… this represented the first year-over-year increase in tuberculosis deaths since 2005
SmartHealth Blog
Joaquim Cardoso MSc (Chief Editor)
January 21, 2022
everydayhealth
*This is an synthesis of the publication below (Covid-19’s Devastating Effect on Tuberculosis Care — A Path to Recovery. N Engl J Med. 2022 Jan 5), with the title above, by the editor of the blog.
Synthesis *
Infographic
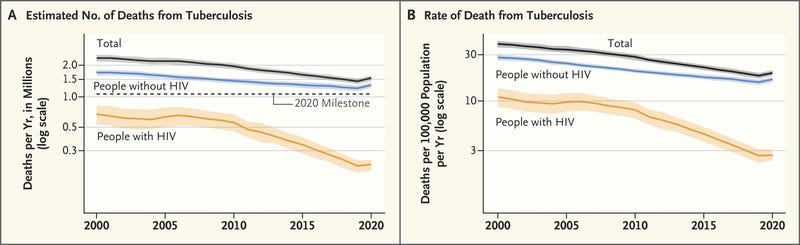
Global Trends in the Estimated Number of Tuberculosis Deaths and Tuberculosis Mortality, 2000 to 2020.
What is the problem?
- In 2020, there were roughly 1.5 million tuberculosis deaths worldwide, representing the first year-over-year increase in tuberculosis deaths since 2005 .2
- This decrease was concentrated in 16 countries, with Asian countries (especially India, Indonesia, the Philippines, and China) seeing the largest reductions in case reporting.2
- The WHO (where two of us work) estimates that nearly 10 million people developed tuberculosis in 2020.2
- Only 5.8 million cases were diagnosed and reported, however, which reflects an 18% decrease from 2019.
- Other negative pandemic-related effects include a 15% reduction in the number of people treated for drug-resistant tuberculosis, a 21% decrease in people receiving preventive treatment for tuberculosis infection,
- and a decrease (from $5.8 billion to $5.3 billion) in global tuberculosis spending between 2019 and 2020.2
What are the causes:
- The Covid-19 pandemic has had devastating effects on every aspect of global health, but tuberculosis services have been disproportionately affected
- Tuberculosis deaths have increased because of reduced access to care .2
What are the consequences?
- Given these setbacks, progress toward the 2022 targets established by the United Nations (UN) high-level meeting on tuberculosis is off track. Reductions in tuberculosis incidence have dramatically slowed.
- This trend is expected to worsen, driven by ongoing Covid-19 surges in low- and middle-income countries.2
What is the context?
- Nearly 20% of global tuberculosis incidence is attributable to undernutrition.2
- In 2020, the Covid-19 pandemic pushed 100 million people into poverty, and the UN estimates that developing economies will have pandemic-related losses of $12 trillion through 2025.
- In countries with high tuberculosis burdens, such as India, the population attributable fraction for undernutrition is higher — more than 50% in many Indian states3 — and malnutrition and poverty could be important tuberculosis drivers in coming years.
What are the solutions?
- Without an effective tuberculosis vaccine for adults, treatment is the primary form of disease control.
- New platforms such as mRNA and viral vectors that have proven successful for Covid-19 vaccines could be leveraged to develop tuberculosis vaccines, and clinical trials must be accelerated.
What are the recommendations ?
The path to recovery will require both immediate, short-term steps and longer-term actions.
- First, ending the Covid-19 pandemic quickly is critical for rebuilding tuberculosis services and other essential health services.
- Second, we need to highlight the worsening tuberculosis epidemic.
- Third, improving case detection is an urgent priority.
In the longer term, only by establishing multisectoral collaborations involving personal, societal, and health system interventions will we end the global tuberculosis epidemic by 2035.1
Another long-term strategy involves increasing investment in the development of new tuberculosis tools, taking advantage of the scientific advances that rapidly produced Covid-19 vaccines, diagnostics, and drugs.
Tuberculosis should be included in the pandemic preparedness and response agenda, which will probably be the focus of international government attention and increases in health spending moving forward.
What is the necessary funding?
- These efforts will require increased funding.;
- The century-old bacille Calmette–Guérin vaccine is still used for tuberculosis.
- Investments in new tuberculosis vaccines amount to barely $0.1 billion per year, and overall research and development investments reached only $0.9 billion in 2020, as compared with an estimated need of $2 billion.2
Conclusion
- The authors of the paper believe that world leaders should commit to vaccinating people globally to help end the Covid-19 pandemic.
- They should also reaffirm their commitment to ending the tuberculosis epidemic, work harder to mitigate the effects of the pandemic, and address the social, environmental, and economic determinants of tuberculosis infection and mortality.
ORIGINAL PUBLICATION
Covid-19’s Devastating Effect on Tuberculosis Care — A Path to Recovery
NEJM Group
Madhukar Pai, M.D., Ph.D., Tereza Kasaeva, M.D., Ph.D., and Soumya Swaminathan, M.D.
