If people have access to primary care and referral systems, cancer can be detected early, treated effectively and cured.
Together, we can reverse the tide of cancer, avoiding 7 million unnecessary deaths by 2030.
WHO
André Ilbawi, Cherian Varghese
Executive WHO editors and writers
February 2020
Executive summary (excerpted from the full report)
Edited by Joaquim Cardoso MSc.
Chief Editor of The Cancer Strategy Institute
February 22, 2022
Cancer is a serious health problem in all populations, regardless of wealth or social status.
The global response to cancer has been uneven and inequitable.
Most low- and middle-income countries (LMIC) started later to address the cancer burden, having made hard choices to concentrate limited resources on an enormous burden of infectious diseases.
In 2020, when one in five people (20%) globally will face a cancer diagnosis during their lifetime and as gains against infections and other conditions have led to increased life expectancy, it is beyond time to accelerate global cancer control, through prevention, diagnosis, treatment and management, palliative care and surveillance.
Every year, effective cancer control is delayed, the response becomes more expensive, the preventable loss of life increases, and economic and human development remain stifed.
Whatever a country’s current stage of cancer control, the next steps can be informed by validated analytical tools, guiding principles, examples and global assistance.
This report introduces the principles, tools and current priorities in cancer control.
It also presents new evidence of the value of cancer control as an investment, with substantial human and economic returns.
The burden of noncommunicable diseases (NCDs) now outweighs the burden of infectious diseases in every country and will continue to grow over the coming decades.
The urgency of the NCD problem led to adoption of the Sustainable Development Goals (SDGs) and their target 3.4: “By 2030, reduce by one third premature mortality from NCD through prevention and treatment and promote mental health and well-being.” Universal health coverage (UHC) is a related SDG target (3.8).
The cancer control interventions described in this report can be melded into UHC benefit packages to drive progress in meeting both targets.
Let it be clear, without substantial — perhaps monumental — efforts in cancer control, these targets cannot be met.
1. Chapter 01. The Growing Burden of Cancer
2. Chapter 02. Cancer Control Is Effective
3. Chapter 03. Effective Primary Prevention
4. Chapter 04. Early Detection and Screening
5. Chapter 05. Cancer Management
6. Chapter 06. National Cancer Planning
7. Chapter 07. Financing Cancer Control
8. Chapter 08. Cancer Control Implementation, Together
1. Chapter 01. The Growing Burden of Cancer
In 2018, 18.1 million people around the world had cancer,
and 9.6 million died from the disease.
By 2040, those figures will nearly double, with the greatest increase in LMIC, where more than two thirds of the world’s cancers will occur.
There are more than 50 million cancer survivors currently alive.
Cancer is the cause of about 30% of all premature deaths from NCDs among adults aged 30–69.
The most frequently diagnosed cancer is
- lung cancer (11.6% of all cases), followed by
- female breast (11.6%) and
- colorectal cancers (10.2%).
The leading cause of death from cancer is
- Lung cancer (18.4% of all deaths), followed by
- colorectal (9.2%) and
- stomach cancers (8.2%).
The most common cancer type varies among countries, with certain cancers, such as cervical cancer and Kaposi sarcoma, much more common in countries at the lower end of the human development index (HDI) than in high-HDI countries.
Cancer mortality is a function of incidence and survival.
Inequity in access to effective treatment is mirrored in the much higher case fatality rates in lower HDI countries, a result of diagnosis at later stages and lack of treatment.
Progress in reducing the probability of premature deaths from cancer has been much greater in high-income countries (HIC), where there has been a 20% reduction from 2000 to 2015.
In low-income countries (LIC), the probability of premature mortality decreased by only 5% in that time period, refecting increasing global inequality.
Chapter 02. Cancer Control Is Effective
The spectrum of cancer control interventions includes primary prevention, screening and early diagnosis, multimodal treatment and survivorship and palliative care.
In each domain, highly effective interventions have reduced the cancer burden in countries where they are widely available and used by the population.
In countries with widespread access to the full range of effective measures — mainly higher HDI countries — cancer mortality rates have fallen and continue to do so.
The rate of death from cancer is rising in many countries at the lower end of the spectrum.
This can be changed by adoption of affordable, feasible national cancer control plans (NCCPs) for programmes to expand the services offered and financial and geographic access.
Cancer control is an integral component of the path towards UHC (Universal Health Coverage)
Key recommendation #1:
Activate political will,
strengthen governance and
make a cancer control plan founded on UHC.
By focusing on a set of priority interventions and investing effciently, more than 7 million lives can be saved by 2030, with major social and economic benefts.
The total required investment is
· US$ 2.70 per person in LIC,
· US$ 3.95 per person in LMIC and
· US$ 8.15 per person in upper to middle-income countries by 2030.
While these investments are ambitious, they are achievable and feasible. The key message is that cancer management is not prohibitively expensive.
Key recommendation #2:
Identify priorities that are feasible,
evidence based and can be financed
Chapter 03. Effective Primary Prevention
Globally, approximately one third to one half of all cancers could be prevented with current knowledge and technology.
