the
health strategist
portal
the knowledge portal of “the health strategist — institute”
for in-person health strategy
and digital health strategy
Joaquim Cardoso MSc
Chief Researcher and Strategy Officer (CRSO)
for “the health strategist ” — research unit
Chief Editor for“the health strategist” — knowledge portal
Senior Advisor — for “the health strategist” — advisory consulting
July 13, 2023
ONE PAGE SUMMARY
What is the problem?
- Rising costs of medications and growing disparities in drug access and outcomes.
- Current policies focus on drug price negotiations, patent reforms, and spending caps but overlook the potential of value-based payment (VBP) models.
What are the causes?
- Lack of integration of drugs into VBP models due to design and implementation barriers:
– Disparate funding streams in Medicare.
– Limited data on drug costs and effectiveness available to prescribing clinicians.
– Complexity in incorporating drugs into new payment approaches.
What are the recommendations:
- Enhance data availability to support informed decision-making by clinicians.
- Tailor VBP models for different categories of drugs to address specific challenges.
- Include quality measures in VBP models to encourage appropriate drug utilization.
- Provide incentives for high-value prescribing practices and use of efficacious treatments.
- Align provider financial incentives with goals to reduce total drug spending.
- Explore a spectrum of options in designing VBP models for different segments of the drug market.
- Incorporate drugs into accountable care programs and total cost-of-care VBP models.
Conclusion:
- The inclusion of drugs in VBP models is crucial for improving access, utilization, and equity in drug spending.
- Addressing barriers and tailoring VBP models can lead to better outcomes, cost savings, and enhanced data-driven decision-making.
- Policymakers and payers should explore various options to integrate drugs into VBP models and consider the unique challenges of different drug market segments.
DEEP DIVE

How Value-Based Payment Can Improve Drug Spending, Utilization, and Equity
Commonwealth Fund
Kristen Ukeomah; Mark Japinga; Nitzan Arad; Christina Bush; Frank McStay; Robert Saunders
July 2023
The cost of medications continues to rise, spurred in part by the introduction of new and costly drug therapies.
These increased costs have caused policymakers, public payers (i.e., Medicare and Medicaid), and commercial health insurers to closely examine the results achieved by such therapies and consider the growing disparities in drug access and outcomes.
The Inflation Reduction Act (IRA) — passed last summer — included provisions to introduce drug price negotiations in Medicare.
Policymakers also have proposed other policies, including patent reforms, international reference pricing, and out-of-pocket spending caps.
One other potential vehicle for improving access to and benefit from pharmaceutical drugs is using value-based payment (VBP) models, which tie payment for delivery of health services to outcomes on cost, quality, and equity of care.

Promise of VBP Models to Encourage Appropriate and Equitable Use of Drugs
VBP models can change how health care is paid for, with the goal of delivering high-quality, efficient health care aimed at treating the whole person.
These payment models began to spread widely in 2010; evidence to date demonstrates modest cost savings and quality improvements.
The Centers for Medicare and Medicaid Services (CMS) has set the ambitious goal of having all Medicare beneficiaries served by VBP models by 2030.
Incorporating drugs may help unlock the full potential of VBP models, ensure the right drug is used for the right patient at the right time, and expand access to drugs for underserved populations.
Integrating medication-related quality measures into VBP models could encourage high-value prescribing practices and provide incentives to providers based on use of the most efficacious treatment and improved drug utilization and health outcomes.

Barriers to Incorporating Drugs into VBPs
Most VBPs to date have not been designed to assess spending, utilization, and outcomes for drugs.
Indeed, drugs are often excluded from the total cost-of-care calculations that make up the “benchmark” — that is, the threshold amount that determines whether VBP participants have saved money.
Participants often achieve savings by reducing low-value care or avoidable hospitalizations.
In Medicare, only one VBP model (the Enhancing Oncology Model) has included all types of prescription drugs.
Commercial payers have similarly faced challenges incorporating drugs into VBPs.
This is because of several barriers to designing and implementing VBP models, which include:
- Disparate funding streams
- Limited data about drug costs and effectiveness available to prescribing clinicians
- Complexity in incorporating drugs into new payment approaches.
1.Disparate funding streams.
In traditional Medicare, there is a divide in the financing of benefits and services (i.e., Part A for hospital care, B for physician services and physician-administered drugs, and D for outpatient prescription drugs) that complicates the ability of Medicare to include prescription drugs and care in one VBP model.
CMS directly operates Parts A and B, but private plans handle the day-to-day administration of the Part D benefit (e.g., approving and paying for individual outpatient drugs).
This limits CMS’ ability to design all-encompassing VBP models in traditional Medicare.
Medicare Advantage and commercial plans, which do not face the same bifurcated financing and management of benefits, may be better able to operate models that capture all types of care and establish use-cases for future VBP initiatives in traditional Medicare.
2.Limited data about drug costs and effectiveness available to prescribing clinicians.
Clinicians often do not know what a patient may pay out of pocket for different drugs, given that insurance plans will differ in cost sharing for the same drug.
Moreover, clinicians frequently do not have information about how effective a drug will be for specific patients and conditions.
Without better information on price and effectiveness, clinicians have a limited ability to manage prescription drug spending and identify the most appropriate option for patients.
Clinicians often do not know what a patient may pay out of pocket for different drugs, given that insurance plans will differ in cost sharing for the same drug.
3.Complexity in incorporating drugs into new payment approaches.
In addition to clinicians lacking information about drug prices, factors like drug prices changing based on negotiations and changes in patients’ out-of-pocket costs can make it challenging to include drugs in payment models.
Further, VBP models typically use quality measures to ensure smarter spending and high-quality care, but there are few quality measures available to assess the appropriate use of pharmaceuticals or that follow the current evidence on the most efficacious drugs for patients with similar clinical indications and therapeutic goals.
Moreover,there is variation among pricing and payment programs and some approaches to drug payment may result in misalignment between provider financial incentives and goals to reduce total drug spending.
In short, health care organizations may be paid more in certain situations for prescribing more expensive drugs or a significant fraction of their revenue can be based on buying and using prescription drugs.
The overall effect limits how much clinician prescribing can be changed.

