This is an excerpt of the publication below, with the title above, focusing on the topic in question.
Global Horizons for Value-Based Care: Lessons Learned from the Cleveland Clinic
NEJM Catalyst
Chibueze Okey Agba, MBA, Joshua Snowden-Bahr, JD, MHA, Kushal T. Kadakia, MSc, Samer Abi Chaker, MD, MPH, James B. Young, MD, and Alex G. Forystek
June 28, 2022
One page summary by:
Joaquim Cardoso MSc.
Health Transformation Institute
Continuous transformation for universal health
Value Based Care Unit
July 5, 2022
Summary
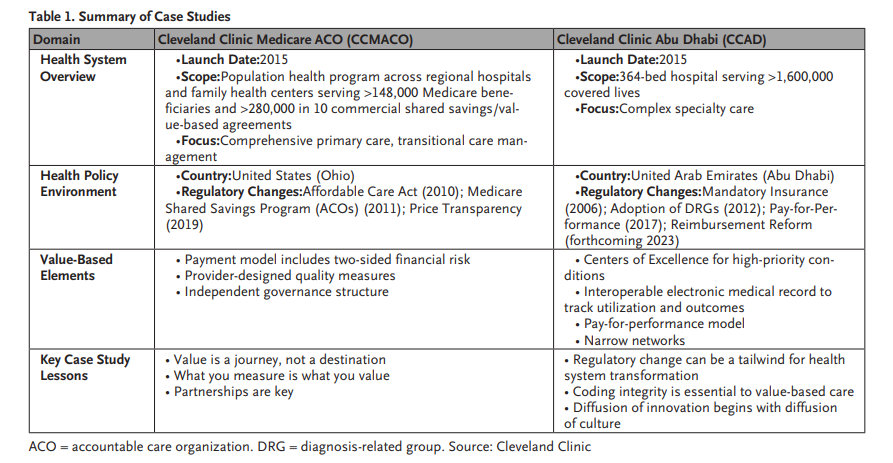
- The full version of this article reviews the Cleveland Clinic’s unique experience developing, operating, and refining value-based care models
(1) in the United States and
(2) The United Arab Emirates, with early applications and lessons learned
(3) in the United Kingdom,
… using these case studies to extrapolate challenges, successes, and opportunities for implementing global value-based care models. - This excerpt focuses on the “Case Study 1: Cleveland Clinic Medicare Accountable Care Organization (U.S.)”
ORIGINAL PUBLICATION (excerpt of full version)
Case Study 1: Cleveland Clinic Medicare Accountable Care Organization (U.S.)
Model Overview
Cleveland Clinic’s Medicare Accountable Care Organization (CCMACO) covers more than 148,000 beneficiaries in northeast Ohio.
Participating provider organizations include Cleveland Clinic’s main campus and regional hospitals, the Cleveland Clinic group practice, and independent primary care physicians affiliated with the Cleveland Clinic Quality Alliance.
Multidisciplinary care teams form the core of CCAMCO’s outpatient chronic disease management program, with these providers connected by investments in information technology (IT) and collaborative governance between patients, providers, and payers.
Evidence is lacking on how to design, implement, and sustain payer-provider partnerships in international markets, including infrastructure investments, operational changes, and contractual best practices.
Policy and Market Context
CCMACO Timeline
Cleveland Clinic joined MSSP in 2015. Because patient attribution for the ACO program occurs at the primary care physician level, Cleveland Clinic formed a separate legal entity to foster partnerships with independent primary care providers in Ohio.
The resulting entity, Cleveland Clinic Medicare ACO, LLC, also established governance structures designed to reflect CCMACO’s commitment to continuous improvement.
For example, the governing body includes a Medicare beneficiary to incorporate an active patient voice during decision-making.
Both independent and employed physicians serve as representatives on the Quality Committee and Financial Committee.
Operationally, CCMACO has developed a team-based model comprising primary care coordinators, population health medical assistants, transitional care management hub caregivers, pharmacists, and social workers.
This multidisciplinary approach, informed by the “team of teams” culture of Cleveland Clinic’s institute model, focuses on managing care transitions to reduce unnecessary utilization.
CCMACO initially only assumed upside risk under MSSP’s Track 1.
The program showed promise from the outset, achieving $42.2 million in savings (of which Cleveland Clinic kept 3%) and a quality score of 96.3% by 2016.
This foundation for value prepared Cleveland Clinic to transition to downside risk, entering Track 1+ in 2018.
