Depression and anxiety among the top causes of health loss worldwide, increased by Covid-19
IHME
November, 2021
flowneuroscience
This post discusses suicide and some people might find it disturbing. If you or someone you know is suicidal, please, contact your physician, visit your local ER, or call the suicide prevention hotline in your location.
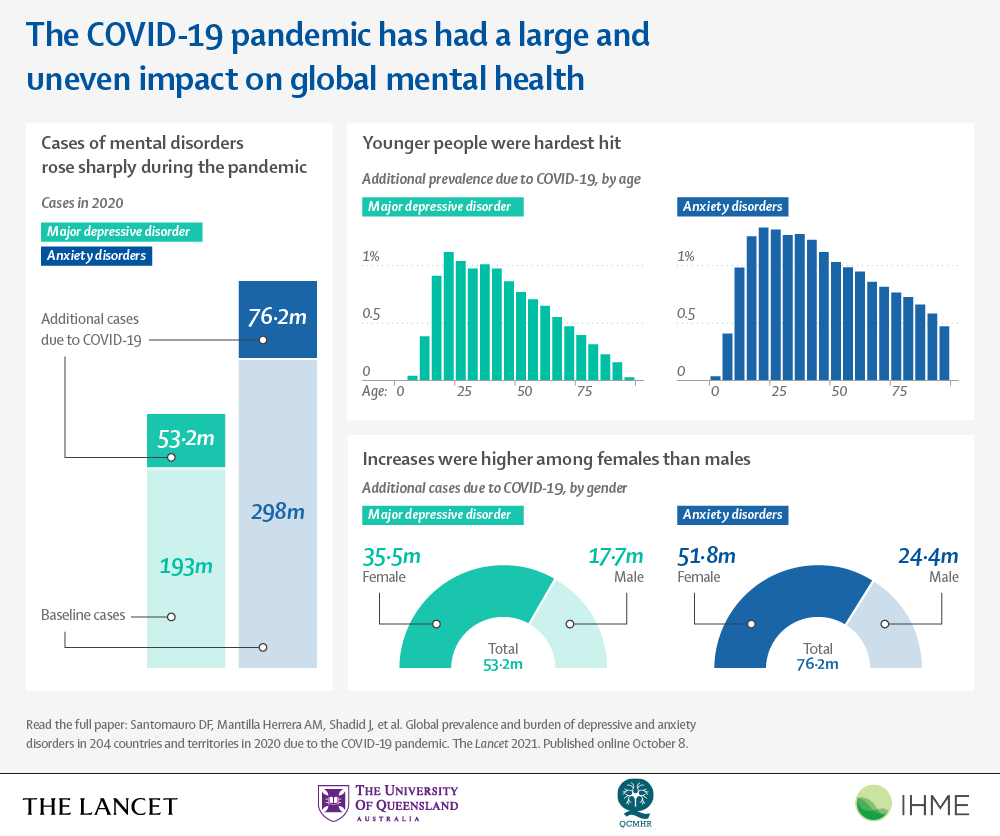
As we near the third year of the COVID-19 pandemic, a noticeable and disproportionate increase in the global burden of depressive and anxiety disorders has impacted the mental health of women and children worldwide.
According to a new analysis published in The Lancet showing that the COVID-19 pandemic led to a stark rise in depressive and anxiety disorders globally in 2020,
the overall number of cases of mental disorders rose dramatically, with an additional 53.2 million and 76.2 million cases of anxiety and major depressive disorders (MDD), respectively.
Method
The study assessed the global impact of the pandemic on anxiety disorders and MDD and quantified the prevalence and burden of the disorders by age, sex, and location in 204 countries and territories, noting that the increase in the prevalence of anxiety disorders and MDD during 2020 was associated with both the increasing COVID-19 infection rates and decreasing human mobility.
The COVID-19 impact indicators incorporated the combined impacts of the spread of the virus, lockdowns, stay-at-home orders, decreased public transportation, school, and business closures, and decreased social interactions, among others.
Globally, anxiety disorders prevalence was strongly associated with increased infection rates, while MDD prevalence was more associated with decreasing human mobility.
Those whose mental health was most affected by these indicators are women and children.
