Some public-health researchers are embracing data and technology to target small groups with precise health interventions. Others fear that these tactics could fail millions.
Nature
Carrie Arnold
04 January 2022
A man has a nasal swab at a mobile COVID-19 testing site in Manhattan, New York City. Credit: Todd Heisler/The New York Times/Redux/eyevine
From their offices in a high-rise building in Queens, epidemiologist Sharon Greene and her colleagues watched the COVID-19 pandemic sweep through New York City in April 2020.
Using an open-source data-analytics program called SaTScan, her team mapped outbreaks as they unfolded across individual neighbourhoods, almost in real time.
This sophisticated approach relied on detailed data from hospitals and laboratories, and showed that the virus wasn’t affecting all New Yorkers equally.
That knowledge helped Greene’s team at the New York City Department of Health and Mental Hygiene to distribute testing resources and protective gear such as masks and gloves to the right places.
It was a different approach from New York City’s typical pandemic response plan, which advised largely blanket policies such as lockdowns and mass testing.
“Instead of just parking a testing van somewhere in an affected zip code, we can park it at an intersection in the middle of the cluster,” Greene says. “It’s hyper-local public health.” By the middle of the year, cases in the city began to drop.
The tech-centric, targeted approach used by Greene and other epidemiologists to address COVID-19 is part of a burgeoning field known as precision public health.
The concept is a modernization of the 150-year-old field of epidemiology, similar to how precision medicine has transformed health care, says Muin Khoury, director of the Office of Genomics and Precision Public Health at the US Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, and one of the idea’s biggest advocates.
The definition of precision public health is sprawling and variable: for most researchers in the field it includes a sweep of data-driven techniques, such as sequencing pathogens to detect outbreaks and turbo-charging data collection to monitor harmful environmental exposures. It also encompasses an ambition to target interventions to specific people who need them.
For Caitlin Allen, a PhD student of public health at Emory University in Atlanta, who organized a meeting on precision public health in October last year, the kernel of the idea is simple.
“You’re doing all the things you normally do in public health, but the unique aspect is that we’re using big data and predictive analytics to be more targeted and tailored in these efforts,” she says.
The concept promises to save money and lives by targeting interventions to the right people.
To Sandro Galea, an epidemiologist and dean of the Boston University School of Public Health, Massachusetts, and others, however, it sounds too good to be true.
“We’re all looking for the silver bullet, but there isn’t one,” says Galea.
The debate over the merits of precision public health has typically taken place in the pages of academic journals.
But funders are putting hundreds of millions of dollars behind precision-public-health initiatives, and some researchers worry about the implications for conventional public health.
Spending on public health is already sliding: although national health expenditure in the United States grew by 4.3% from 2008 to 2018, researchers found no change in public-health spending.
Galea is concerned that the precision approach is diverting attention away from regular public health.
“I worry that this is becoming the great sucking sound where we focus all our energy on technological approaches and we don’t focus on more foundational issues that will make a difference in the lives of millions,” Galea says.
Think local
For John Quackenbush, a biostatistician at the Harvard School of Public Health in Boston, the push for precision public health has existed since the birth of epidemiology.
In the 1850s, citizens of London stared down a different outbreak: cholera. The disease killed millions of people in the nineteenth century.
In 1854, a string of cases appeared in Soho, in central London. Physician John Snow worked just a few streets away. Snow went from door to door and began to plot cholera cases on a map. He found that people who got their water from a pump on Broad Street were much more likely to develop cholera.
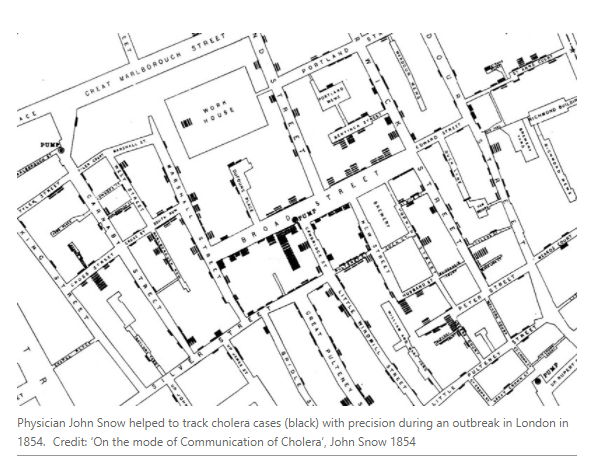
Snow’s statistics might seem pedestrian to modern epidemiologists, but they were state-of-the-art in 1854. If Snow had had access to SaTScan, he would have used that, Quackenbush says, and maybe brought the outbreak to a halt much more quickly.
