It is no coincidence that, like SARS before it, as well as multiple outbreaks of avian influenza, COVID-19 was initially associated with a live animal market.
This is a republication of the article below, with the title above, preceded by the Key Messages, by the editor of the blog.
COVID-19 — lessons for zoonotic disease
Science
EDWARD C. HOLMES
10 Mar 2022
A flying squirrel is for sale in a live animal market in Guangzhou, China, in 2004. Exposure to mammals in live animal markets and the fur trade could exacerbate the potential for virus spillover to humans.PHOTO: NIHARIKA KULKARNI/REUTERS
Executive Summary
by Joaquim Cardoso MSc.
Chief Editor of “The Health Strategy Blog”
@ The Pandemic Strategy Unit
March 13, 2022
What is the context?
- It is no coincidence that, like SARS before it, as well as multiple outbreaks of avian influenza, COVID-19 was initially associated with a live animal market.
- A core question in understanding the drivers of zoonotic emergence is whether particular animal groups are common sources of zoonotic viruses.
- A related question is whether the viruses that are most likely to emerge in humans can be identified.
How does the transmission occurs?
- Although viruses frequently jump species boundaries, there are a range of host genetic, immunological, ecological, and epidemiological barriers to successful cross-species transmission.
- Humans must come into contact with infected animals. This human–animal interface forms the central nexus for disease emergence, and modern human lifestyles mean exposure events will be increasingly commonplace.
- Compared to the highly infectious Delta and Omicron variants of SARS-CoV-2, the virus first detected in Wuhan in 2019 was far less efficient at human transmission, but still a good enough respiratory pathogen to spread rapidly in a dense, well-mixed, and fully susceptible population.
How might zoonotic diseases be prevented, or limited?
More intensive and effective surveillance at the animal–human interface is the simplest way to mitigate future pandemics.
- Such surveillance should be performed in those living and working at the human–animal interface, including in the wildlife trade and fur farming, and in animal production and slaughter, who work at live animal markets; in people who live near bat roosts; and even in those who work at animal rescue centers or in the veterinary profession (5).
There is little doubt that the wildlife trade and its high-risk end point — live animal markets — pose a danger for emerging zoonotic viruses.
- Recent metagenomic surveillance of the animal breeding facilities that supply these markets in China has identified a high diversity of host-jumping viruses, including novel coronaviruses and influenza viruses, sometimes in animals experiencing respiratory disease (2).
- By contrast, the large-scale surveillance of wildlife species in nature for potentially pandemic viruses does not seem feasible.
As physical distancing has been adopted to dampen the spread of COVID-19, to minimize morbidity and mortality, similar approaches should be deployed to better separate ourselves from wildlife.
- The wildlife trade and the live animal markets they supply must be strongly regulated and monitored, and effort should be devoted to establishing and maintaining suitable and sustainable environments for wildlife, including bats, located away from population centers.
It is imperative that some form of global “pandemic radar” is established in which information on sporadic zoonotic events to full-blown disease outbreaks is shared rapidly and freely (14).
- Such a radar can involve regular immunological surveillance, perhaps using approaches (15) adapted to recognize those groups of viruses, such as coronaviruses, that most often jump species boundaries, combined with ongoing metagenomic surveillance to detect active infections.
That humans live in a viral world with an increasingly porous human–animal interface makes future zoonotic outbreaks a reality that must be prepared for.
ORIGINAL PUBLICATION (full version)

COVID-19 — lessons for zoonotic disease
Science
EDWARD C. HOLMES
10 Mar 2022
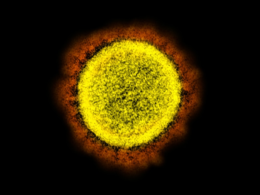
The COVID-19 pandemic is an unrelenting demonstration of the devastating impact of zoonotic disease, whereby viruses jump from animals to infect humans.