Among women, there were almost 52 million additional cases of anxiety disorders and more than 35 million additional MDD cases present in 2020, compared to 2019.
Mental disorders were anticipated to have a greater impact on females as they are more likely impacted by the social and economic consequences of the pandemic, specifically as challenges like school closures and illness disproportionately required women-especially those who were more likely to be financially disadvantaged during the pandemic due to lower salaries and savings than their male counterparts-to fill the role of caretaker.
This comes as no shock, as females generally are more susceptible to depression and anxiety disorders compared to males, with susceptibility starting before the age of 15.
It is not uncommon for adolescents to be diagnosed with mental disorders: 1 in 7 adolescents aged 10 to 19 years are currently diagnosed globally, according to UNICEF.
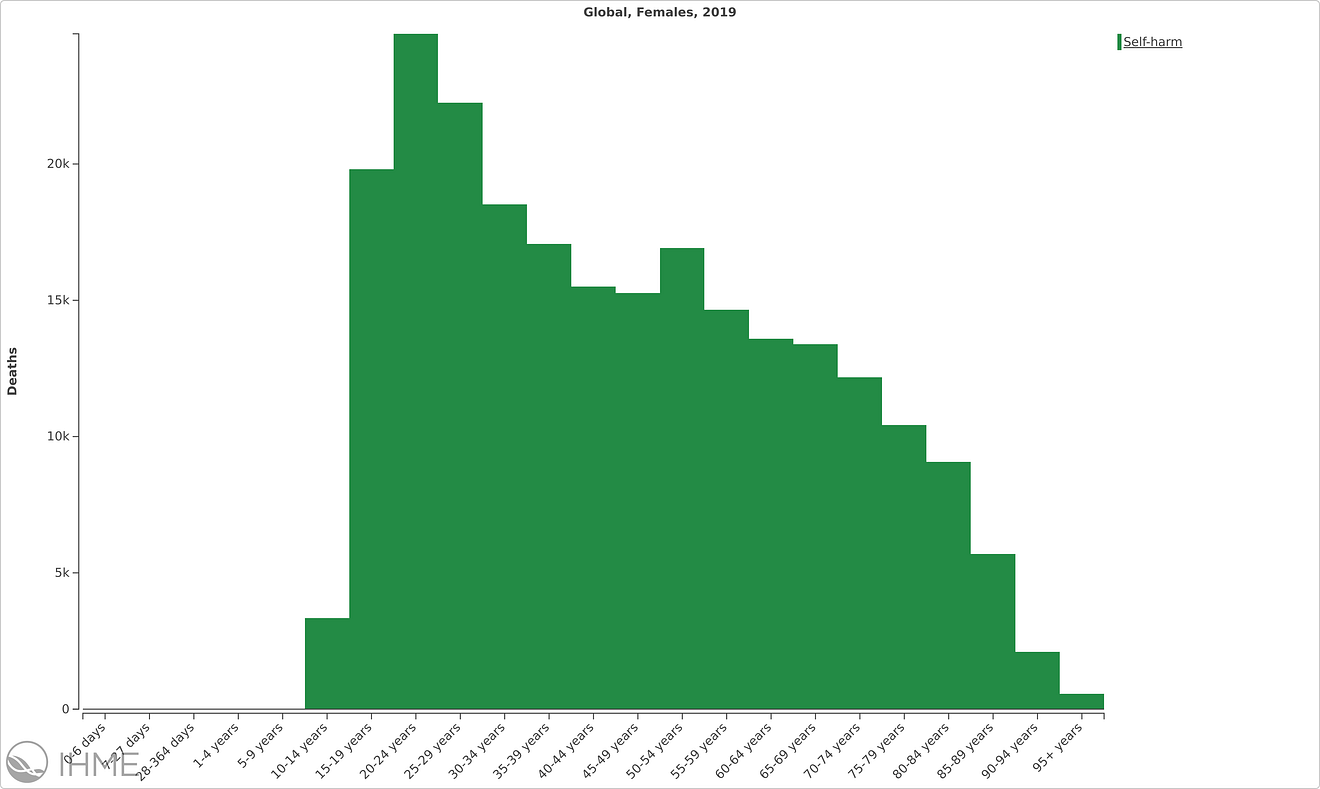
Self-harm deaths in women globally in 2019, GBD 2019
Younger people were more affected by major depressive disorder and anxiety disorders in 2020 than older age groups.