“We just have access to unprecedented quantities of data,” Quackenbush says.
More than a century ago, the first municipal public-health departments in cities such as London and New York aimed to improve the health of large swathes of the population by building sewage systems, removing rubbish, purifying drinking water and collecting basic information on births and deaths.
The efforts were broad both because all residents would benefit from these interventions, and because early sanitation workers had little information on where to target their resources.
As time passed, epidemiology grew more sophisticated and precise as researchers were able to home in on specific clusters of disease and ever more detailed risk factors for future illnesses.
In that sense, the concept of precision public health is not new — but the phrase is recent.
Khoury coined it in a March 2015 blog post as he watched the genomics revolution take hold in medicine. He wanted to see that same energy spill over into public health.
To some extent, it already had. In 1996, the CDC launched PulseNet, which used DNA fingerprinting of bacteria that caused food poisoning to detect large, diffuse outbreaks across county and state lines. Large outbreaks of Salmonella, Listeria and Escherichia coli were investigated and halted when they might otherwise have gone unnoticed.
Khoury saw similar potential in other genetic technologies. As a paediatrician and geneticist, he had spent years studying a genetic condition called familial hypercholesterolaemia (FH), which causes extremely high cholesterol levels and can lead to heart attack and stroke.
Despite being readily recognized with basic screening tests and a proven therapy (high-dose statins) that reduces the risk of heart disease by 80%, many of those with FH go undiagnosed. With less than 1% of the population affected, public-health investments to screen everyone would be impractical and wasteful.
To Khoury and others, FH seemed like the perfect place for precision public health to shine. A US team is piloting a machine-learning method that scans health records (including standard blood cholesterol measurements) and identifies those likely to have FH. This strategy could help to ensure that individuals with FH get appropriate screening and treatment without wasting resources on the 99% of people without FH.
Soon after Khoury’s initial blog post, the term start popping up everywhere. In June 2016, the University of California, San Francisco, hosted the first precision-public-health conference. In the same year, the Zika virus swept across the Western Hemisphere. Health officials in Miami, Florida, began preparing for it to reach the United States.
Using a detailed geographic information system to map locally acquired cases, they were able to target mosquitoes with insecticides sprayed across just two blocks of Miami, rather than dousing whole neighbourhoods or even the entire city.

Precision approaches are taking off in many more guises.
The Bill & Melinda Gates Foundation has given a total of $271 million to the Child Health and Mortality Prevention Surveillance network led by Emory University to map out areas of greatest maternal-health problems and childhood malnutrition across Africa and Asia.
The goal is to help governments, charities and other advocates to create evidence-based policies to target childhood disease where it is most severe.
And in September 2019, the Rockefeller Foundation launched a $100-million Precision Public Health Initiative dedicated to using predictive analytics to prevent health threats, and exploiting big data to address the social factors that lead to poor health, such as discrimination and poverty.
During the pandemic, the foundation created an interactive dashboard, containing detailed statistics on various COVID-19 testing strategies, to help educators determine the safest way to reopen schools.
The idea seemed so promising that advocates began to wonder whether precision public health had any downsides. Its critics would find plenty.
Woolly definition
When you ask Galea what his problems are with precision public health, he laughs as if to say, “Where to start?”
His biggest complaint is that no one has defined exactly what precision public health is.
One common description is ‘the right intervention to the right population at the right time’. But critics say this isn’t any different from what John Snow did more than 150 years ago. Dubbing it ‘precision’ is at best extraneous and at worst deceptive, Galea says. “This is what public health does anyway.”
What makes precision public health problematic, he says, is that it focuses on new technologies instead of the bread-and-butter methods that have made the field so successful.
With decades of public-health funding cuts, Galea and his colleague Merlin Chowkwanyun at the Columbia University Mailman School of Public Health in New York City say they understand why epidemiologists and other professionals need to use snappy terms to secure even basic funding.