Effective and feasible ways to prevent cancer are:
· With WHO “best buys” for NCDs as a guide,
· tobacco control through taxation and other policies and
· high coverage with vaccines to prevent infection with human papillomavirus (HPV) and hepatitis B virus.
Particular consideration should also be given to
· obesity,
· alcohol,
· occupational exposures and
· air pollution that are persistent or increasing major cancer risk factors.
Key recommendation #3:
Focus on WHO “best buys” for NCD primary prevention.
Chapter 04. Early Detection and Screening
Early diagnosis is the best alternative for the many cancers that cannot yet be prevented and those that occur despite prevention.
Currently, in most LMIC, cancer is diagnosed at an advanced stage, when treatment is generally less effective, more expensive and more disabling.
Two distinct approaches can be used to identify cancer early
· early diagnosis for symptomatic disease and
· screening of asymptomatic individuals in a target population.
Early diagnosis programmes are the priority.
They consist of
· raising awareness about cancer symptoms,
· ensuring the capacity for rapid clinical and pathological diagnosis and
· timely referral to a site where effective treatment can be given.
The priority in screening should be cervical cancer in all countries and
breast and colorectal cancer screening in well resourced countries.
There is significant inequity in the availability of high-quality pathology and diagnostic imaging, which are necessary for making an appropriate treatment plan.
Key recommendation #4:
Prioritize and invest in early diagnosis.

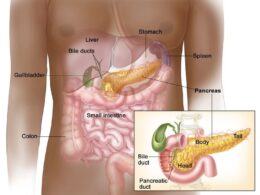
Chapter 05. Cancer Management
Cancer management is generally more complex than that for other diseases, even other NCDs.
Treatment can involve surgery, systemic therapy (e.g. chemotherapy, immunotherapy, endocrine therapy) and radiotherapy.
These diagnostic and therapeutic approaches should be delivered by a multidisciplinary team, which is the cornerstone of integrated, patient-centred care.
The past half century has seen tremendous progress in cancer treatment,
- mainly through advances in systemic therapy,
- more recently in immunotherapy,
- as well as refinements in radiotherapy and surgery.
For some common cancers — breast, cervix and colorectal cancers, leukaemias, most childhood cancers and others — curative treatment has existed for several decades and is affordable to countries at all income levels.
Decisions on the treatments to be selected will have to be made in NCCPs, according to impact, cost and feasibility.
While some recent innovative therapies can have meaningful survival or quality of life benefits for certain cancer patients, many of the newest treatments have only marginal population benefts over older ones.
WHO has defined priority interventions to help guide decisions on the choice of medicines and health products.
Key recommendation #5:
Implement effective, feasible cancer management interventions,
ensuring high-quality value-based care.
The aim of palliative care is to prevent and relieve suffering during all phases of serious health problems, including pain and suffering as a result of treatment, in both survivors and people who eventually die from cancer.
In cancer, the foremost (although not the only) target is pain control, which in most cases can be relieved by inexpensive oral morphine or other opioids.
These are unfortunately largely unavailable in much of the world, particularly in LMIC.
Some countries have, however, overcome political and regulatory barriers to provide adequate palliative care, including pain control and other services, demonstrating that it is feasible.
The World Health Assembly has called for universal access to palliative care as a necessary step towards UHC.
With more than 50 million cancer survivors currently alive, attention must be paid to their long-term health needs and reintegration into society and the workplace.
Key recommendation #5:
Palliative and survivorship care should be included in all NCCPs.
Chapter 06. National Cancer Planning
Ideally, a national cancer plan starts with the collection and analysis of data on the disease burden, the prevalence of risk factors and current capacity and system performance.
In view of the multisectoral, multimodal nature of cancer control, planning is essential to synchronize the delivery of services and to work towards realistic milestones.
Even in the absence of complete data, cancer plans can define the appropriate steps for advancing cancer control.
Short- and medium-term capacity development is necessary to extend services and achieve full population coverage for effective interventions.
WHO and others can provide guidance to countries in planning and selecting interventions that are effective and cost-effective and information for budgetary analyses.
Cancer planning should be led by a designated responsible government directorate, working with all relevant stakeholders, including knowledgeable members of the public and professionals.
Sustainable success will require commitment to regular reviews of progress and revision of the plan, increasing investment in information systems, strengthening governance structures and, because cancer services are currently less well funded than other disease programmes in many LMIC, ensuring a continual, appropriate increase in the share of the health budget.
Key recommendation #6:
Strengthen information systems to improve planning and accountability
Chapter 07. Financing Cancer Control
Funding of cancer control with capital investments and funding of services with the best value for the greatest good ensure equitable fnancial and geographical access to high-quality cancer services.
A WHO and international Agency for Research on Cancer (IARC) tool for setting priorities and costing cancer control plans is available for costing cancer services, which can be used to model fnancial projections with both domestic and external funding.
In general, payment for direct patient services under UHC is a government responsibility.