The additional prevalence of these disorders peaked among those aged 20–24 years (1,118 additional cases of major depressive disorder per 100,000 and 1,331 additional cases of anxiety disorders per 100,000) and declined with increasing age .
According to the Global Burden of Disease 2019, self-inflicted injuries are a main cause of death worldwide in adolescent girls, and suicide is the leading cause of death for girls and women between 15 and 19 globally; 46,000 adolescents die from suicide each year, a top 5 cause of death in their age group.
Complemented by the challenges of the pandemic, 1 in 7 children have been directly affected by the lockdown, and 1.6 billion children have suffered a loss of education from being fully or partially out of school in 2020.
With school closures and wider social restrictions in place, young people’s ability to learn and interact with their peers has been hindered.
Furthermore, youth are more likely to become unemployed during and following economic crises, as mental health disorders directly impact lost contributions to economies at nearly $390 billion a year.
Despite the economic loss, 2% of government health budgets are allocated to mental health spending globally, according to UNICEF.
The greater impact among women and young people was likely because they are more impacted by the social and economic consequences of the pandemic, which has created a greater urgency to strengthen mental health systems through policy-based methods of action that address the burden of anxiety disorders and MDD globally.
Even before the COVID-19 pandemic, mental health disorders posed a significant burden worldwide.
In 2019, depression was the second-leading cause of disability globally, and anxiety ranked eighth, both being the most common types of mental health disorders.
While men and women experienced similar rates of mental health disorders overall, depressive, anxiety and eating disorders were more common in women, while ADHD and autism spectrum disorders were more common in men.
Global disability-adjusted life-years (DALYs) by mental disorder, sex, and age in 2019
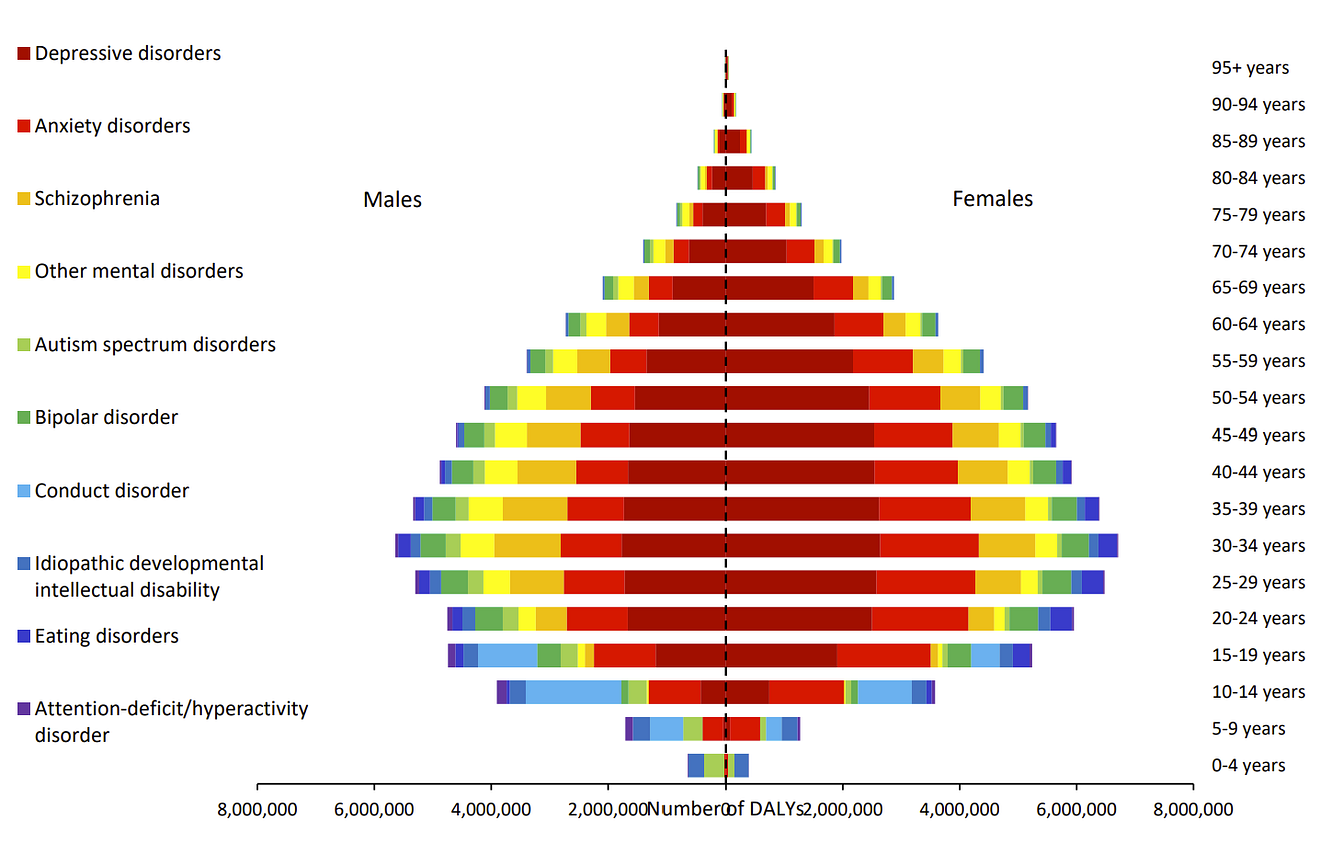
Health loss due to mental health disorders tends to peak between ages 25 and 34, increasing during childhood and adolescence and decreasing steadily into older ages.
In 2019, this translated into over 80% of the burden of mental health disorders falling on those between 16 and 65 years, which are primary working ages.
Overall, the highest prevalence of mental health disorders was in the regions of Australasia, Tropical Latin America, and high-income North America.
However, when looking only at depressive disorders, sub-Saharan Africa, North Africa, and the Middle East all stood out for high levels.
For low-income countries that may lack funding or other resources for health infrastructure, it can be particularly challenging to address mental health needs as they are often overlooked.