However, they worry that the seemingly subtle change to ‘precision’ approaches conceals a broader shift away from public health’s historical ideals of improving the well-being of even the most marginalized populations.
The core of public health, says David Taylor-Robinson, a health-equities scientist at the University of Liverpool, UK, is to improve the health of populations.
The ‘precision’ in precision public health, notes Taylor-Robinson, refers to individuals, not populations.
Improving the health of individuals is clinical medicine, not public health. In that sense, he says, “precision public health is an oxymoron”.
The danger of this contradiction is that it becomes easier to lose sight of the lower-tech, more challenging strategies that researchers know would improve people’s health, such as universal health care, welfare support and reducing income inequalities, according to Mira Vegter, a social scientist at Wageningen University in the Netherlands.
“We can be blinded by the data opportunities at the expense of some of the more dynamic social questions,” she says.
But in an emergency, there might not be time to rise to the challenge of addressing complex social questions. As the COVID-19 pandemic hit, some data-heavy techniques got the chance to prove their worth.
Hi-tech health
Even before the pandemic, many public-health departments, including New York City’s, had been honing real-time data analytics to trace infectious-disease outbreaks,.
As the coronavirus spread through New York, Greene’s goal was to focus on areas where transmission was growing faster than the citywide average. Over time, the work allowed her to begin making short-term predictions (called nowcasts) about future cases.
“It’s hard to shift resources around in real time,” Greene says. “If you can alert people earlier, they have more of a chance to protect themselves, and the more likely you are to prevent another infection.”
As well as tracking cases of COVID-19, epidemiologists around the world also began to track how the SARS-CoV-2 virus itself was spreading and changing, to help inform what measures were likely to be most effective.
Over the past 15 years, public-health laboratories around the world have been sequencing the genomes of infectious pathogens — which change slightly as they are passed between people — as a way to connect the dots on who was infecting whom.
It’s also how scientists noticed variants of SARS-CoV-2 emerging and spreading.
Several large databases of its genome sequences allow virologists to watch in near real time as coronavirus variants popped up and began to circulate.
“It’s like opening a window into a whole new world,” says Emma Thomson, a virologist at the University of Glasgow, UK. “You see so much more detail,” she says.
Pathogen sequencing in public health has been a clear success, even to those wary of precision methods.
“To not use these technologies strikes me as unambitious,” says Chowkwanyun. “I think there’s a way to marry this whizz-bang stuff with old-school public health.”
Galea agrees. But he also points out that the first wave of the pandemic overwhelmed New York City before it could scramble adequate resources to mount a defence.
Galea says that investments in basic public health, such as improving housing and requiring paid sick leave for workers, would have benefits during a pandemic — and ripple effects beyond.
Besides, says Thomson, pathogen sequencing and other techniques rely on the ability of public-health systems to step in and do something to stem the outbreak. “It’s great and it’s important but it has its limitations, especially when public-health departments are overwhelmed,” she says.
It’s easy to forget that access to basic health data, such as birth and death certificates and communicable-disease reporting, is the fuel that drives the public-health machine, says Angeline Ferdinand, a public-health researcher at the University of Melbourne, Australia.
Even basic data are lacking in some places, she points out — let alone the ability to perform whole-genome sequencing and the informaticians to put it to use. This could exacerbate inequalities both within and between countries.
Targeted treatment
For Allen and Khoury, however, there are many more ways in which new technologies and genomic information could pinpoint those most in need of help.
Take cancer, for example. Allen is piloting a project that analyses existing scans with machine learning to help identify individuals at high genetic risk of developing cancer, even if they don’t have a family history of the disease.
These people could benefit from more-intensive cancer screenings such as mammograms and colonoscopies. She recently completed a study that showed information collected by chatbots on medical websites could accurately predict whether a person met criteria for genetic testing for several cancers.
Whether or not researchers see a conflict between public health’s fundamental mission and its new ‘precision’ arm, both sides agree on one thing: public health will continue to be of utmost importance in the coming decades.
“The goal is to improve the health of the whole population, using all the tools that we have, whether we call them precision public health or not,” Khoury says.
Originally published at https://www.nature.com.