, mounting a quick and specific immune response.
Analyses of people infected with SARS-CoV-1 have indicated that N-specific T cell immunity can be very long lasting, with some individuals retaining memory T cells up to 17 years after initial infection.
Animal Models: mRNA-N Vaccine
First up, Hajnik et al. tested their vaccine for its ability to produce an immune response, known as immunogenicity.
For this, they separated mice into a control group, which was vaccinated with a saline solution, and a test group, which received the mRNA-N vaccine.
The mRNA-N vaccine was administered intramuscularly in two doses, an initial prime and a boost three weeks later (Figure 2).
Two weeks after the booster shot, the scientists euthanized the mice and analyzed their blood, with a focus on T and B cell responses.
Compared to the mock group, mice vaccinated with the mRNA-N vaccine displayed strong CD4+ and CD8+ T cell responses.
CD4+ T cells, also known as helper T cells, activate a number of other immune cells and help orchestrate the immune response.
CD8+ T cells, or killer T cells, actively recognize and destroy infected host cells, slowing the spread of the infection.
The N-specific T cells expressed three important signaling molecules: interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), and interleukin-2 (IL-2). Interferon-γ is the primary activator of immune cells called macrophages, which engulf and destroy invading microbes.
Tumor necrosis factor-α is a vital component of our inflammatory response, and can induce regulated cell death in infected or damaged tissues.
And interleukin-2 helps stimulate the growth and proliferation of T and B cells.
Hajnik et al. also witnessed a clear induction of nucleocapsid-specific immunoglobulin G (IgG) antibodies following vaccination.
However, although these antibodies could bind the nucleocapsid protein, they did not have any neutralizing potency, meaning they cannot help prevent infection of our cells.
Next, they tested their vaccine against live infection in mice and hamsters.
They used the same timeline as they did for their immunological analysis: one prime dose followed by a booster three weeks later.
They infected the mice with a mouse-adapted SARS-CoV-2 strain two weeks after administration of the booster shot.
They did the same for the hamsters, albeit with the Delta variant, since hamsters are susceptible to wild-type SARS-CoV-2 infection.
Two days post infection, the researchers looked at viral loads in the lungs of the mice and hamsters.
Compared to the control group, mice and hamsters vaccinated with mRNA-N showed a reduction in viral RNA and in infectious viral titers.
This reduction was statistically significant, but only modest.
Curiously, no such reduction was seen when the vaccine was administered intranasally instead of intramuscularly.
Intranasal administration also failed to induce any antibody response.
Curiously, no such reduction was seen when the vaccine was administered intranasally instead of intramuscularly.
Intranasal administration also failed to induce any antibody response.
To pinpoint the protective effect of the vaccine, Hajnik and colleagues depleted CD8+ T cells in one group of hamsters.
They did this by administering antibodies that bind to CD8+ T cells, effectively blocking them and impairing their function.
Depletion of CD8+ T cells almost entirely eliminated the protective effects of mRNA-N vaccination, with no noticeable reduction of viral loads in the lungs.
This implicates N-specific CD8+ T cells as the key component of viral control.
One important drawback is that there was no noticeable reduction of viral loads in the upper respiratory tract following mRNA-N vaccination.
The scientists suggest this may be due to the vaccine’s inability to stimulate neutralizing antibodies.

Animal Models: mRNA-N+S Vaccine
Given their initial success with the nucleocapsid-based vaccine, Hajnik et al. created a bivalent mRNA vaccine that targets both the nucleocapsid protein as well as the spike protein.
To test the efficacy of the combination mRNA-N+S vaccine, they compared it to an mRNA vaccine containing only the spike protein (mRNA-S) and to a mock vaccine based on saline solution.
Again they used a mouse model as well as a hamster model.
Both the mRNA-N+S vaccine and the mRNA-S vaccine managed to successfully control the infection, with almost no detectable infectious virus in the lungs.
A more fine-grained analysis using reverse transcription polymerase chain reaction (RT-PCR) technology revealed that the combination vaccine outperformed the spike-only vaccine; the spike-only vaccine managed to reduce viral RNA copies in the lungs to barely detectable levels, but the combination vaccine was able to completely eradicate viral loads in the lungs (Figure 3).
The vaccines fared just as well against the Delta virus in hamster models.
But again, the mRNA-N+S vaccine outperformed the spike-only vaccine, and this time by a larger margin.