In addition to shortages of mental health services, other barriers can prevent people from receiving treatment, like social stigma or their own perceived need.
Despite policies aimed at reducing mental health disorders, not much has changed in the past two decades at the global level.
Since 1990, the age-standardized rate of health loss has stayed roughly the same, and the total amount has increased by about 55%, a result of rising population size.
The demand for mental health services has never been greater, and it is imperative that countries do not neglect this demand as they work to enhance public health services.
Mental health is a human right, and people in all countries, at all income levels deserve access to treatment and prevention resources.
Originally published at http://www.healthdata.org on October 7, 2021.
ORIGINAL PUBLICATION
Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic
The Lancet
COVID-19 Mental Disorders Collaborators †
November 6, 2021
SUMMARY (excerpted)
Background
Before 2020, mental disorders were leading causes of the global health-related burden, with depressive and anxiety disorders being leading contributors to this burden. The emergence of the COVID-19 pandemic has created an environment where many determinants of poor mental health are exacerbated. The need for up-to-date information on the mental health impacts of COVID-19 in a way that informs health system responses is imperative. In this study, we aimed to quantify the impact of the COVID-19 pandemic on the prevalence and burden of major depressive disorder and anxiety disorders globally in 2020.
Methods
We conducted a systematic review of data reporting the prevalence of major depressive disorder and anxiety disorders during the COVID-19 pandemic and published between Jan 1, 2020, and Jan 29, 2021. We searched PubMed, Google Scholar, preprint servers, grey literature sources, and consulted experts. Eligible studies reported prevalence of depressive or anxiety disorders that were representative of the general population during the COVID-19 pandemic and had a pre-pandemic baseline. We used the assembled data in a meta-regression to estimate change in the prevalence of major depressive disorder and anxiety disorders between pre-pandemic and mid-pandemic (using periods as defined by each study) via COVID-19 impact indicators (human mobility, daily SARS-CoV-2 infection rate, and daily excess mortality rate). We then used this model to estimate the change from pre-pandemic prevalence (estimated using Disease Modelling Meta-Regression version 2.1 [known as DisMod-MR 2.1]) by age, sex, and location. We used final prevalence estimates and disability weights to estimate years lived with disability and disability-adjusted life-years (DALYs) for major depressive disorder and anxiety disorders.