Although there is rightly an urgent focus on the development of vaccines and antivirals to limit the spread and severity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections, it is essential that this once-in-a-generation experience is used to determine the factors that drive zoonotic disease emergence and identify where gaps in our knowledge lie.
By understanding why and how zoonotic diseases emerge in humans, as well as the barriers to this process, it is possible to be better prepared to prevent pandemics like COVID-19 from happening again or at least respond more effectively.
Zoonotic diseases have been part of the human experience since the origin of our species.
In cases like SARS-CoV-2 or Ebola, the viral jumps from animals to humans occurred recently, whereas others, such as herpesviruses or papillomaviruses, likely occurred in our earliest ancestors.
The antiquity of zoonotic disease highlights the intimate relationship between human and animal viruses. The COVID-19 pandemic has led to considerable debate over the identity and role played by “reservoir hosts” (such as bats), “novel hosts” (like humans), and “intermediate hosts” (with suggestions including pangolins and raccoon dogs) that act as a conduit between the former two.
Although it is natural to place humans at the end of this chain of emergence, such an anthropocentric perspective is misleading.
In reality, viruses are ubiquitous components of global ecosystems that regularly move between interacting species, but usually do not result in overt disease (1).
Humans are also part of this viral ecosystem, and rather than being the end point of emergence, they can pass their viruses to other species (2).
Humans are also part of this viral ecosystem, and rather than being the end point of emergence, they can pass their viruses to other species
The key issue, then, is not that zoonotic diseases appear in humans, but that their emergence seems to be increasing in frequency (3).
Major changes in land use, increasing urbanization, and global connectedness are well documented as driving disease emergence through increasing human–animal contacts and accelerating transmission rates, and climate change will similarly accelerate the rate of zoonotic events.
Warming global temperatures will result in changing geographic distributions of wildlife as appropriate habitats shrink, perhaps leading to multispecies refugia that will increase the rate of cross-species virus transmission.
Those human populations that rely on the animal world will similarly find subsistence increasingly difficult and so may exploit previously pristine areas or change farming practices, increasing the risk of exposure to animal pathogens.
Unless these processes are limited now, with combating global climate change at the forefront, COVID-19 will only be an unsatisfying taste of what is to come.

A flying squirrel is for sale in a live animal market in Guangzhou, China, in 2004. Exposure to mammals in live animal markets and the fur trade could exacerbate the potential for virus spillover to humans.
A core question in understanding the drivers of zoonotic emergence is whether particular animal groups are common sources of zoonotic viruses.
If so, can this information be used to establish a watch-and-act list of those species most likely to carry potentially pandemic viruses?
It has long been known that most viral infections in humans have their ancestry in mammals (4).
Birds are the only other probable source of zoonotic diseases, with the various forms of avian influenza virus that occasionally appear in humans (such as H5 subtype viruses) presenting an ongoing pandemic threat.
Although viruses are often abundant in other animal groups (such as bony fish), their phylogenetic distance to humans greatly reduces the likelihood of successful cross-species transmission.
Within the mammals, a variety of groups have served as reservoirs for zoonotic viruses (3), particularly those with which humans share proximity, either as food sources (such as pigs) or because they have adapted to human lifestyles (like some species of rodent), as well as those that are so closely related to humans (such as nonhuman primates) that viruses face little adaptive challenge when establishing human-to-human transmission.
A core question in understanding the drivers of zoonotic emergence is whether particular animal groups are common sources of zoonotic viruses.
Most of all, since the emergence of SARS in late 2002, there has been intense interest in bats as virus reservoirs, although this may in part reflect biases in both ascertainment and confirmation (5).
Although bats seemingly tolerate a high diversity and abundance of viruses, the underlying immunological, physiological, and ecological reasons for this are not fully understood (6).
More pragmatically, the majority of bat viruses have not appeared in humans, and those that have emerged often do so through other host species (i.e., “intermediate hosts”) prior to successful emergence (7). Bats are important players in disease emergence, but they are only one component of the more complex global viral ecosystem.