January 5, 2022
The Covid-19 pandemic has had devastating effects on every aspect of global health, but tuberculosis services have been disproportionately affected.1
According to the World Health Organization (WHO) Global Tuberculosis Report 2021, case notifications have plummeted because of pandemic-related disruptions in services.2
For the first time in more than a decade, tuberculosis mortality has increased.2
Even as high-income countries roll out Covid-19 vaccine boosters and stockpile millions of vaccine doses, many low- and middle-income countries are struggling to obtain vaccines.
Whereas 76% of people in high-income countries have received at least one Covid-19 vaccine dose, as of the end of December 2021, the rate was only 8% in low-income countries.
Because of vaccine inequity, new variants of SARS-CoV-2 (such as omicron) are emerging and particularly affect countries with low vaccine coverage and high rates of poverty and tuberculosis.
The WHO (where two of us work) estimates that nearly 10 million people developed tuberculosis in 2020.2
Only 5.8 million cases were diagnosed and reported, however, which reflects an 18% decrease from 2019.
The WHO … estimates that nearly 10 million people developed tuberculosis in 2020.
Only 5.8 million cases were diagnosed and reported, however, which reflects an 18% decrease from 2019.
This decrease was concentrated in 16 countries, with Asian countries (especially India, Indonesia, the Philippines, and China) seeing the largest reductions in case reporting.2
These countries all had major Covid-19 outbreaks and health care service disruptions.
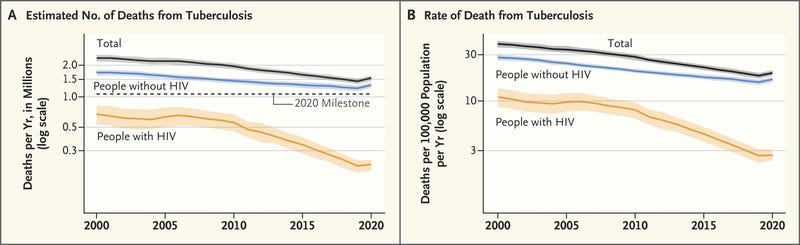
Global Trends in the Estimated Number of Tuberculosis Deaths and Tuberculosis Mortality, 2000 to 2020.
Tuberculosis deaths have increased because of reduced access to care.2
In 2020, there were roughly 1.5 million tuberculosis deaths worldwide, representing the first year-over-year increase in tuberculosis deaths since 2005 (see figure).2 Other negative pandemic-related effects include a 15% reduction in the number of people treated for drug-resistant tuberculosis, a 21% decrease in people receiving preventive treatment for tuberculosis infection, and a decrease (from $5.8 billion to $5.3 billion) in global tuberculosis spending between 2019 and 2020.2
Given these setbacks, progress toward the 2022 targets established by the United Nations (UN) high-level meeting on tuberculosis is off track. Reductions in tuberculosis incidence have dramatically slowed.
This trend is expected to worsen, driven by ongoing Covid-19 surges in low- and middle-income countries.2
India and Indonesia, for example, had delta-variant surges in 2021, with millions of excess deaths and severe disruptions to essential health services.
The emergence of the omicron variant poses a new threat, especially to countries in southern Africa that are experiencing massive Covid-19 surges on top of already high tuberculosis and HIV coinfection burdens.
This trend is expected to worsen, driven by ongoing Covid-19 surges in low- and middle-income countries
Without an effective tuberculosis vaccine for adults, treatment is the primary form of disease control.
Because so many tuberculosis cases have been missed during the past 2 years, increased transmission is expected. WHO modeling suggests that the pandemic’s effects on tuberculosis incidence and mortality in 2020 will be exacerbated in 2021 and beyond, in some cases throughout all 16 countries that were considered.2
These projections don’t account for exacerbations in the social determinants (extreme poverty and malnutrition, for example) that fuel the tuberculosis epidemic.
In 2020, the Covid-19 pandemic pushed 100 million people into poverty, and the UN estimates that developing economies will have pandemic-related losses of $12 trillion through 2025.
Nearly 20% of global tuberculosis incidence is attributable to undernutrition.2
In countries with high tuberculosis burdens, such as India, the population attributable fraction for undernutrition is higher — more than 50% in many Indian states3 — and malnutrition and poverty could be important tuberculosis drivers in coming years.
Nearly 20% of global tuberculosis incidence is attributable to undernutrition
The path to recovery
The path to recovery will require both immediate, short-term steps and longer-term actions.
- First, ending the Covid-19 pandemic quickly is critical for rebuilding tuberculosis services and other essential health services.
- Second, we need to highlight the worsening tuberculosis epidemic.
- Third, improving case detection is an urgent priority.
First, ending the Covid-19 pandemic quickly is critical for rebuilding tuberculosis services and other essential health services.