Findings
We identified 5683 unique data sources, of which 48 met inclusion criteria (46 studies met criteria for major depressive disorder and 27 for anxiety disorders). Two COVID-19 impact indicators, specifically daily SARS-CoV-2 infection rates and reductions in human mobility, were associated with increased prevalence of major depressive disorder (regression coefficient [B] 0·9 [95% uncertainty interval 0·1 to 1·8; p=0·029] for human mobility, 18·1 [7·9 to 28·3; p=0·0005] for daily SARS-CoV-2 infection) and anxiety disorders (0·9 [0·1 to 1·7; p=0·022] and 13·8 [10·7 to 17·0; p<0·0001]. Females were affected more by the pandemic than males (B 0·1 [0·1 to 0·2; p=0·0001] for major depressive disorder, 0·1 [0·1 to 0·2; p=0·0001] for anxiety disorders) and younger age groups were more affected than older age groups (−0·007 [–0·009 to −0·006; p=0·0001] for major depressive disorder, −0·003 [–0·005 to −0·002; p=0·0001] for anxiety disorders). We estimated that the locations hit hardest by the pandemic in 2020, as measured with decreased human mobility and daily SARS-CoV-2 infection rate, had the greatest increases in prevalence of major depressive disorder and anxiety disorders. We estimated an additional 53·2 million (44·8 to 62·9) cases of major depressive disorder globally (an increase of 27·6% [25·1 to 30·3]) due to the COVID-19 pandemic, such that the total prevalence was 3152·9 cases (2722·5 to 3654·5) per 100 000 population. We also estimated an additional 76·2 million (64·3 to 90·6) cases of anxiety disorders globally (an increase of 25·6% [23·2 to 28·0]), such that the total prevalence was 4802·4 cases (4108·2 to 5588·6) per 100 000 population. Altogether, major depressive disorder caused 49·4 million (33·6 to 68·7) DALYs and anxiety disorders caused 44·5 million (30·2 to 62·5) DALYs globally in 2020.
Interpretation
This pandemic has created an increased urgency to strengthen mental health systems in most countries.
Mitigation strategies could incorporate ways to promote mental wellbeing and target determinants of poor mental health and interventions to treat those with a mental disorder.
Taking no action to address the burden of major depressive disorder and anxiety disorders should not be an option.
Research in context
Evidence before this study
For our study, we did a systematic literature review of the peer-reviewed and grey literature for studies published between Jan 1, 2020, and Jan 29, 2021, investigating prevalence of depressive and anxiety disorders during the COVID-19 pandemic. Most of the identified work consisted of surveys done for a specific location, at a snapshot in time, and indicated an increase in prevalence of depressive and anxiety disorders during the COVID-19 pandemic. We also found several systematic reviews and meta-analyses to summarise these studies; however, these studies were either qualitative syntheses or simply presented pooled estimates across studies. We did not find any studies that attempted to synthesise the global prevalence and burden of depressive and anxiety disorders due to the COVID-19 pandemic for the year 2020.
Added value of this study
This study is the first to quantify the prevalence and burden of depressive and anxiety disorders by age, sex, and location globally. We compiled available evidence of the change in the prevalence of major depressive disorder and anxiety disorders during the COVID-19 pandemic. We then developed a model to estimate the prevalence of major depressive disorder and anxiety disorders by age, sex, and location on the basis of available indicators of the location-specific impact of the COVID-19 pandemic. We then used prevalence to estimate the burden of major depressive disorder and anxiety disorders due to the COVID-19 pandemic in 2020.
Implications of all the available evidence
We found that depressive and anxiety disorders increased during 2020 due to the COVID-19 pandemic.
Even before the COVID-19 pandemic, depressive and anxiety disorders featured as leading causes of burden globally, despite the existence of intervention strategies that can reduce their effects.
Meeting the added demand for mental health services due to COVID-19 will be difficult, but not impossible.
Mitigation strategies should promote mental wellbeing and target determinants of poor mental health exacerbated by the pandemic, as well as interventions to treat those who develop a mental disorder.