Where the mRNA-S vaccine managed to reduce lung viral RNA copies 57-fold compared to mock, the mRNA-S+N vaccine managed to do so by 770-fold. Still, both vaccines protected against lung damage, including bronchiolitis and interstitial pneumonia.
Addition of the spike protein to the vaccine also helped improve its efficacy in the upper respiratory tract.
As with the nucleocapsid-only vaccine, the spike-only vaccine was not that effective in clearing the virus from the nose and throat, with only a five-fold decrease in viral mRNA copies four days after initial infection.
Compare this to the mRNA-N+S vaccine, which already provided an eleven-fold decrease two days after initial infection.
This rose to a 98-fold decrease by four days post infection. So, the bivalent nucleocapsid/spike vaccine provides stronger and faster control of SARS-CoV-2 Delta in the lungs and upper respiratory tract compared to the spike-only vaccine.

What about Omicron?
To test the breadth of the immune response elicited by the mRNA-N+S vaccine, Hajnik et al. also exposed hamsters to the Omicron variant (BA.1).
They split the hamsters into four groups: one that received a mock vaccine, one that received a two microgram dose of spike-only vaccine, one that received a four microgram dose of spike-only vaccine, and finally one that received the mRNA-N+S vaccine, which included two micrograms of each protein.
At two micrograms, the spike-only vaccine induced modest viral clearance from the lungs; a 12-fold reduction in viral RNA copies two days after infection.
Little changed with the four microgram dose, which produced only modest viral control very similar to that of the smaller dose.
The mRNA-N+S vaccine, in contrast, managed to completely clear viral RNA copies from the lungs by day two of the infection.
The same held true for viral titers, with four out of five hamsters having no detectable levels of infectious virus.
Results in the upper respiratory tract mirrored those seen with Delta: the spike-only vaccine only weakly reduced viral RNA copies compared to the mock vaccine.
The combination vaccine again outperformed the others, managing to produce a 3-fold decrease in viral copies two days after initial infection.
This suggests a combination vaccine may be better suited to reducing viral shedding and possibly onwards transmission of the virus.
This suggests a combination vaccine may be better suited to reducing viral shedding and possibly onwards transmission of the virus.

Implications
This work by Hajnik et al. has laid the groundwork for the development of more broadly neutralizing Covid-19 vaccines, ones that can remain effective even in the face of continued viral variation.
Research like this sets us on the path for the generation of a truly universal SARS-CoV-2 vaccine.
Successes like these reemphasize the importance of continued funding and research on coronaviruses; the more we know about a virus, the easier it is to produce targeted and lasting interventions.
This is true for vaccines and prophylactic drugs alike.
Research like this sets us on the path for the generation of a truly universal SARS-CoV-2 vaccine.
Originally published at https://www.forbes.com
ORIGINAL PUBLICATION
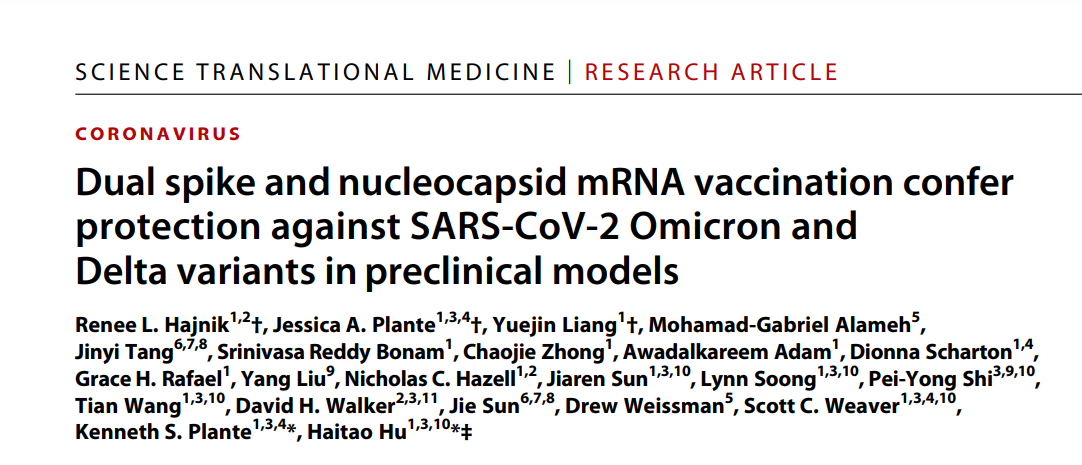
Dual spike and nucleocapsid mRNA vaccination confer protection against SARS-CoV-2 Omicron and Delta variants in preclinical models
SCIENCE TRANSLATIONAL MEDICINE
Renee L. Hajnik1,2 †, Jessica A. Plante1,3,4 †, Yuejin Liang1 †, Mohamad-Gabriel Alameh5 , Jinyi Tang6,7,8 , Srinivasa Reddy Bonam1 , Chaojie Zhong1 , Awadalkareem Adam1 , Dionna Scharton1,4 , Grace H. Rafael1 , Yang Liu9 , Nicholas C. Hazell1,2 , Jiaren Sun1,3,10, Lynn Soong1,3,10, Pei-Yong Shi3,9,10, Tian Wang1,3,10, David H. Walker2,3,11, Jie Sun6,7,8 , Drew Weissman5 , Scott C. Weaver1,3,4,10, Kenneth S. Plante1,3,4 *, Haitao Hu1,3,10*‡
About the authors affiliations:
1 Department of Microbiology and Immunology, University of Texas Medical Branch, Galveston, TX 77555, USA.
2 Department of Pathology, University of Texas Medical Branch, Galveston, TX 77555, USA.
3 Institute for Human Infections and Immunity, University of Texas Medical Branch, Galveston, TX 77555, USA.
4 World Reference Center for Emerging Viruses and Arboviruses, University of Texas Medical Branch, Galveston, TX 77555, USA.
5 Department of Medicine, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA 19104, USA.
6 Division of Pulmonary and Critical Medicine, Department of Medicine, Mayo Clinic, Rochester, MN 55905, USA.
7 Carter Immunology Center, University of Virginia, Charlottesville, VA 22908, USA.
8 Division of Infectious Disease and International Health, Department of Medicine, University of Virginia, Charlottesville, VA 22908, USA.
9 Department of Biochemistry and Molecular Biology, University of Texas Medical Branch, Galveston, TX 77555, USA.
10Sealy Institute for Vaccine Sciences, University of Texas Medical Branch, Galveston, TX 77555, USA.
11Center for Biodefense and Emerging Infectious Diseases, University of Texas Medical Branch, Galveston, TX 77555, USA.
Doubling up on antigens
As additional SARS-CoV-2 variants evolve, vaccines that maintain efficacy across these variants become increasingly important. Here, Hajnik et al. tested whether an mRNA vaccine encoding the more conserved nucleocapsid (N) protein of SARS-CoV-2 can elicit responses that protect against SARS-CoV-2 challenge in vivo. mRNA-N vaccination alone elicited immune responses that could control SARS-CoV-2. Furthermore, combining mRNA-N vaccination with an mRNA vaccine encoding the spike protein (mRNA-S+N) induced better viral control than mRNA-S vaccination alone, including against the Omicron variant. Thus, incorporating the N protein into SARS-CoV-2 vaccines may promote protection against existing and future variants.
Abstract
Emergence of SARS-CoV-2 variants of concern (VOCs), including the highly transmissible Omicron and Delta strains, has posed constant challenges to the current COVID-19 vaccines that principally target the viral spike protein (S). Here, we report a nucleoside-modified messenger RNA (mRNA) vaccine that expresses the more conserved viral nucleoprotein (mRNA-N) and show that mRNA-N vaccination alone can induce modest control of SARS-CoV-2. Critically, combining mRNA-N with the clinically proven S-expressing mRNA vaccine (mRNA-S+N) induced robust protection against both Delta and Omicron variants. In the hamster models of SARS-CoV-2 VOC challenge, we demonstrated that, compared to mRNA-S alone, combination mRNA-S+N vaccination not only induced more robust control of the Delta and Omicron variants in the lungs but also provided enhanced protection in the upper respiratory tract. In vivo CD8+ T cell depletion suggested a potential role for CD8+ T cells in protection conferred by mRNA-S+N vaccination. Antigen-specific immune analyses indicated that N-specific immunity, as well as augmented S-specific immunity, was associated with enhanced protection elicited by the combination mRNA vaccination. Our findings suggest that combined mRNA-S+N vaccination is an effective approach for promoting broad protection against SARS-CoV-2 variants.