No country can keep new variants in check without high Covid-19 vaccine coverage. Without global vaccination, health care systems in low- and middle-income countries will collapse. We believe people working in the tuberculosis field should support the WHO plan — which was also included in the Group of 20 Rome leaders’ declaration — to vaccinate 70% of all countries’ populations by mid-2022. To achieve this goal, high-income countries will need to immediately redistribute surplus vaccine doses and meet their pledges to the Covid-19 Vaccines Global Access (COVAX) program. Waiving intellectual-property rights and sharing vaccine know-how is essential so that countries can produce their own vaccines. The WHO has created a multilateral mechanism to address regional inequities in vaccine manufacturing, with the first mRNA technology–transfer hub established in South Africa and spokes in many countries.
Second, we need to highlight the worsening tuberculosis epidemic.
Real-time Covid-19 dashboards are widely available, and governments respond immediately to new data. Tuberculosis programs can learn from this approach. Investments in digital data systems, connected diagnostics, and digital treatment-support tools could make tuberculosis data more visible and accessible. Communities could use these data to hold governments accountable and advocate for increased funding. During the pandemic, the WHO has published monthly tuberculosis-notification data and offered modeling estimates to guide countries’ recovery efforts. Such rapid reporting should become the new normal, and real-time tuberculosis data should be available everywhere.
Third, improving case detection is an urgent priority.4
Doing so will necessitate leveraging mobile-phone–based apps and digital tools to improve patient education, triage, and referrals and contact screening. Targeted active-case–finding initiatives, guided by precision public health (i.e., predictive analytics and mapping of hotspots), could help identify people with undiagnosed tuberculosis. This approach will require learning from Covid-19 testing experiences by bringing tuberculosis testing closer to where people live and work and engaging communities, private providers, and community-based health workers and civil-society organizations.4
Every country has scaled up its molecular-testing capacity for Covid-19, and this capacity could be used for tuberculosis testing, in combination with validation of simpler, nonsputum samples.
Better integration of tuberculosis and Covid-19 testing is also necessary. Because of the need to provide medical care during lockdowns, substantial advances have been made in digital health, remote service provision, ultra-portable digital x-ray systems with artificial-intelligence–based reading software, use of digital technologies for promoting medication adherence, and use of e-pharmacies in combination with home delivery of medicines.4 These systems could be leveraged for tuberculosis on a large scale, including scale-up of preventive therapy for tuberculosis.
In the longer term, only by establishing multisectoral collaborations involving personal, societal, and health system interventions will we end the global tuberculosis epidemic by 2035.1
Achieving this goal will require addressing the social determinants of tuberculosis infection and mortality; reducing stigma and other barriers to seeking care; promoting the use of masks, improved ventilation, and other airborne infection–control measures; and ensuring that health care workers have adequate personal protective equipment.
Another long-term strategy involves increasing investment in the development of new tuberculosis tools, taking advantage of the scientific advances that rapidly produced Covid-19 vaccines, diagnostics, and drugs.
Development of a simple, point-of-care tuberculosis test, an improved tuberculosis vaccine, and ultra-short drug regimens is critical.
Funding
These efforts will require increased funding.
Even as more than $100 billion has been invested in developing Covid-19 vaccines, leading to more than a dozen vaccines being authorized within 1 year after the WHO declaration of Covid-19 as a Public Health Emergency of International Concern, the century-old bacille Calmette–Guérin vaccine is still used for tuberculosis.
Investments in new tuberculosis vaccines amount to barely $0.1 billion per year, and overall research and development investments reached only $0.9 billion in 2020, as compared with an estimated need of $2 billion.2
New platforms such as mRNA and viral vectors that have proven successful for Covid-19 vaccines could be leveraged to develop tuberculosis vaccines, and clinical trials must be accelerated.
Investments in new tuberculosis vaccines amount to barely $0.1 billion per year, and overall research and development investments reached only $0.9 billion in 2020, as compared with an estimated need of $2 billion.2
Tuberculosis should be included in the pandemic preparedness and response agenda, which will probably be the focus of international government attention and increases in health spending moving forward.
Investments in social protection and universal health coverage would mitigate the Covid-19 pandemic’s effects and help avert the next crisis. Progress toward the UN’s Sustainable Development Goals (SDGs) would be beneficial for tuberculosis and other poverty-related diseases. Conversely, failure to achieve the SDGs’ tuberculosis-mortality target by 2030 would result in substantial health and economic losses.5
Conclusion
We believe world leaders should commit to vaccinating people globally to help end the Covid-19 pandemic.
They should also reaffirm their commitment to ending the tuberculosis epidemic, work harder to mitigate the effects of the pandemic, and address the social, environmental, and economic determinants of tuberculosis infection and mortality.
Author Affiliations
From the McGill International TB Centre and McGill School of Population and Global Health, McGill University, Montreal (M.P.); and the Global Tuberculosis Program (T.K.) and the Science Division (S.S.), World Health Organization, Geneva.
References (5)
See the original publication.
Originally published at https://www.nejm.org.