Under this program, ACOs become eligible for shared savings up to 50% in exchange for a fixed loss sharing rate of 30%.
By 2020, the final quality score exceeded 98.1% with $9.56 million in savings.
Of this sum, 75% was distributed to ACO participants, 15% was invested in infrastructure, and 10% was invested in redesigned care processes and resources.
Lessons from CCMACO later informed the dissemination of value-based care principles to Cleveland Clinic Florida, which established its own ACO model in 2018 that currently encompasses nearly 36,000 beneficiaries in a one-sided risk model.
Cleveland Clinic Florida maintains select contracts with limited downside risk (AvMed and Florida Blue), and it will expand its ACO to downside risk once it further enhances its operating model and capabilities.

Challenges and Lessons Learned
- 1.Value is a journey, not a destination
- 2.What you measure is what you value
- 3.Partnerships are key.
1.Value is a journey, not a destination.
Cleveland Clinic already had many of the ingredients of value-based care: physician salaried employment model, integrated financial management platform, interoperable electronic medical records, culture of improvement, and ethos of innovation.
However, piecing together new payment and delivery models requires thoughtful planning and collaboration, and a willingness to challenge norms for how care is governed and delivered.
To this end, CCMACO convened different stakeholders to develop the governance models, legal arrangements, and care teams that would assume accountability for the ACO population.
CCMACO’s leadership also developed a phased approach for titrating financial risk from Track 1 to Track 1+, therefore transitioning from upside risk only to both upside and downside risk, to provide sufficient space for the model to achieve “wins” (that is, demonstrate shared savings) and make adjustments (e.g., new partnerships).
2.What you measure is what you value.
Well-designed performance measures provide valuable insight to providers and system leaders about areas for improvement and investment.
However, measures must be rooted in outcomes that matter to patients. Metric development should be a collaborative process accounting for both physician and patient perspectives.
CCMACO incorporated this principle into its contracting mechanism, creating a formal Quality Committee within the ACO legal entity that included both employed and independent physicians.
This cocreation process fostered accountability, while investment in enterprise analytics created mechanisms to track and measure performance.
To supplement the primarily process-based ACO quality measures, CCMACO invested in quantifying the patient experience through the use of rigorously designed patient surveys, the creation of an advanced patient registry, and focusing on patient experience through leadership rounding and continuous improvement projects led by a physician Chief Experience Officer.
Piecing together new payment and delivery models requires thoughtful planning and collaboration, and a willingness to challenge norms for how care is governed and delivered.
3.Partnerships are key.
Value is achieved, or lost, at the margins of care delivery: hospitalizations, procedures, discharges, follow-ups, and care transitions.
Team-based models and partnerships help to close gaps in the care continuum.
For example, CCMACO created a Transitional Care Management Hub, where caregivers focus on preventing readmissions by coordinating patient handoffs back to their primary care provider and collaborating with pharmacists to provide services such as medication reconciliation.
CCMACO also partnered with other care delivery organizations in the region.
We included independent primary care practices in the Cleveland Clinic Quality Alliance, and partnered with high-quality skilled nursing facilities to reduce length of inpatient stays.
We included independent primary care practices in the Cleveland Clinic Quality Alliance, and partnered with high-quality skilled nursing facilities to reduce length of inpatient stays.
The United States is not alone in trying to evolve more effective financial incentives for improving health care. The Cleveland Clinic describes the lessons it has learned from working with value-based care models in the U.S., the United Arab Emirates, and the United Kingdom.
About the authors and affiliations:
Chibueze Okey Agba, MBA
Chief Financial Officer, Hartford HealthCare, Hartford, Connecticut, USA
Joshua Daniel Snowden-Bahr, JD, MHA
Regional Director, Contracting & Business Development (International Markets), Market & Network Services, Cleveland Clinic Health System, Cleveland, Ohio, USA
Kushal T. Kadakia, MSc
MD Candidate, Harvard Medical School, Boston, Massachusetts, USA
Samer Abi Chaker, MD, MPH
Health Care Program Leader, CAPADEV LLP, Dubai, UAE
James B. Young, MD
Executive Director of Academic Affairs, Cleveland Clinic, Cleveland, Ohio, USA; Professor of Medicine & Vice Dean for Academic Affairs, Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, Ohio, USA
Alex G. Forystek
International Payer Contracts Manager, Cleveland Clinic, Cleveland, Ohio, USA
References and additional information
See original publication
Originally published at https://catalyst.nejm.org on June 28, 2022.
RELATED ARTICLES