Where resources are limited, there has been minimal external aid for NCDs, particularly cancer; however, there are many private-sector initiatives in some countries for certain types of cancer (e.g. childhood cancer) that provide resources for capacity-building, training and capital investments.
In countries in which cancer control has lagged, cancer control planning can include sources of financing for the necessary investments.
Financing for both services and population coverage should be extended in steps, in line with the national cancer plan and with the principle of progressive realization of UHC.
Country experience indicates that this is best achieved in a system of pre-paid, centrally disbursed funding.
Key recommendation #7:
Fund priorities in cancer interventions, and ensure fnancial protection
Chapter 08. Cancer Control Implementation, Together
Cancer control is implemented by ensuring that all the necessary facilities, equipment, personnel, information systems and fnancing are in place to deliver the cancer plan.
A radiotherapy unit is of no use without trained professionals in several categories (e.g. medical physicists), specialized maintenance personnel and record-keepers, as well as laboratory and imaging services to evaluate progress.
If one link in the chain is missing, the patient suffers, and resources are wasted.
Similarly, a screening programme for breast cancer will have no impact unless the technology necessary for diagnostic and treatment is available.
Cancer centres are important hubs for increasing capability, strengthening standards and increasing efficiency.
Key recommendation #8:
Build capacity through cancer centres and networks linked to strong primary care.
The most pressing needs, particularly in LMIC, are training a cancer workforce and ensuring the basic infrastructure for cancer (only some of which is shared with that for other medical conditions).
Global collaboration is a necessity for some countries, including training in other countries and collaborating with national, international and private-sector organizations.
Implementation also involves working within the assigned budget for infrastructure and staff and procuring the necessary commodities.
One of the greatest global threats to the solvency of cancer control is the cost of cancer medicines and products. In this area, regional and global cooperation can improve access, as individual countries and particularly small markets have little leverage.
Key recommendation #9:
Optimize the workforce and access to reliable, sustainable medicines and other products.
An overriding concern in cancer control is maintaining high quality. Cancer is less forgiving of lapses in quality than many other diseases.
Delays in access to diagnosis and treatment, substandard cancer medicines, poor control of radiotherapy can all lead to unnecessary suffering, deaths and wasted resources.
Implementation requires good working relationships among government departments, with the medical and business communities and globally with international and national organizations.
Internally, a coalition of stakeholders should be involved in preparing the national cancer plan.
Governments are responsible for setting policy and creating an enabling environment through laws and regulation, but they rely on partners with real responsibilities for aspects of implementation.
It is only together that we can achieve progress in cancer and provide care for all.
Key recommendation #10:
Engage communities and civil society to achieve cancer control together.
Foreword
Tedros Adhanom Ghebreyesus
Director-General World Health Organization
Cancer is a deeply personal disease. It affects all of us — including me. We all have friends and family who have lived and sometimes died with this horrible disease. Cancer exerts a tremendous physical, emotional and fnancial strain on individuals, families, communities, health systems, and countries.
Nearly every country has seen an increase in cancer cases over the past decade, and over the next 20 years, cancer rates are projected to rise by at least 60%.
Many low- and middle-income countries already have large numbers of cancer patients who do not have access to timely, quality diagnosis and comprehensive treatment. In 2019, more than 90% of high-income countries reported that treatment services for cancer were available in the public health system, compared to less than 15% of lowincome countries, where survival is unacceptably low.
Countries passed a resolution at the World Health Assembly in 2017 committing themselves to cancer prevention and control through an integrated approach, and asking WHO to provide guidance. Now is the time to convert political commitments into action. In 2018 WHO launched an initiative to save the lives of millions of children from cancer, and in 2019 we prequalifed a biosimilar medicine for the frst time, trastuzumab, paving the way for more women to have access to one of the most effective but most expensive breast cancer treatments. In 2020 WHO will present countries with a global strategy towards the elimination of cervical cancer, which kills one woman every two minutes, but is largely preventable.
My hope and expectation is that this report will help countries to set priorities for investing in cancer control and universal health coverage. This report builds on the science and evidence from the International Agency for Research on Cancer’s World Cancer Report.
WHO does not work alone. Controlling cancer will require governments to prioritize investments and implement policies to address risk factors; countries to have trained health workers and medicines; civil society to take a lead in mobilizing communities; development partners and donors to make strategic investments; individuals to make healthy choices; and industry to promote access and innovation.
Recent decades have seen rapid innovation in cancer diagnosis and treatment. Yet the distribution and uptake of these services, medicines and technologies have been profoundly inequitable and ineffcient. Being diagnosed with cancer shouldn’t be a death sentence because you do not have access to health care or the means to pay for it.
If people have access to primary care and referral systems, cancer can be detected early, treated effectively and cured.
Careful evidence-based investments in cancer interventions will deliver meaningful social and economic returns, with increased productivity and equity.
Together, we can reverse the tide of cancer, avoiding 7 million unnecessary deaths by 2030.
If people have access to primary care and referral systems, cancer can be detected early, treated effectively and cured.
Together, we can reverse the tide of cancer, avoiding 7 million unnecessary deaths by 2030.
Originally published at https://www.who.int