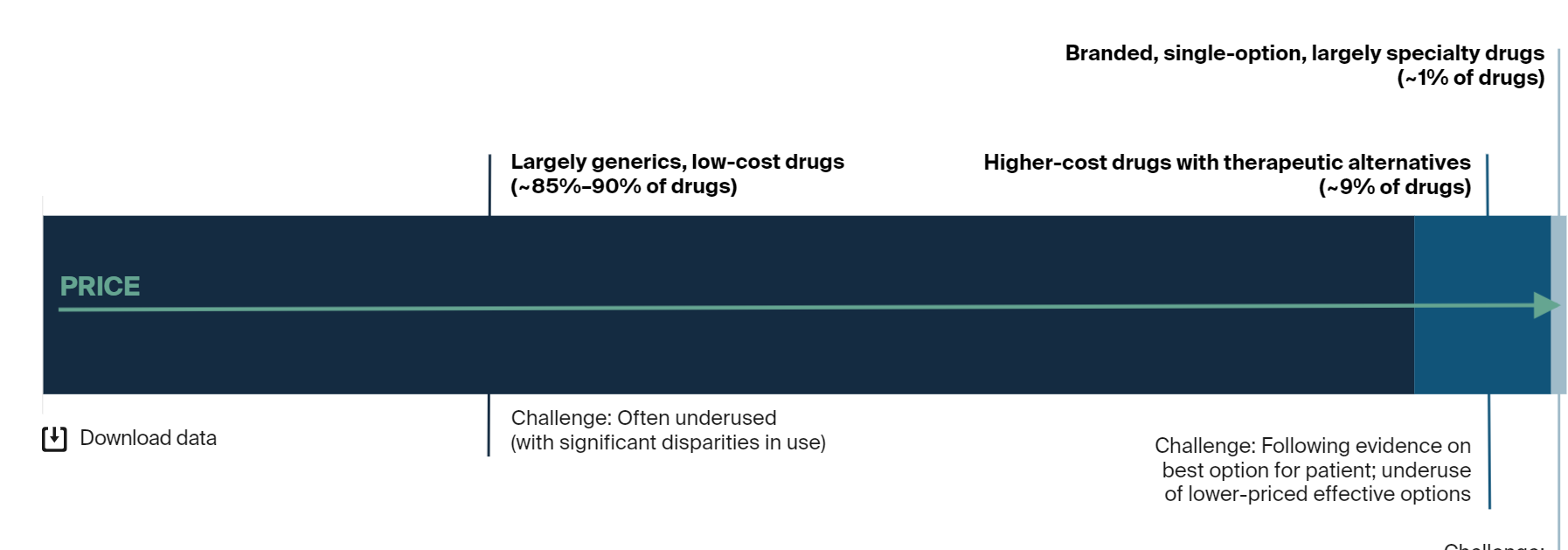
Tailoring VBP for Different Categories of Drugs
There are different challenges in different segments of the drug market. These include overuse and underuse, high prices, and limited evidence about what works.
Consequently, there is no single solution for all problems. VBP models can affect the utilization of drugs but have limited ability to affect prices.
There are several policies being implemented that focus on drug prices, such as direct negotiation as authorized in the Inflation Reduction Act, value-based contracts for specific drugs, or patent law changes.
However, overall spending depends on both utilization and price, so price policies alone do not ensure smarter drug spending.
VBP models could include quality measures that address
- underuse (e.g., utilizing low-cost, generic drugs for chronic condition management),
- provide incentives for appropriate use (e.g., identifying a lower-cost, equally effective alternative), and
- provide data that allows health care organizations to engage specialty clinicians about the drugs they are prescribing.
Challenges and Opportunities in Different Segments of the Drug Market
Conclusion
While a multitude of barriers have challenged drugs from being incorporated into care delivery VBPs, inclusion of drugs in the next iteration of accountable care models is an important goal given the critical role they play in health outcomes.
Total cost-of-care value-based payment models, such as those used in accountable care programs, may present the best opportunity to accomplish this through meaningful quality measures and enhanced data.
While the exact design elements must be tailored to different segments of the drug market, a spectrum of options should be explored by policymakers and commercial payers alike.
Originally published at https://www.commonwealthfund.org on July 12, 2023.
About the authors & affiliations
Kristen Ukeomah
Policy Research Assistant, Duke-Margolis Center for Health Policy at Duke University
Mark Japinga
Research Associate, Duke-Margolis Center for Health Policy at Duke University
Assistant Research Director for Biomedical Innovation, Duke-Margolis Center for Health Policy at Duke University
Policy Analyst with the Biomedical Innovation Team, Duke-Margolis Center for Health Policy at Duke University
Assistant Research Director, Duke-Margolis Center for Health Policy at Duke University
Robert Saunders
Senior Research Director, Health Care Transformation, Duke-Margolis Center for Health Policy at Duke University