A related question is whether the viruses that are most likely to emerge in humans can be identified.
Although metagenomic sequencing is revealing an increasingly large virosphere, with mammals carrying many thousands of different viruses, most of which remain undocumented (5), the greatest pandemic risk is posed by respiratory viruses because their fluid mode of (sometimes asymptomatic) transmission makes their control especially challenging.
Three groups of RNA viruses that regularly jump species boundaries best fit this risk profile: paramyxoviruses, influenza viruses, and, particularly, coronaviruses. Hendra and Nipah viruses, both with ultimate bat ancestry, are exemplars of paramyxoviruses that have emerged in humans.
Although neither have resulted in large-scale outbreaks, it is possible that more transmissible paramyxoviruses (such as the case of measles virus) lurk in the mammalian virosphere.
The documented host range of influenza viruses is growing, including recent reports of avian H9N2 influenza virus in diseased Asian badgers (2), but most human influenza virus pandemics have their roots in those viruses that circulate in waterbirds and poultry, often with the secondary involvement of pigs.
Fortunately, birds and humans are sufficiently different in most virus–cell interactions that avian viruses are usually unable to successfully transmit among humans.
A related question is whether the viruses that are most likely to emerge in humans can be identified.
By contrast, coronaviruses are commonly found in mammals that often exist at very high population densities, particularly bats and rodents, or that have strong connections with humans, such as pigs and dogs, and are appearing in humans with an increasing frequency (8).
SARS-CoV-2 has also highlighted the potential for “generalist” coronaviruses that can transmit in a wide range of mammalian species.
Notably, SARS-CoV-2 has been reported in such animals as cats, dogs, lions, tigers, mink (with transmission back to humans), and, most recently, white-tailed deer in the US, where the virus has jumped multiple times from humans, reaching high levels of prevalence in some populations (9).
Notably, SARS-CoV-2 has been reported in such animals as cats, dogs, lions, tigers, mink (with transmission back to humans), and, most recently, white-tailed deer in the US, where the virus has jumped multiple times from humans, reaching high levels of prevalence in some populations (9).
As sampling of wildlife continues, more SARS-CoV-2–like viruses will surely be identified in a broader range of species and their natural ecology revealed.
The viruses belonging to the evolutionary lineage containing SARS-CoV-2 — the sarbecoviruses — have a complex history of genomic recombination (10).
Does viral recombination elevate the risk of zoonotic emergence?
Recombination increases genetic diversity, generating virus variants that might, by chance, be better able to infect humans, although like most point mutations, most recombinants will reduce fitness.
There is also no overall association between the ability to recombine and the ability of zoonotic viruses to emerge in humans (11).
For example, of those viral groups perhaps most likely to cause the next pandemic, coronaviruses and influenza viruses recombine (or reassort) abundantly, whereas paramyxoviruses exhibit very low rates of recombination.
Although viruses frequently jump species boundaries, there are a range of host genetic, immunological, ecological, and epidemiological barriers to successful cross-species transmission.
Although viruses frequently jump species boundaries, there are a range of host genetic, immunological, ecological, and epidemiological barriers to successful cross-species transmission. Humans must come into contact with infected animals …
Humans must come into contact with infected animals. This human–animal interface forms the central nexus for disease emergence, and modern human lifestyles mean exposure events will be increasingly commonplace.
Following exposure, a virus must establish a productive infection, transmitting within the human population.
The barriers at this stage are likely substantial, especially as humans are exposed to many more viruses than lead to disease outbreaks.
This is apparent in the relatively high frequency with which people are exposed to animal coronaviruses (12), but the rarity of major outbreaks.
The intimate relationship between virus and host cell receptor acts as a major obstacle, and those animal viruses that by evolutionary chance can bind sufficiently well to human cell receptors will have an advantage in the game of emergence.