Introduction (excerpted)
Mental disorders are among the leading causes of the global health-related burden.
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 showed that the two most disabling mental disorders were depressive and anxiety disorders, both ranked among the top 25 leading causes of burden worldwide in 2019.1 ,2
This burden was high across the entire lifespan, for both sexes, and across many locations. 2
Perhaps more importantly, no reduction in the global prevalence or burden was detected for either disorder since 1990, despite compelling evidence of interventions that reduce their impact.3
The emergence of the COVID-19 pandemic in 2020 against this backdrop has raised many questions around the resulting effects on mental health via its direct psychological effects and long-term economic and social consequences. 4
COVID-19 continues to spread across most of the world’s populations 1 , 2 with significant health consequences and mortality among those who become infected. 5
In addition to the direct effects of COVID-19, the pandemic has created an environment in which many determinants of mental health are also affected.
Social restrictions, lockdowns, school and business closures, loss of livelihood, decreases in economic activity, and shifting priorities of governments in their attempt to control COVID-19 outbreaks all have the potential to substantially affect the mental health of the population.
The need for up-to-date information on the global prevalence and burden of mental disorders incorporating the mental health impacts of COVID-19 in a way that informs health system responses has never been more urgent.
GBD 2020 is in the process of estimating the burden of 370 diseases and injuries 88 risk factors across 204 countries and territories.
GBD 2020 is quantifying the burden using disability-adjusted life-years (DALYs), which represent the number of years of healthy life lost to either mortality or disability.
Here, as part of GBD 2020, we present a method built on the mental disorder estimates presented in GBD 2019 by incorporating the effect of the COVID-19 pandemic. We quantify the impact of COVID-19 on the prevalence and burden of major depressive disorder and anxiety disorders by location, age, and sex in 2020.
Funding
Queensland Health, National Health and Medical Research Council, and the Bill and Melinda Gates Foundation.
About the authors & affiliations
COVID-19 Mental Disorders Collaborators
Damian F Santomauro, Ana M Mantilla Herrera, Jamileh Shadid, Peng Zheng, Charlie Ashbaugh, David M Pigott, Cristiana Abbafati, Christopher Adolph, Joanne O Amlag, Aleksandr Y Aravkin, Bree L Bang-Jensen, Gregory J Bertolacci, Sabina S Bloom, Rachel Castellano, Emma Castro, Suman Chakrabarti, Jhilik Chattopadhyay, Rebecca M Cogen, James K Collins, Xiaochen Dai, William James Dangel, Carolyn Dapper, Amanda Deen, Megan Erickson, Samuel B Ewald, Abraham D Flaxman, Joseph Jon Frostad, Nancy Fullman, John R Giles, Ababi Zergaw Giref, Gaorui Guo, Jiawei He, Monika Helak, Erin N Hulland, Bulat Idrisov, Akiaja Lindstrom, Emily Linebarger, Paulo A Lotufo, Rafael Lozano, Beatrice Magistro, Deborah Carvalho Malta, Johan C Månsson, Fatima Marinho, Ali H Mokdad, Lorenzo Monasta, Paulami Naik, Shuhei Nomura, James Kevin O’Halloran, Samuel M Ostroff, Maja Pasovic, Louise Penberthy, Robert C Reiner Jr, Grace Reinke, Antonio Luiz P Ribeiro, Aleksei Sholokhov, Reed J D Sorensen, Elena Varavikova, Anh Truc Vo, Rebecca Walcott, Stefanie Watson, Charles Shey Wiysonge, Bethany Zigler, Simon I Hay, Theo Vos, Christopher J L Murray, Harvey A Whiteford, Alize J Ferrari.