Modeling studies of receptor binding have revealed a myriad of mammalian species that could be productive hosts for SARS-CoV-2 (13), and a similar approach could be employed for other viral groups.
However, one important lesson from the ongoing evolution of SARS-CoV-2 is that those viruses that initially emerge do not necessarily need to be fully optimized for transmission to have a substantial impact.
Compared to the highly infectious Delta and Omicron variants of SARS-CoV-2, the virus first detected in Wuhan in 2019 was far less efficient at human transmission, but still a good enough respiratory pathogen to spread rapidly in a dense, well-mixed, and fully susceptible population.
Compared to the highly infectious Delta and Omicron variants of SARS-CoV-2, the virus first detected in Wuhan in 2019 was far less efficient at human transmission, but still a good enough respiratory pathogen to spread rapidly in a dense, well-mixed, and fully susceptible population.

How might zoonotic diseases be prevented, or limited? More intensive and effective surveillance at the animal–human interface is the simplest way to mitigate future pandemics.
Such surveillance should be performed in those living and working at the human–animal interface, including in the wildlife trade and fur farming, and in animal production and slaughter, who work at live animal markets; in people who live near bat roosts; and even in those who work at animal rescue centers or in the veterinary profession (5).
There is little doubt that the wildlife trade and its high-risk end point — live animal markets — pose a danger for emerging zoonotic viruses.
It is no coincidence that, like SARS before it, as well as multiple outbreaks of avian influenza, COVID-19 was initially associated with a live animal market.
Recent metagenomic surveillance of the animal breeding facilities that supply these markets in China has identified a high diversity of host-jumping viruses, including novel coronaviruses and influenza viruses, sometimes in animals experiencing respiratory disease (2).
By contrast, the large-scale surveillance of wildlife species in nature for potentially pandemic viruses does not seem feasible.
Wildlife harbor a large, diverse, and continually evolving pool of viruses, and determining whether they can infect human cells requires time-consuming and costly laboratory work.
It is no coincidence that, like SARS before it, as well as multiple outbreaks of avian influenza, COVID-19 was initially associated with a live animal market.
How might zoonotic diseases be prevented, or limited? More intensive and effective surveillance at the animal–human interface is the simplest way to mitigate future pandemics.
By contrast, the large-scale surveillance of wildlife species in nature for potentially pandemic viruses does not seem feasible.
As physical distancing has been adopted to dampen the spread of COVID-19, to minimize morbidity and mortality, similar approaches should be deployed to better separate ourselves from wildlife.
The wildlife trade and the live animal markets they supply must be strongly regulated and monitored, and effort should be devoted to establishing and maintaining suitable and sustainable environments for wildlife, including bats, located away from population centers.
It is imperative that some form of global “pandemic radar” is established in which information on sporadic zoonotic events to full-blown disease outbreaks is shared rapidly and freely (14).
Such a radar can involve regular immunological surveillance, perhaps using approaches (15) adapted to recognize those groups of viruses, such as coronaviruses, that most often jump species boundaries, combined with ongoing metagenomic surveillance to detect active infections.
That humans live in a viral world with an increasingly porous human–animal interface makes future zoonotic outbreaks a reality that must be prepared for.
As physical distancing has been adopted to dampen the spread of COVID-19, to minimize morbidity and mortality, similar approaches should be deployed to better separate ourselves from wildlife.
It is imperative that some form of global “pandemic radar” is established in which information on sporadic zoonotic events to full-blown disease outbreaks is shared rapidly and freely .
About the author
Professor Eddie Holmes is known for his work on the evolution and emergence of infectious diseases, particularly the mechanisms by which RNA viruses jump species boundaries to emerge in humans and other animals. He currently holds an ARC Australian Laureate Fellowship.
He is the author of 667 peer-reviewed papers and two books. His publications have >107,000 citations (h-index of 152, i10-index of 617; see http://scholar.google.com.au/citations?user=Syrp1IMAAAAJ&hl=en)
References and additional information
See the original publication