Affiliations
School of Public Health (D F Santomauro PhD, A M Mantilla Herrera PhD, J Shadid BSc, A Lindstrom MEpi, Prof H A Whiteford PhD, A J Ferrari PhD), The University of Queensland, Herston, QLD, Australia; Queensland Centre for Mental Health Research (D F Santomauro PhD, A M Mantilla Herrera PhD, J Shadid BSc, A Lindstrom MEpi, Prof H A Whiteford PhD, A J Ferrari PhD), Wacol, QLD, Australia; Institute for Health Metrics and Evaluation (D F Santomauro PhD, A M Mantilla Herrera PhD, J Shadid BSc, P Zheng PhD, C Ashbaugh MA, D M Pigott PhD, J O Amlag MPH, A Y Aravkin PhD, B L Bang-Jensen MA, G J Bertolacci BS, S S Bloom BA, R Castellano MA, E Castro MS, S Chakrabarti MA, J Chattopadhyay MS, R M Cogen BA, J K Collins BS, X Dai PhD, W J Dangel Med, C Dapper MA, A Deen MPH, Miss M Erickson MA, S B Ewald MS, A D Flaxman PhD, J J Frostad MPH, N Fullman MPH, J R Giles PhD, G Guo MPH, J He MSc, M Helak BA, E N Hulland MPH, E Linebarger BA, Prof R Lozano MD, J C Månsson MS, Prof A H Mokdad PhD, P Naik MSPH, J K O’Halloran MS, S M Ostroff PhD, M Pasovic MA, L Penberthy MS, G Reinke MA, R C Reiner Jr PhD, A Sholokhov MSc, R J D Sorensen MPH, A T Vo BSc, S Watson MS, B Zigler MPH, Prof S I Hay FMedSci, Prof T Vos PhD, Prof C J L Murray DPhil, Prof H A Whiteford PhD, A J Ferrari PhD), Department of Health Metrics Sciences, School of Medicine (D M Pigott PhD, A Y Aravkin PhD, X Dai PhD, A D Flaxman PhD, Prof R Lozano MD, Prof A H Mokdad PhD, R C Reiner Jr PhD, Prof S I Hay FMedSci, Prof T Vos PhD, Prof C J L Murray DPhil), Department of Political Science (Prof C Adolph PhD), Department of Applied Mathematics (A Y Aravkin PhD), Department of Global Health (S Chakrabarti MA, E N Hulland MPH, R J D Sorensen MPH), Henry M Jackson School of International Studies (S M Ostroff PhD), Evans School of Public Policy & Governance (R Walcott MPH), University of Washington, Seattle, WA, USA; Department of Juridical and Economic Studies (C Abbafati PhD), La Sapienza University, Rome, Italy; Department of Health Systems and Policy (A Z Giref PhD), Addis Ababa University, Addis Ababa, Ethiopia; National Data Management Center (A Z Giref PhD), Ethiopian Public Health Institute, Addis Ababa, Ethiopia; Infectious Diseases Department (B Idrisov MD), Bashkir State Medical University, Ufa, Russia; Laboratory of Public Health Indicators Analysis and Health Digitalization (B Idrisov MD), Moscow Institute of Physics and Technology, Moscow, Russia; Department of Medicine (Prof P A Lotufo DrPH), University of Sao Paulo, Sao Paulo, Brazil; Munk School of Global Affairs and Public Policy (B Magistro PhD), University of Toronto, Toronto, ON, Canada; Department of Maternal and Child Nursing and Public Health (Prof D C Malta PhD), Public Health (F Marinho PhD), Department of Internal Medicine (Prof A P Ribeiro MD), Centre of Telehealth (Prof A P Ribeiro MD), Federal University of Minas Gerais, Belo Horizonte, Brazil; Public Health (F Marinho PhD), Vital Strategies, Sao Paulo, Brazil; Clinical Epidemiology and Public Health Research Unit (L Monasta DSc), Burlo Garofolo Institute for Maternal and Child Health, Trieste, Italy; Department of Health Policy and Management (S Nomura PhD), Keio University, Tokyo, Japan; Department of Global Health Policy (S Nomura PhD), University of Tokyo, Tokyo, Japan; Central Research Institute of Cytology and Genetics (E Varavikova PhD), Federal Research Institute for Health Organization and Informatics of the Ministry of Health (FRIHOI), Moscow, Russia; Cochrane South Africa (Prof C S Wiysonge MD), South African Medical Research Council, Cape Town, South Africa; School of Public Health and Family Medicine (Prof C S Wiysonge MD), University of Cape Town, Cape Town, South Africa
Originally published at https://www.thelancet.com